Translate this page into:
Neurological Predictors of Functional Outcome in Cortical Venous Sinus Thrombosis
Paul Birinder Singh, DM Dayanand Medical College and Hospital Ludhiana 141001, Punjab India drbirinder06@yahoo.co.in
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Objectives Cerebral venous sinus thrombosis (CVST) has a wide clinical spectrum. Despite favorable prognosis, identifying CVST patients with a possible poor functional outcome can be challenging. This study aims to establish the neurological predictors of outcome in CVST.
Materials and Methods We analyzed 70 patients of CVST and categorized them into three groups: Group I with isolated intracranial hypertension; Group II—focal syndrome of neurological deficit; Group III—subacute encephalopathy. Demographic, disease characteristics, and radiological parameters were also analyzed for prediction of hospital course. Functional outcome was assessed by modified Rankin scale (mRS) dichotomized as good (mRS: 0–2) or poor outcome (mRS ≥ 3).
Statistical Analysis Univariate and multivariate logistic regression analyses were performed to find out the independent effects of prognostic factors to be used for outcome prediction.
Results The mean age was 36.71 ± 14.9 years with 40 (68.8%) males. Most common presenting complaints were headache 35 (50%), hemiparesis 14 (20%), and seizures 12 (17.4%). Group I included 44 (62.9%), group II 17 (24.3%) and group III 12 (12.9%) patients. During hospitalization 28 (40%) patients needed intensive care unit (ICU) care, among them 7 (10%) required ventilation. There were eight times more chances of ICU care (odds ratio [OR]: 7.4; 2.5–24.4) and 23 times more need for ventilation (OR: 23; 2.5–88.9) whenever patients were in group II or III. Good outcome (mRS < 2) was noted in 52 (74.2%) patients. Headache was associated with good functional outcome, whereas hemiparesis with poor outcome. Neurological grouping was the independent predictor of functional outcome; patients with focal neurological deficit (group II) were 20 times more likely to have dependent life at the time of discharge (p < 0.05) with the mortality rate of 2.9%.
Conclusions Neurological grouping is a practical tool for prediction of function outcomes. Early anticipation of prognosis helps in decision-making in the clinical practice.
Keywords
cerebral venous sinus thrombosis
mRS
neurological groups
outcome
predictor
Key Message
This study aids the clinicians in identifying the pattern of neurological deficit which can not only foretell hospital course of patients with cortical venous sinus thrombosis, which is a complex neurological entity with a heterogeneous clinical course, but also reveal the functional outcome.
Introduction
Cerebral venous sinus thrombosis (CVST) is an important cause of cerebrovascular accident involving cerebral veins and sinuses. It affects about 5 people per million and accounts for 0.5% of all strokes.1
CVST poses a diagnostic as well as a therapeutic challenge to the clinicians because of diversity in clinical symptoms, mode of onset, and neuroimaging signs.2 Literature suggests that acute CVST contributes to significant morbidity and mortality with dependency rate of 15 to 25% and mortality rate of 4%. Clinical characteristics at admission, which included depressed consciousness, mental status disorder, and low Glasgow Coma Scale (GCS), were regarded as predictors for poor prognosis at 30 days.3 However, individual prognosis is difficult to predict using the aforementioned clinical signs as they may be confounded by the presence of seizures or antiepileptic drug usage. This shows that there are some variables, which are related to outcome as epiphenomena and run in parallel with other true independent predictors. Realizing this void in the assessment of mental status or consciousness in patients with respect to the functional outcome, it would be interesting to note if any specific neurological deficits at the time of diagnosis which when recognized would affect the outcome of patients with CVST. Neurological deficits represent ongoing neuronal loss, which is an important factor in predicting the course of CVST. We planned this prospective observational study in patients with CVST to fill this void in the literature and establish neurological predictors for poor outcomes in such patients.
Materials and Methods
Ethics
The study was conducted with approval of institutional Ethics Committee (BFUHS/2K18p-TH/14222) and informed consent was taken from all adult participants.
Study Design
All consecutive patients with the diagnosis of cortical venous sinus thrombosis (CVST) with age >18 years admitted in the ward or emergency of neurology department of a tertiary care teaching hospital over the course of 3 years were enrolled in the study. The diagnosis of CVST was established clinically and confirmed by MRI (magnetic resonance imaging) brain (T1, T2, T2* gradient echo, susceptibility-weighted images, FLAIR [fluid-attenuated inversion-recovery] and DWI [diffusion-weighted imaging] sequences) with contrast venography.4 An experienced radiologist analyzed all images regarding the location of thrombus, anatomical categorization of involved sinuses, and number of sinuses involved.
Arterial territory stroke, transient ischemic attack, subarachnoid hemorrhage, intracranial bleed, and intracranial tumors were excluded from the study.
