Translate this page into:
An Uncommon Case of Celiac Disease and Deep Cerebral Venous Sinus Thrombosis
Monika Singla Department of Neurology, Dayanand Medical College and Hospital Ludhiana, Punjab 141001 India drmonika78@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Celiac disease is an enteropathy characterized by malabsorption related with gluten intolerance and immune-mediated pathogenesis. It may manifest with gastrointestinal features like diarrhea, abdominal pain, weight loss, and anemia. Besides, it can manifest with various extraintestinal features like ataxia, neuropathy, stroke, or sometimes venous sinus thrombosis. Being of autoimmune origin, relation with systemic lupus erythematosus has also been reported. Herein, we present a rare case of a young patient with celiac disease who presented with fever, headache, and altered sensorium and was found to have meningitis with deep cerebral venous sinus thrombosis.
Keywords
celiac disease
antitransglutaminase antibodies (anti-tTG Ab's)
cerebral venous sinus thrombosis
systemic lupus erythematosus
antinuclear antibody
Introduction
Celiac disease (CD) is a common gastrointestinal autoimmune inflammatory disorder of the small intestine, characterized by gluten intolerance leading to malabsorption. CD is also associated with several extraintestinal especially neurological complications as ataxia, epilepsy, bilateral occipital calcification, peripheral neuropathies, myopathy, stroke, and sometimes venous thrombosis.1 Estimated prevalence of thrombosis in CD in both children and adults is 8%.2 3 The common site of venous thrombosis in CD is usually Budd-Chiari syndrome and rarely, intracranial venous thrombosis.4 Reasons for high preponderance of venous thrombosis in CD are hyperhomocysteinemia, vitamin B 12 and folate deficiency, genetic predisposition (MTHFR mutations), and protein S deficiency.5 6 CD being an autoimmune disorder is found to be associated with various other immune disorders with high thrombogenic potential like systemic lupus erythematosus (SLE), Sjogren's syndrome and antiphospholipid syndrome.7
We hereby report a rare case of a young female, who presented to us with headache, fever, and altered sensorium, was found to have underlying CD with hyperhomocysteinemia, deep cerebral venous sinus thrombosis, and meningitis in due course.
Case History
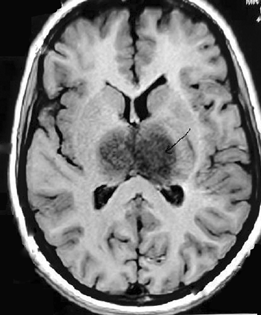
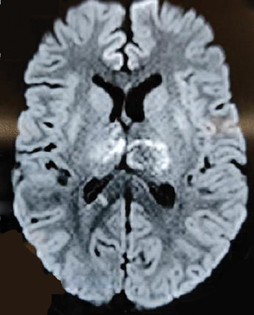
A 24-year-old female presented to our emergency department with 20 days history of intermittent, low-grade fever. She had continuous, holocranial headache, associated with vomiting for 4 to 5 days, followed by reduced responsiveness. She had no seizures at presentation. On examination, she was found in semistupor state, responding only to painful stimuli, with extensor plantars. Her pupils were equal in size and reacting to light. Fundus examination did not show any papilledema. She was found to have neck rigidity, with positive Kernig's sign. In view of fever, headache, vomiting, altered sensorium with meningeal signs, possibility of meningoencephalitis was kept. She required ventilatory support. Magnetic resonance imaging brain showed bilateral bulky thalami, with hemorrhage, and thrombosis of bilateral cerebral veins (Figs. 1 and 2). Magnetic resonance venogram suggested thrombosis of cerebral veins, vein of Galen, and superior sagittal sinus (Fig. 3). Diagnosis of deep and superficial cerebral venous thrombosis was made. Her biochemical profile and cerebrospinal fluid investigations are shown in Table 1. She was started with intravenous antibiotics, ceftriaxone, and vancomycin (antimeningitic dose). In view of deep cerebral venous sinus thrombosis, considering hypercoagulable state, protein C and protein S levels were sent and she was started on intravenous unfractionated heparin infusion. Antiedema measures were started in form of injection mannitol and dexamethasone along with antibiotics. On routine hematology profile, she was found to be anemic. Her serum calcium and potassium were low, though other biochemical profiles including kidney and liver function tests were normal. Thyroid profile was within normal limits. Family was enquired regarding dietary habits or any history of blood loss. Mother later on revealed that she was a diagnosed case of CD on the basis of endoscopy and duodenal biopsy, but as her anti tTG Abs levels improved, she started normal diet 1 year back. Detailed antinuclear antibody (ANA) profile was sent. Homocysteine levels were high. After 2 to 3 days of treatment, she initially started improving; she was weaned off from the ventilator and was extubated. She started maintaining on binasal oxygen. ANA profile report showed positivity of double-stranded DNA antibodies, suggestive of SLE. After 2 weeks of treatment, antibiotics were stopped. In view of underlying SLE, oral steroids were added, along with oral anticoagulation. She was discharged in stable condition.
