Translate this page into:
A rare case of recurrent headache during exercise due to severe intracranial atherosclerotic stenosis
*Corresponding author: Rudolph Muliawan Putera, Department of Neurology, Airlangga Faculty of Medicine, Dr. Soetomo General Hospital, Surabaya, Indonesia. rudolph_muliawan@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Putera RM, Sani AF. A rare case of recurrent headache during exercise due to severe intracranial atherosclerotic stenosis. J Neurosci Rural Pract 2022;13:775-7.
Abstract
Intracranial atherosclerotic stenosis (ICAS) can cause ischemic stroke, up to 30-50% stroke in Asian population. However, recurrent exercise-induced headache due to ICAS has not been reported. We present a case of a patient 60-year-old male suffering from recurrent headache during exercise due to severe ICAS. The headache occurred after 5 minutes of running, appeared shortly after every running, and resolved at rest. Head magnetic resonance angiography showed moderate bilateral stenosis at middle cerebral artery (MCA), and cerebral catheter angiography confirmed 70% stenosis of the left MCA and 20% stenosis of the right MCA, with robust antegrade flow and good collaterals which explained why there was no neurological deficit. After treated with best medical therapy, including dual antiplatelet, statin therapy, and risk factor modification, for 90 days, he was capable of running for 20 min without headache.
Keywords
Exercise headache
ICAS
Secondary headache
Red flags
Best medical therapy
INTRODUCTION
Intracranial atherosclerosis stenosis (ICAS) of large intracranial arteries accounts for 6–50% of all ischemic strokes worldwide.[1-5] A recent study reported a more frequent occurrence of the anterior circulation in Chinese population with ICAS, with the most common location at middle cerebral artery (MCA).[3] ICAS events are associated with advanced age, diabetes, hypertension, and dyslipidemia.[6]
Secondary headaches are very important to consider as they are sometimes serious and can be life-threatening. Headache in this case was sudden with onset after 50 years. There was a change in the pattern in which the patient, who had previously exercised regularly for five years without headaches, experienced headaches after doing sports activities.[7,8]
CASE REPORT
A 60-year-old man presented to the neurology clinic with complaint of headache for two months before, worsening in the past one month. It occurred after 5 min of running for a distance of 500 m, with a Numeric Rating Scale (NRS) 7. It appeared shortly after every running and was improved with rest. There was no history of the previous headaches or complaints of other neurological deficits. He had a history of hypertension, dyslipidemia, and diabetes mellitus type 2.
Magnetic resonance imaging of the head [Figure 1] did not reveal any signs of stroke. Cerebral catheter angiography [Figure 2] revealed 70% stenosis of the M1 of the left MCA, 30% stenosis of the left supraclinoid internal carotid artery, and 20% stenosis of the M1 of the right MCA, and stenosis of the anterior inferior cerebellar artery with good antegrade flow and good collateral. This explains how the patient did not suffer from stroke manifestations.
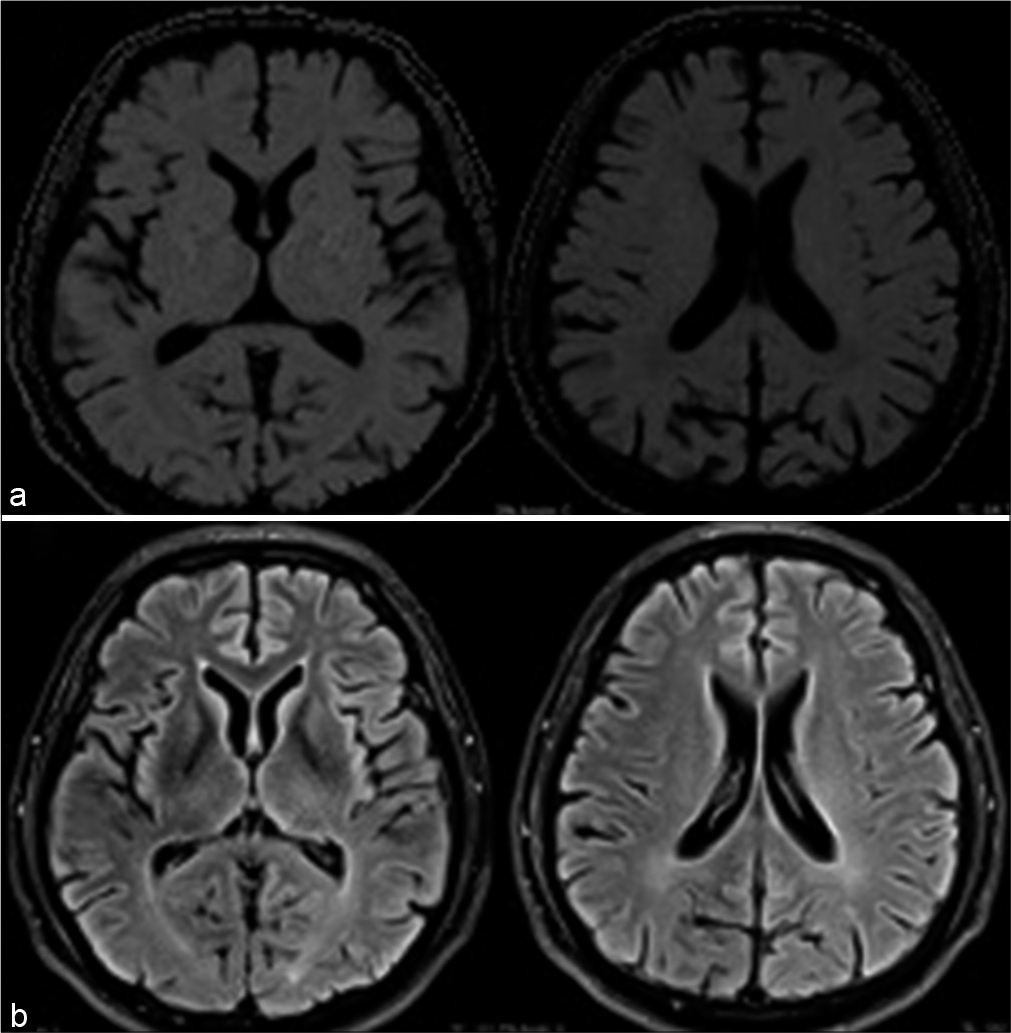
- Magnetic resonance imaging of the head, with diffusion-weighted imaging (a) and fluid attenuated inversion recovery (b) sequence, showing no lesion of stroke.
