Translate this page into:
Arteriovenous Malformation of Conus Medullaris Fed by the Artery of Desproges-Gotteron
Shahnawas Bishwas, OSD, DG Health Department of Neurosurgery, Dhaka Medical College & Hospital Dhaka 1100 Bangladesh shahnawasns@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Presence of the artery of Desproges-Gotteron is extremely rare. It has seldom been mentioned in the literature as well. The authors have dealt with a case of a dural arteriovenous malformation (AVM) of conus medullaris fed by the artery of Desproges-Gotteron in a young female of 19 years. The patient presented with a tingling sensation of lower limbs, progressive difficulty walking, and incontinence of the bladder. There was weakness in all groups of muscle of both lower limbs and definite sensory level on examination. Magnetic resonance imaging revealed multiple flow voids at the level of conus medullaris. Spinal digital subtraction angiography (DSA) revealed dural AVM at the level of conus. The patient underwent transarterial embolization with 30% Endocryl(n-butyl cyanoacrylate) in two stages, and repeated spinal DSA revealed no evidence of residual AVM. Patient's neurology gradually improved. Almost 2 years down the line, the follow-up revealed gradual but complete motor and sensory deficits recovery except for occasional burning pain in lower limbs. Spinal AVM supplied by the artery of Desproges-Gotteron is a unique variation. Moreover, the authors believe that it is the first reported case in Bangladesh.
Keywords
conus medullaris
arteriovenous fistula
Desproges-Gotteron
embolization
Endocryl
Introduction
Desproges-Gotteron artery, often known as “cone artery,” is a posterior radiculomedullary (radiculopial) artery.1 It begins from the internal iliac artery or one of its branches,2 runs across the L5 or S1 nerve root until it reaches the conus medullaris, and anastomoses with the perimedullary network (conal basket). The existence of this artery, initially identified in a thesis by Desproges-Gotteron in 1955, is inconstant.3 Compression of the Desproges-Gotteron artery explains the clinical picture in which a patient comes with acute conus medullaris or cauda equina compression but no imaging evidence of direct compromise of these structures. We present a case of a patient who had a symptomatic arteriovenous malformation (AVM) of the conus medullaris nourished by the Desproges-Gotteron artery.
Case Report
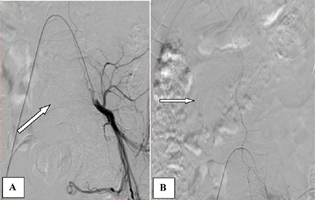
A 19-year-old woman arrived with tingling in her lower limbs, difficulties in walking, and bladder incontinence. On examination, there was a sensory level at L2 level with a diminished sense of vibration and joint position from the knee downward and power ⅕ and ⅖ in all groups of the muscle of left and right lower limbs. Magnetic resonance imaging (MRI) of the spine revealed multiple flow voids in the regions of conus medullaris and cauda equine (Fig. 1A). The presence of a dural AVM in the conus medullaris fed by the Desproges-Gotteron artery was verified by a digital subtraction angiography (DSA). This artery is derived from the internal iliac artery's posterior division, which entered the dura through the ventral sacral foramen along the sacral-1 root (Fig. 1B and C).

-
Fig. 1 Magnetic resonance imaging spine T2-weighted imaging showing multiple flow voids in conus medullaris and cauda equina (right arrow, [A]); spinal digital subtraction angiography (B, C) showing dural arteriovenous fistula in conus medullaris (right arrow [B] and left arrow [C]).
Fig. 1 Magnetic resonance imaging spine T2-weighted imaging showing multiple flow voids in conus medullaris and cauda equina (right arrow, [A]); spinal digital subtraction angiography (B, C) showing dural arteriovenous fistula in conus medullaris (right arrow [B] and left arrow [C]).
Transarterial embolization was performed with 30% Endocryl (n-butyl cyanoacrylate). In this endovascular procedure, the guiding catheter—Launcher RC 5 Fr was kept in the posterior division of the internal iliac artery, microcatheter—Apollo 3 cm (….) detachable tip catheter was navigated till the point of AVM over the microwire—Mirage.008 hydrophilic guide wire. Then embolization was performed of the AVM, including the pedicle of the draining vein's feeding artery and foot (Fig. 2). The patient's tingling sensation disappeared on the first postprocedural day. On the seventh postprocedural day, her power became ⅖ and ⅗ in all groups of the muscle of left and right lower limbs, respectively. She took regular physiotherapy. After 6 weeks, patient came to us walking with aid with improved bladder control.

-
Fig. 2 Transarterial embolization—guiding catheter in an internal iliac artery (right arrow [A]), artery of the Desproges-Gotteron (left oblique arrow [A]), microcatheter in arteriovenous malformation (oblique arrow [B]), embolization with 30% Endocryl (n-butyl cyanoacrylate, left arrow [C]).
Fig. 2 Transarterial embolization—guiding catheter in an internal iliac artery (right arrow [A]), artery of the Desproges-Gotteron (left oblique arrow [A]), microcatheter in arteriovenous malformation (oblique arrow [B]), embolization with 30% Endocryl (n-butyl cyanoacrylate, left arrow [C]).
