Translate this page into:
Effect of Scapular Stabilization Exercise during Standing on Upper Limb Function and Gait Ability of Stroke Patients
Address for correspondence: Prof. Lee BH, Department of Physical Therapy, Sahmyook University, Hwarangro-815, Nowon-gu, Seoul 01795, Republic of Korea. E-mail: 3679@syu.ac.kr
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The purpose of this study was to determine the effect of scapular stabilization exercise during standing on a paretic side on upper limb function and gait ability of stroke patients.
Methods:
This study was a hospital-based, randomized controlled trial with a blinded assessor. A total of 17 patients with hemiplegic diagnosis after stroke were divided into two groups (9 patients in a study group and 8 patients in a control group). The study group received physical therapy and scapular stabilization exercise on a paretic side. Participants were subjected to initial evaluation before the treatment. Subjects were subsequently re-evaluated 4 and 8 weeks later to compare the changes. Measurements of hand function and gait ability were performed.
Results:
Based on multivariate analysis of variance for repeated-measures, there was a significant time effect for Timed Up and Go test (TUG) (F = 13.816, P = 0.000), Functional Gait Assessment (FGA) (F = 18.613, P = 0.000), and manual function test (MFT) (F = 16.777, P = 0.000). The group × time interaction effect was also significant for FGA (F = 4.966, P = 0.024) and MFT (F = 6.946, P = 0.003), but not for TUG test (F = 3.343, P = 0.069).
Conclusion:
Results of the present study indicated that scapular stabilization exercise during standing on a paretic side for 8 weeks had an effect on hand function and gait ability of hemiplegic patients after stroke. Further studies are needed to find the most proper exercise for stroke patients who have gait disability and upper limb dysfunction.
Keywords
Gait
scapular stabilization exercise
stroke
upper limb function
INTRODUCTION
Hemiplegic patients often present the abnormal gait patterns due to weakness in paretic side. Development of functional gait ability plays a crucial role in achieving functional independency for these patients.[1]
Many stroke patients cannot use their impaired upper limb properly despite long-term intensive therapy because damage to the upper limb after stroke is one of the most common and severe stroke side effects.[2] The hand function of the upper limb is the most highly damaged one in brain-damaged patients. This is because betz cell is the most abundant cell in the cerebral cortex. It is responsible for the control of hand.[3] Adjustment to a specific pattern is required for segments between the neck and the body to maintain the stability of the upper body during walking.[4] Arbitration is particularly required for this adjustment because the upper body segments can affect dynamic stability.[5] The upper body uprights the trunk while walking. Body stability through the movement of the upper body is ±1.5° of movement of the body during walking. This can enhance the stability of the head and reduce improper signals from an otolith and the vestibular system.[6] With the dynamic regulation of the scapular, stable muscles can make scapular effectively positioned to obtain ideal postural control on body weight load. In addition, when setting the position of the right shoulder blade, dynamic control capability on the scapular thoracic joints are reacquired. Shoulder stabilization exercises are focused on the recovery of balanced ability to control between shoulder stabilizers. Recently, closed kinematic chain exercises have frequently been used in therapeutic exercises of the upper extremities.[7] Walking is also a complicated motor act requiring the coordination of trunk and limb muscles involving many joints.[8] It is a basic prerequisite of daily life. It is also one of the most automatic daily activities. It is the functional result of interactions among biomechanical, neurophysiological, and motor control systems. The desire to regain walking ability after neurological dysfunction is often the primary goal of rehabilitation. A lot of time and energy are devoted to retrain walking after stroke.[910] Asymmetric gait patterns are often related to compensatory movements of both the paretic side and the nonparetic side.[11] This compensation may contribute to limited functional recovery.[12] Therefore, fall prevention and improvement of walking ability are often the major focus of rehabilitation for stroke patients.[13]
The effects of scapular stabilization exercise during standing have been demonstrated in the previous studies.[71415161718] However, the effects of scapular stabilization exercise during standing on a paretic side on gait ability of hemiplegic patients after stroke remain unclear. Therefore, the objective of this study was to determine the effects of scapular stabilization exercise during standing on a paretic side on the gait ability of hemiplegic patients after stroke.
METHODS
Participants
This study was conducted at B Hospital located at S city, Gyeonggi-do. A total of 17 patients who were admitted to inpatient rehabilitation center were selected as the study group. The inclusion criteria were those who have been diagnosed with hemiplegia for more than 6 months;[19] those who were able to respond properly from a sensory stimuli given by the examiner with over 24 points in Mini–Mental State Examination;[20] those who were able to carry out instructions given by verbal command;[15] those who were independent in ambulation with or without a walking aid;[21] those who were able to fire the dorsiflexor more than 5° in knee extension;[22] and those who understood the content of study and agreed to participate actively.