The data regarding demographic profile and baseline characteristics including age, gender, comorbidities, laboratory parameters, and radiological features were collected and analyzed. The clinical features including presenting neurological symptoms and detailed neurological examination, GCS, and modified Rankin scale (mRS) were also entered in the prestructured performa. We performed a literature search regarding neurological features and presenting clinical symptoms in patients with CVST.5 6 7 According to the literature review, all patients of CVST included in the study were categorized into three groups based on the presence of neurological signs and symptoms.
Group I included patients with isolated intracranial hypertension as diagnosed by presence of papilledema irrespective of vision loss.
Group II included focal syndrome of neurological deficit such as motor weakness, sensory deficits, cortical blindness, aphasia, and apraxia with or without any combination of cranial nerve palsy with preserved consciousness.
Group III included patients having subacute encephalopathy (defined as altered consciousness, mentation, disorientation, or confusion state) with focal neurological signs.8 Encephalopathy was not explained by any other metabolic cause.
Primary outcome of the study was functional outcome (dependency), which was evaluated using mRS dichotomized as good outcome (mRS: 0–2) or poor outcome (mRS > 2) at the time of discharge.
Secondary outcome parameters of the study were duration of intensive care unit (ICU) stay (days) and need for mechanical ventilation (as per the standard protocol of the hospital).
Statistical Analysis
The data concerning the presenting neurological features and outcome of the subjects were compiled and analyzed by using appropriate statistical methods. The Chi-square test wherever appropriate was performed to analyze the univariate relations between possible prognostic factors and outcome at the time of discharge. As it is likely that different prognostic factors are mutually related, the independent effects of prognostic factors were additionally analyzed with multivariate logistic regression. A probability value (p-value) less than 0.05 was considered statistically significant. All statistical calculations were done using SPSS (Statistical Package for the Social Science) 21 version statistical program for Microsoft Windows.
Results
We prospectively analyzed 70 patients of CVST during the 3-year period. Among them, 40 (68.5%) were males and 22 (31.5%) females. The mean age of patients was 36.71 ± 14.93 years. The majority of patients (n = 38; 54.3%) were in the age group of 21 to 40 years followed by 25 (35.7%) patients in the age group above 40 years, and associated comorbid conditions were noted in 8 (11.4%) patients with CVST. The common presenting complaints noted in our cohort in a decreasing order of frequency were headache in 35 (50%) patients, hemiparesis in 14 (20%), and seizures in 12 (17.14%) patients. The demographic factors, presenting clinical features, and venous sinuses involved (radiological characteristics) of all CVST patients are summarized in Table 1.
|
Characteristics, N = 70 |
|
|---|---|
|
Mean age (range) |
36 ± 14.93 (18–58 years) |
|
Gender |
|
|
Male |
40 (68.8%) |
|
Female |
22 (31.5%) |
|
Presenting neurological deficit |
|
|
Headache |
35 (50%) |
|
Hemiparesis |
14 (20%) |
|
Seizure |
12 (17.1%) |
|
Encephalopathy |
9 (12.9%) |
|
Radiological parameters |
|
|
Deep |
16 (22.9%) |
|
Superficial |
34 (48.5%) |
|
Both |
20 (28.6%) |
|
One sinus |
50 (71.4%) |
|
Two sinuses |
17(24.3%) |
|
Multiple sinuses |
3 (4.3%) |
|
Comorbid condition |
|
|
DM |
2 (2.9%) |
|
HTN |
6 (8.5%) |
|
Neurological syndrome |
|
|
Group I |
44 (62.9%) |
|
Group II |
17 (24.3%) |
|
Group III |
9 (12.9%) |
Abbreviations: CVST, cerebral venous sinus thrombosis; DM, diabetes mellitus; HTN, hypertension.
Among patients with CVST, 44 (62.9%) presented with isolated increased intracranial pressure (group I), while 17 (24.3%) presented with focal neurological deficits (group II), and encephalopathy was the presenting neurological symptom (group III) in nine (12.8%) patients. There was no statistical difference in age, gender, and sinus involvement between three neurological groups of CVST patients. Group II and III had higher odds of ICU requirement (odds ratio [OR]: 7.4; 2.5–24.4) and mechanical ventilation (OR: 23; 2.5–88.9). In this study, 52 (74.2%) patients had good outcome (mRS < 2), while 18 (22.9%) had poor outcome with mortality rate of 2.9% (n = 2). During their hospital course, 28 (40%) patients needed ICU admission and among them 7 (10%) required mechanical ventilation for deteriorating clinical condition.