|
Hemoglobin |
5.8 g/dL |
|
TLC |
6.4 |
|
Platelet count |
221 |
|
Serum iron |
10 |
|
Ferritin |
4.8 ng/mL |
|
ESR |
55 |
|
Serum LDH |
285 |
|
Serum haptoglobin |
108 |
|
CSF-TLC |
175, neutrophils (70%) |
|
CSF-Proteins |
155 mg/dL |
|
CSF-Glucose |
49 mg/dL |
|
Anti-tTG Abs |
160U mL |
|
ANA (by ELISA) |
4+ |
|
Protein-C |
62% |
|
Protein-S |
72.3% (low) |
|
Viral markers |
Nonreactive |
Abbreviations: ANA, antinuclear antibody; CSF, cerebrospinal fluid; ELISA, enzyme-linked immunosorbent assay; ESR, erythrocyte sedimentation rate; LDH, lactate dehydrogenase; TLC, total leucocyte count; tTG Abs, tissue transglutaminase antibodies.
-
Fig. 1 T1-weighted axial image showing hypointense lesions in bilateral thalami (arrow).
Fig. 1 T1-weighted axial image showing hypointense lesions in bilateral thalami (arrow).
-
Fig. 2 Diffusion-weighted axial image showing bilateral bright thalami suggestive of acute diffusion restriction.
Fig. 2 Diffusion-weighted axial image showing bilateral bright thalami suggestive of acute diffusion restriction.

-
Fig. 3 Magnetic resonance venogram coronal plane showing no flow related enhancement seen in bilateral internal cerebral veins, vein of Galen, and straight sinus suggestive of thrombosis.
Fig. 3 Magnetic resonance venogram coronal plane showing no flow related enhancement seen in bilateral internal cerebral veins, vein of Galen, and straight sinus suggestive of thrombosis.
Discussion
Being an autoimmune disorder, CD manifests as immunologically mediated inflammatory response, damaging the mucosa of the intestine leading to malabsorption of food.8 Despite intestinal disease and patient presenting with gut symptoms as diarrhea, weight loss, and failure to thrive, our patient had different manifestations like fever and headache. She was diagnosed to have deep cerebral venous sinus thrombosis, along with meningitis. This is an odd presentation, of deep cerebral venous system involvement in CD with SLE and meningitis.
SLE is a multisystem autoimmune disease with heterogeneous manifestations. SLE is associated with the production of autoantibodies, with a pathologic basis of vasculitis induced by immune complexes, further suggesting the blood vessels being an important target of over-activity of autoimmunity. Vascular involvement in SLE may vary form arteriostenosis and deep venous thrombosis. The vascular injuries caused by vasculitis, antiphospholipid antibodies, and prothrombotic tendencies in SLE might also be responsible for cerebral venous sinus thrombosis.9 10 11
Our patient presented with meningitis, besides deep cerebral venous sinus thrombosis, which may be due to her altered immune response initially. She responded well to antibiotics and heparin infusion. Therefore, our patient had quite different presentation of CD with meningitis with cortical venous sinus thrombosis, that too deep cerebral venous system, that is not reported in literature previously with underlying SLE.
Learning Points
-
Celiac disease is associated with hypercoagulable state as well as autoimmune disorders.
-
Deep venous sinus thrombosis can be a rare as well as serious association of celiac disease.
Conflict of Interest
None declared.
Funding None.
References
- [Adult celiac disease with thrombosis: a case series of seven patients. Role of thrombophilic factors] Rev Med Interne. 2011;32(10):600-604.
- [Google Scholar]
- Risk of thromboembolism in 14,000 individuals with coeliac disease. Br J Haematol. 2007;139(1):121-127.
- [Google Scholar]
- Hypercoagulability in celiac disease–an update. Autoimmun Rev. 2014;13(11):1138-1141.
- [Google Scholar]
- Recurrent cerebral venous thrombosis revealing celiac disease: an exceptional case report. Acta Neurol Belg. 2017;117(1):341-343.
- [Google Scholar]
- Cerebral venous thrombosis revealing celiac disease: a rare case report. Sch J Med Case Rep. 2018;6(6):397-400.
- [Google Scholar]
- Clinical characteristics of cerebral venous sinus thrombosis in patients with systemic lupus erythematosus: a single-centre experience in China. J Immunol Res. 2015;2015:540738.
- [Google Scholar]
- Systemic lupus erythematosus complicated with cerebral venous sinus thrombosis: a report of two cases. J Korean Med Sci. 2001;16(3):351-354.
- [Google Scholar]