Experimental procedures
Seventeen participants were randomly assigned with computer lottery study group (scapular stabilization exercise) (n = 9) and control group (simple scapular exercise) (n = 8). The scapular stabilization exercise applied in this study was a revised version of that used in a previous study.[23] First, maximum shoulder external rotation at 45° abduction was performed in the supine position and gradually extended as long as there was no pain. Then, stretching was performed at 90° of the shoulder in a sitting position and gradually extended as long as there was no pain. Finally, the subjects reached toward the ground with their palms, with the shoulder and elbow extension in the sitting position, gradually extending their reach as long as there was no pain.
Strengthening exercise on scapular stabilization used for functional scapular instability stroke patients in the study of Awad et al.[18] was used in this study with proper revision. Briefly, participants received 30 min of strengthening exercise on scapular stabilization in the supine and sitting posture. Exercise was conducted 3 times per weeks for a total of 8 weeks. Participants in the control group (simple scapular exercise) received 30 min of shoulder movement exercise (flexion, extension, abduction, adduction, internal rotation, and external rotation) in the supine and sitting posture. All the participants in both groups received 30-min sessions of conventional physical therapy for 10 times per week for 4 weeks. The main reasons for 7 dropouts from the study were a personal issue [Figure 1].

- Flow of participants through the exercise program
Outcome measurement
Timed Up and Go test (TUG) is functional flexibility test invented by Podsiadlo and Richardson.[24] It was designed as a quick measure of basic balance and mobility skill of elderly people. The time taken for subjects to rise from an armchair, walk 3 m, turn, and return to the chair is measured in seconds.
Functional Gait Assessment (FGA) is used to evaluate postural stabilization during gait. It was initially invented for the elderly who had great risk of falling down. In this study, the original form of FGA was properly revised with an addition of three items in Dynamic Gait Index.[25]
Manual function test (MFT) is an upper limb function assessment for hemiplegic patients after stroke. It measures eight motions with respect to the movement of the shoulder. A score is obtained for each item with an average of 32-point.[26]
Statistical analysis
This study used SPSS version 18.0 (SPSS (IBM Co., Armonk, NY, USA)) for statistical analysis of all measured data. To find general characteristic and normal distribution between the two groups, Chi-square distribution was applied to all participants. Analysis of variance (ANOVA) was used to distinguish the study group from control group. ANOVA was also used to compare the categories in each group. Normal distribution was implemented for the results of the study groups and control groups. Differences between the two groups were analyzed using multivariate ANOVA for repeated-measures (MANOVA-RMs). Pearson's correlation analysis was performed to determine the correlations between balance ability and gait ability. Statistical significance was considered when P < 0.05.
RESULTS
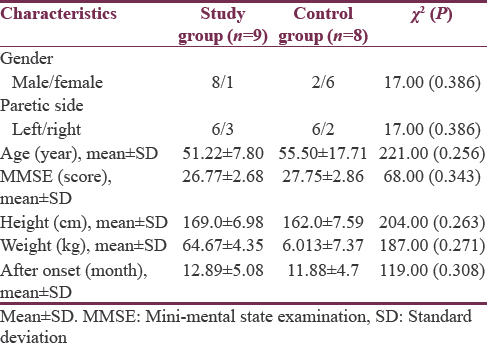
This study enrolled 17 patients, including 9 in the study group and 8 in the control group. In the study group, six patients had left hemiplegia while three patients had right hemiplegia. In the control group, six patients had left hemiplegia, and two patients had right hemiplegia. All patients had similar height, age, and weight. Characteristic of subjects were summarized in Table 1.
After scapular stabilization exercise on a paretic side, MANOVA-RM was performed. Results are presented in Table 2. There was a significant time effect for TUG (F = 13.816, P = 0.000), FGA (F = 18.613, P = 0.000), and MFT (F = 16.777, P = 0.000). The group x time interaction effect for these variables was also significant for FGA (F = 4.966, P = 0.024) and MFT (F = 6.946, P = 0.003), but not for TUG test (F = 3.343, P = 0.069).