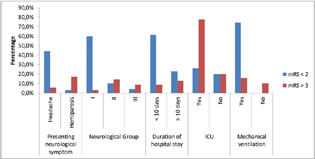
On univariate analysis there was significant association of presenting neurological complaint with functional outcome; headache was associated with good functional outcome (mRS ≤ 2) while hemiparesis with poor outcome. In addition, patients of group II and III, requiring longer duration of stay (>10 days) or need for mechanical ventilation, were the predictors of dependency (mRS > 2; Table 2). On multivariate regression analysis, neurological categorization II and III were the strongest independent predictor for poor outcome (mRS > 2) in CVST (Fig. 1). In our cohort, there was no effect of age, gender, anatomical site, or type of venous sinus thrombosis on the functional outcome of patients with CVST.
|
Clinical characteristics |
Functional outcome |
Chi square |
p-Value |
||
|---|---|---|---|---|---|
|
mRS ≤ 2 |
mRS > 3 |
||||
|
Age |
36.24 ± 14.24 |
38.68 ± 16.84 |
2.473 |
0.290 |
|
|
Gender |
Male |
37 (52%) |
11 (15.7%) |
0.626 |
0.429 |
|
Female |
15 (21.4%) |
7 (10%) |
|||
|
Sinus thrombosed |
Deep |
14 (20%) |
7 (10%) |
3.438 |
0.179 |
|
Superficial |
22 (31.4%) |
9 (12.8%) |
|||
|
Both |
16 (22.8%) |
2 (2.9%) |
|||
|
Presenting neurological symptom |
Headache |
31 (44.2%) |
4 (5.7%) |
10.110 |
0.001 |
|
Hemiparesis |
2 (2.8%) |
12 (17.1) |
29.45 |
0.000 |
|
|
Seizure |
11 (15.7%) |
2 (2.9%) |
0.214 |
0.214 |
|
|
Neurological group |
I |
42 (60%) |
2 (2.9%) |
47.007 |
0.000 |
|
II |
7 (10%) |
10 (14.3%) |
|||
|
III |
3 (4.2%) |
6 (8.6%) |
|||
|
Duration of hospital stay |
≤10 days |
43 (61.4%) |
6 (8.6%) |
15.513 |
0.000 |
|
>10 days |
16 (22.8%) |
9 (12.8%) |
|||
|
ICU admission |
Yes |
38 (26%) |
4 (77.8%) |
14.409 |
0.000 |
|
No |
14 (20%) |
14 (20%) |
|||
|
Mechanical ventilation |
Yes |
52 (74.2%) |
11 (15.7%) |
22.469 |
0.000 |
|
No |
0 |
7 (10%) |
|||
Abbreviations: ICU, intensive care unit; mRS, modified Rankin scale.
Note: Statistically significant p-values are indicated in bold.
-
Fig. 1 The graph shows independent predictors of functional outcome in CVST patients. CVST, cerebral venous sinus thrombosis; ICU, intensive care unit; mRS, modified Rankin scale.
Fig. 1 The graph shows independent predictors of functional outcome in CVST patients. CVST, cerebral venous sinus thrombosis; ICU, intensive care unit; mRS, modified Rankin scale.
Discussion
Cranial venous sinuses thrombosis is a distinct cerebrovascular disorder having heterogeneous clinical course with unfavorable outcome noted in 25 to 30% of patients. Predictors of clinical outcome depend upon the venous thrombotic occlusive process. Occlusion of cerebral veins leads to venous infarction and brain swelling resulting in neuronal damage and hemorrhage. This presents as focal neurological deficits and if parenchymal lesions are extensive there are severe neurological manifestations with higher chances of dependency. While on the other extreme, occlusion of sinus thrombosis may lead to development of isolated increase in intracranial pressure due to impaired absorption of cerebrospinal fluid with no parenchymal involvement, which results in good functional outcome. Hence, patients with acute CVST present with varying pattern of neurological signs, depending on the number and site of venous sinuses involved. Hence the categorization of patients on the basis of neurological spectrum of clinical manifestations will have better predictive value rather than assessment of individual clinical signs. Although GCS, seizure, and consciousness level have been shown to influence outcomes, but these represent epiphenomena and have confounding effect on each other, questioning the true predictive value of the subjective neurological signs.9 Hence in this study we aimed to identify the pattern or group of neurological signs that would help physicians in predicting hospital course as well as functional outcome in patients with acute CVST.
In this study, functional dependency rate was 25.8% (mRS ≥ 3) at the time of discharge with case fatality rate of 2.9%.
Liang et al showed functional dependence (mRS: 0–2) rate of 70.5% in a cohort of 44 patients of CSVT.10 This variation in the functional outcome might be related to the study design though both studies assessed the short-term functional outcome at the time of discharge. Age, gender, anatomical involvement of sinus, superficial or deep, and number of sinus thrombosis did not show any correlation with the outcome of CVST patients. However, a previous study by Ferro et al showed that older age and male gender were associated with poor outcome.11 This study included comparatively younger patients having mean age of 36 ± 14.93 years, which may be the reason for this disparity between the two studies.