Despite physiotherapy, her weakness persisted, and she developed stiffness in her lower limbs. Follow-up DSA almost 2 months after the first embolization revealed the presence of residual AVM. Transarterial embolization was again performed, ensuring complete occlusion of the nidus (Fig. 3). From the second postprocedural day, patient's weakness and stiffness improved. The patient was discharged with the advice of regular physiotherapy.
-
Fig. 3 The second session of embolization. Vascular catheter in an internal iliac artery (oblique arrow [A]) and microcatheter embolizing artery of Desproges-Gotteron (right arrow [B]).
Fig. 3 The second session of embolization. Vascular catheter in an internal iliac artery (oblique arrow [A]) and microcatheter embolizing artery of Desproges-Gotteron (right arrow [B]).
Almost 2 years down the line, the follow-up since the embolization, examination of her lower limbs revealed intact all modalities of sensation except the absence of vibration and joint position sense below the ankle; power improved up to 4 +/5 and 5/5 in all groups of the muscle of left and right lower limbs, respectively. Follow-up MRI of the spine also revealed the presence of no flow voids in the spine. She is expecting a baby in a couple of months.
Discussion
In the 1950s, Desproges-Gotteron investigated 91 patients with sciatica and motor loss who were checked in the rheumatology, neurology, and neurosurgery departments at the Lariboisière Teaching Hospital in Paris.3 He discovered in his research that the magnitude of a disc herniation did not always correlate with the likelihood of motor loss. A cadaveric examination of the L5 and S1 nerve roots revealed that an artery, the Desproges-Gotteron artery, supplied the L5 and S1 nerve roots and extended to the ventral surface of the conus in three of the twelve specimens. Desproges-Gotteron also discovered that in ∼15% of cases, the Adamkiewicz artery was absent or began higher than usual, and that in these cases, a lower lumbar nerve-following artery always contributed to the blood supply to the lower cord.3
Reis et al4 described an adult man with radicular discomfort, impotence, and urine retention who had conus medullaris syndrome. To treat his radicular pain and restore bladder function, he had foraminal decompression with L5–S1 microdiscectomy. The clinical situation was attributed by the authors of this case report to compression of the Desproges-Gotteron artery.
Following spinal manipulation, Balblanc et al2 reported a case of paraplegia in an older woman who presented with progressive back pain and difficulties in walking. This patient's presentation and course were likewise compatible with compression of the Desproges-Gotteron artery by a L4–5 disc fragment migration. Unfortunately, transforaminal glucocorticoid injection at L5–S1 has resulted in conus medullaris infarction, with the authors blaming the Desproges-Gotteron artery.5
The conus malformations are also included in newer classifications of spinal cord AVMs.6 7 Moreover, Mhiri et al8 described a case of an adult male who presented with growing lower limb paralysis and micturition failure and was diagnosed as a spinal dural arteriovenous fistula. An AVM supplied by a lateral sacral artery and drained by two enlarged ascending perimedullary veins was discovered on an MRI of the lumbosacral spine. The lateral sacral artery, on the other hand, supplies blood to the cauda equina on a regular basis.9 10
We believe that this is the first example of a dural AVM of the conus medullaris supplied by the Desproges-Gotteron artery successfully treated in Bangladesh. It is very advised that clinicians consider this rarity during the intervention.
Conclusion
Paraplegia due to spinal dural AVM fed by artery of Desproges-Gotteron is a rare incidence. Seldom it has been mentioned in the literature due to the extreme lack of diagnosed cases. Even with severe neurological abnormalities, endovascular embolization of a spinal AVM can be very rewarding, as demonstrated in this patient.
Conflict of Interest
None declared.
References
- Spinal cord ischemia: clinical and imaging patterns, pathogenesis, and outcomes in 27 patients. Arch Neurol. 2006;63(8):1113-1120.
- [Google Scholar]
- Vascular complication involving the conus medullaris or cauda equina after vertebral manipulation for an L4-L5 disk herniation. Rev Rhum Engl Ed. 1998;65(4):279-282.
- [Google Scholar]
- Foraminal L5-S1 disc herniation and conus medullaris syndrome: a vascular etiology? Acta Neurochir (Wien). 2007;149(5):533-535. , discussion 535
- [Google Scholar]
- Desproges-Gotteron artery, spinal cord infarction, and transforaminal glucocorticoid injections. Joint Bone Spine. 2009;76(1):120-121. , author reply 121–122
- [Google Scholar]
- Modified classification of spinal cord vascular lesions. J Neurosurg. 2002;96:145-156. (2, Suppl):
- [Google Scholar]
- Pediatric perimedullary arteriovenous fistula of the conus medullaris supplied by the artery of Desproges-Gotteron. J Neurosurg Pediatr. 2013;11(4):426-430.
- [Google Scholar]
- Sacral meningeal arteriovenous fistula supplied by branches of the hypogastric artery revealed by conus medullaris infarction. Spinal Cord. 2000;38(11):711-714.
- [Google Scholar]
- Arterial vascularization of the cauda equina. J Bone Joint Surg Am. 1981;63(1):53-62.
- [Google Scholar]