DISCUSSION
Scapular stabilization is particularly affected by scapular stability during movement in cardinal planes. The previous studies on recovery of upper extremity function have investigated the effects of balance, upper limb function, and gait speed in poststroke patients.[71415161718]
Movement disorders can bring about limitations to muscle control and motion functions or mobility. They can also result in degradation of balance control abilities. Hemiplegia is accompanied by increased posture instability, asymmetrical weight bearing, impairment of body weight transfer capabilities, and decreased postural stability.[2728]
According to Eng and Chu,[29] gait abilities of paretic and nonparetic lower limbs are not identical. In addition, the paretic side is less competent in weight-bearing ability. In particular, slow gait velocity and reduced gait endurance may cause many difficulties in the recovery of gait ability. Overcoming these difficulties is a crucial objective of stroke patient rehabilitation.[30] Many studies have reported treatment methods for improving the gait ability of stroke patients.[31] Stroke patients suffer from deficits in functional ambulation capacity, balance, walking velocity, cadence, stride length, temporal gait pattern, and muscular activity pattern.
In general, stroke patients show decreased walking velocity, which can result in decreased paretic stance phase but increased paretic swing phase.[32]
According to Hill et al.,[33] gait speed and shoulder girdle strength are improved (P < 0.05) after 8 weeks of training for stroke patients. In the study group of this study, gait speed (TUG test) was changed from 24.01 to 18.95 s. In addition, FGA scores were changed from 16.00 to 19.78 points after 8 weeks of training.
Upper extremity hemiparesis can impair the performance of many daily activities such as dressing, bathing, self-care, and writing, thereby resulting in reduced functional independence. Therefore, stroke survivors need to participate in rehabilitation programs to achieve functional independence.[34] Approximately, one-third of all stroke survivors have significant residual disability. The severity of upper extremity hemiparesis is a significant determinant of poststroke disability and quality of life.[35] Hemiparesis of the upper extremity is often the most severe one in the most distal regions. Although proximal muscles and joints may be the least affected ones, purposeful movement requiring precise control of the proximal segments is slow, inaccurate, and poorly coordinated.[36]
Postural control of the trunk is also a critical component of independent performance of activities of daily living. Hsieh et al. have investigated the relationship between trunk control and comprehensive activities of daily living.[37] A paretic arm can change scapular orientation because scapular stabilizers are often so impaired by muscle weakness that they cannot overcome arm weight or maintain anatomical characteristics. The weakness of scapular stabilizers has been shown to increase motor impairment of the upper extremities and consequently affect many stroke survivors to achieve independent daily livings.[38] The efficacy of scapular stabilization exercise in improving balance and performance of daily activities by stroke patients was also investigated in this study. An important finding of this study was a statistically significant improvement in the function of the paretic upper extremity after the scapular stabilization exercise. However, in the study group, MFT was changed from 9.67 to 12.56 points. For upper limb function, there was a significant time effect on MFT (F = 16.777, P = 0.000) and group × time effect on MFT (F = 6.946, P = 0.003).
Gait ability showed statistically significant differences in group × time effect in both groups. This study was focused on the effect of scapular stabilization exercise on a paretic side on balance and gait in hemiplegic patients. We assumed that compensate movement was intervened through the training. It played a major role for TUG, FGA, and MFT tests score improvement.
CONCLUSION
Results of the present study indicated that scapular stabilization exercise during standing on a paretic side for 8 weeks had an effect on the gait ability of hemiplegic patients after stroke. Further studies needed to find the most proper exercise for stroke patients with gait disability and upper limb dysfunction.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Steps to Follow: A Guide to the Treatment of Adult Hemiplegia: Based on the Concept of K. and B. Bobath Berlin, New York: Springer-Verlag; 1985.
- Relationship of isokinetic peak torque with work and power for ankle plantar flexion and dorsiflexion. J Orthop Sports Phys Ther. 1995;22:113-5.
- [Google Scholar]
- The 38th annual John Stanley Coulter lecture. The Winter of Our Discontent: Breaking intolerable time locks for stroke survivors. Arch Phys Med Rehabil. 1989;70:92-4.
- [Google Scholar]
- Sagittal plane analysis of head, neck, and trunk kinematics and electromyographic activity during locomotion. J Orthop Sports Phys Ther. 2001;31:255-62.
- [Google Scholar]
- Biomechanical walking pattern changes in the fit and healthy elderly. Phys Ther. 1990;70:340-7.
- [Google Scholar]
- Head stabilization during various locomotor tasks in humans. II. Patients with bilateral peripheral vestibular deficits. Exp Brain Res. 1991;85:208-17.
- [Google Scholar]
- Central pattern generation of locomotion: A review of the evidence. Phys Ther. 2002;82:69-83.