Headache was a significant predictor of good outcome (p = 0.001) that had not been reported previously. Headache is the most common symptom of CVST12 13 as seen in this study. As group I included patients with isolated intracranial hypertension, hence headache was found in all patients and was actually the reason for it to be associated with good outcome. On the other hand, presence of focal neurological deficit and hemiparesis on univariate analysis showed a negative predictive value for the outcome signifying that significant neurological loss had already set in at the time of diagnosis before the start of treatment.14 15 Neurological grouping in addition was also a significant independent predictor (p = 0.000) of outcome and hospital course in patients with CVST. In group II, 16 (94.1%) patients had GCS >8 and 12 (70.6%) required ICU admission, among which 4 (23.5%) were on mechanical ventilation, while in group III all patients had GCS <8 requiring ventilation. Hence group II and III included patients with focal neurological deficit and encephalopathy, respectively, representing progressive and extensive involvement of brain parenchyma because of edema or tentorial herniation.14 15 Neurological categorization represents cumulative neurological deficits due to cumulative neuronal loss at the time of CVST diagnosis, which extrapolates as clinical signs that determine the prognosis.
In this study radiological parameters including anatomical type and number of sinus involved were important for diagnosing CVST but they played very little role in predicting the hospital course and outcome. Occlusion of large sinuses may lead to either unilateral or bilateral neurological deficits or rarely result in isolated intracranial hypertension syndrome only.16 This emphasizes that outcome is influenced by extent of neuronal loss more than the number of occluded sinuses. This is in coherence with a previous study by Gunes et al who also found that presence of focal neurological deficits was a poor prognostic sign in CVST.13
Also, from our experience, hospital course can also be predicted by categorizing the patients according to the neurological deficits. Neurological predictors are easy to recognize by the physicians especially in the emergency department with detailed clinical and neurological evaluation of patients with CVST. This helps in early prediction of the hospital course, need for ICU admission, or ventilator support at the time of diagnosis of CVST and step-up therapeutic treatment options in anticipation of poor outcome. This anticipation of prognosis not only helps in decision-making in the clinical practice but also fills the gap of communication between the caregivers. This study also establishes that most patients with CVST had a benign prognosis, with mortality rates less than 3%, and among the surviving patients, 74.2% had a good functional outcome.
Although the individual time course in patients with CVST is variable with mortality risk during the acute phase of illness, but still there is a significant chance of good recovery in those who overcome the initial acute phase of the disease.
Our study has some limitations that should be taken into account. The sample size was small and our study had assessed outcome at the time of discharge and long-time follow-up was not done.
Conclusion
Early diagnosis and prompt recognition of pattern of neurological deficits not only predict the prognosis of patients with CVST but also help the clinicians in identifying the patients who need intensive monitoring in ICU or require ventilator support.
Acknowledgments
The authors acknowledge the participation of our patients in this study.
Conflict of Interest
None declared.
Funding None.
References
- Cerebral venous thrombosis.Major Problems in Neurology, 1st ed. London: WB Saunders; 1997. p. :27-104. In: ed.
- [Google Scholar]
- Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients. J Neurol Neurosurg Psychiatry. 2001;70(1):105-108.
- [Google Scholar]
- Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;352(17):1791-1798.
- [Google Scholar]
- Cerebral venous thrombosis: diagnosis and management. J Neurol. 2000;247(4):252-258.
- [Google Scholar]
- A practical score for prediction of outcome after cerebral venous thrombosis. Front Neurol. 2018;9:882.
- [Google Scholar]
- Cortical vein thrombosis in adult patients of cerebral venous sinus thrombosis correlates with poor outcome and brain lesions: a retrospective study. BMC Neurol. 2017;17(1):219.
- [Google Scholar]
- Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) Stroke. 2004;35(3):664-670.
- [Google Scholar]
- Cerebral venous thrombosis and headache–a case-series. Headache. 2015;55(6):806-814.
- [Google Scholar]
- Clinical associations, biological risk factors and outcomes of cerebral venous sinus thrombosis. J Int Med Res. 2016;44(6):1454-1461.
- [Google Scholar]
- Cerebral venous thrombosis: comparing characteristics of infective and non-infective aetiologies: a 12-year retrospective study. Postgrad Med J. 2015;91:670-674. (1082):
- [Google Scholar]
- Clinical presentations of cerebral vein and sinus thrombosis. Front Neurol Neurosci. 2008;23:77-88.
- [Google Scholar]