- [Google Scholar]
- Relationship between step length asymmetry and walking performance in subjects with chronic hemiparesis. Arch Phys Med Rehabil. 2007;88:43-9.
- [Google Scholar]
- Task-specific training with trunk restraint on arm recovery in stroke: Randomized control trial. Stroke. 2006;37:186-92.
- [Google Scholar]
- Falls and injury prevention should be part of every stroke rehabilitation plan. Clin Rehabil. 2005;19:441-51.
- [Google Scholar]
- Three-dimensional scapulothoracic motion during active and passive arm elevation. Clin Biomech (Bristol, Avon). 2005;20:700-9.
- [Google Scholar]
- Functional activity characteristics of individuals with shoulder dysfunctions. J Electromyogr Kinesiol. 2005;15:576-86.
- [Google Scholar]
- The effects of stretching and stabilization exercise on the improvement of spastic shoulder function in hemiplegic patients. J Phys Ther Sci. 2014;26:491-5.
- [Google Scholar]
- The effects of active scapular protraction on the muscle activation and function of the upper extremity. J Phys Ther Sci. 2014;26:599-603.
- [Google Scholar]
- Effect of shoulder girdle strengthening on trunk alignment in patients with stroke. J Phys Ther Sci. 2015;27:2195-200.
- [Google Scholar]
- Determinants of walking function after stroke: Differences by deficit severity. Arch Phys Med Rehabil. 2007;88:115-9.
- [Google Scholar]
- Home-based motor imagery training for gait rehabilitation of people with chronic poststroke hemiparesis. Arch Phys Med Rehabil. 2008;89:1580-8.
- [Google Scholar]
- Relationship between ambulatory capacity and cardiorespiratory fitness in chronic stroke: Influence of stroke-specific impairments. Chest. 2005;127:495-501.
- [Google Scholar]
- A randomized controlled trial of an implantable 2-channel peroneal nerve stimulator on walking speed and activity in poststroke hemiplegia. Arch Phys Med Rehabil. 2007;88:971-8.
- [Google Scholar]
- Strengthening interventions increase strength and improve activity after stroke: A systematic review. Aust J Physiother. 2006;52:241-8.
- [Google Scholar]
- The timed “Up & amp; go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142-8.
- [Google Scholar]
- Functional gait assessment and balance evaluation system test: Reliability, validity, sensitivity, and specificity for identifying individuals with Parkinson disease who fall. Phys Ther. 2011;91:102-13.
- [Google Scholar]
- Reliability and validity of the manual function test in patients with stroke. Am J Phys Med Rehabil. 2009;88:247-55.
- [Google Scholar]
- Sonographic monitoring of mass effect in stroke patients treated with hypothermia. Correlation with intracranial pressure and matrix metalloproteinase 2 and 9 expression. J Neurol Sci. 2009;276:75-8.
- [Google Scholar]
- The effect of treadmill-based incremental leg weight loading training on the balance of stroke patients. J Phys Ther Sci. 2014;26:235-7.
- [Google Scholar]
- Reliability and comparison of weight-bearing ability during standing tasks for individuals with chronic stroke. Arch Phys Med Rehabil. 2002;83:1138-44.
- [Google Scholar]
- Toward a common language for function, disability, and health. Phys Ther. 2006;86:726-34.
- [Google Scholar]
- Analysis of impairments influencing gait velocity and asymmetry of hemiplegic patients after mild to moderate stroke. Arch Phys Med Rehabil. 2003;84:1185-93.
- [Google Scholar]
- Effect of treadmill exercise training on spatial and temporal gait parameters in subjects with chronic stroke: A preliminary report. J Rehabil Res Dev. 2008;45:221-8.
- [Google Scholar]
- Maximal strength training enhances strength and functional performance in chronic stroke survivors. Am J Phys Med Rehabil. 2012;91:393-400.
- [Google Scholar]
- Effect of rehabilitation tasks on organization of movement after stroke. Am J Occup Ther. 1999;53:333-44.
- [Google Scholar]
- Compensation in recovery of upper extremity function after stroke: The copenhagen stroke study. Arch Phys Med Rehabil. 1994;75:852-7.
- [Google Scholar]
- Rehabilitation of arm function after stroke. Literature review. Ann Phys Rehabil Med. 2009;52:269-93.
- [Google Scholar]
- Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002;33:2626-30.
- [Google Scholar]
- Scapular and humeral movement patterns of people with stroke during range-of-motion exercises. J Neurol Phys Ther. 2011;35:18-25.
- [Google Scholar]