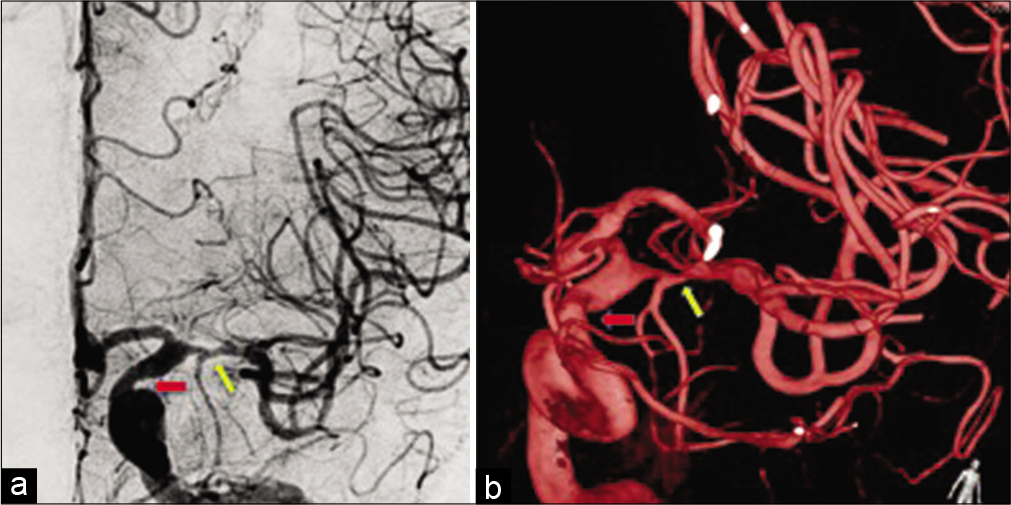
- Results of cerebral catheter angiography (a) and three-dimensional reconstruction (b) showing 70% stenosis of the M1 segment of the left middle cerebral artery (yellow arrow), 30% stenosis of the left supraclinoid ICA (red arrow).
DISCUSSION
A longitudinal and cohort study reports that mild-to-moderate symptomatic ICAS was an independent risk factor for the future ischemic stroke in a healthy population.[6] Symptomatic ICAS patients with >70% luminal stenosis of large intracranial arteries increased the risk of stroke by 20% at one year and poorly collaterals reflect distal perfusion status.[2,9]
Case reports of headaches that occur after sports activities have not been reported and the mechanism of headache in ICAS still needs more investigation. Recent studies report that the annual risk of stroke in asymptomatic patients with at least 50% stenosis of large intracranial arteries is <10%.[10]
Intensive medical therapy including antiplatelet therapy, aggressive control of cardiovascular risk factors, and lifestyle modification, remains the standard of care in patients with ICAS.[4,11] The use of short-term combination aspirin and clopidogrel is effective in reducing the risk of stroke recurrence in patients with ICAS.[1]
After the patient received intensive medical therapy including dual antiplatelet for 90 days, control of hypertension and dyslipidemia, moderate exercise, and low fat and low salt diet, there were improvements from laboratory results of vascular risk factors and also clinically in which patients could run for 20 min over 800 m with NRS 1.
However, patients with high-grade symptomatic ICAS still have a substantial risk of recurrent TIA and stroke even after receiving intensive medical therapy.[12] Angioplasty may be used for severe ICAS in patients with recurrent ischemic attacks and on medical therapy.[13-15] Endovascular therapy could lessen the risk of perioperative complications and offer superior benefits for symptomatic ICAS patients with strict patient selection, selection of the type of percutaneous transluminal angioplasty and stenting, and operator experience.[9,11]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Aterosclerotic intracranial arterial stenosis. Lancet Neurol. 2014;12:1106-14.
- [CrossRef] [Google Scholar]
- Diagnosis and management of active intracranial atherosclerotic disease: A case study. Stroke. 2018;49:e221-3.
- [CrossRef] [Google Scholar]
- Intracranial arterial stenosis in Caucasian versus Chinese patients with TIA and minor stroke: Two contemporaneous cohorts and a systematic review. J Neurol Neurosurg Psychiatry. 2021;92:590-7.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial atherosclerosis treatment: Past, present, and future. Stroke. 2020;51:e49-53.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of symptomatic intracranial atherosclerotic disease In: New Insight into Cerebrovascular Diseases - An Updated Comprehensive Review. London: IntechOpen; 2020.
- [Google Scholar]
- A prospective study of asymptomatic intracranial atherosclerotic stenosis in neurologically normal volunteers in a Japanese cohort. Front Neurol. 2016;7:39.
- [CrossRef] [PubMed] [Google Scholar]
- Headache disorders: Differentiating and managing the common subtypes. Br J Pain. 2012;6:124-32.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular treatment of intracranial atherosclerotic stenosis: Current debates and future prospects. Front Neurol. 2018;9:666.
- [CrossRef] [PubMed] [Google Scholar]
- Prognosis of asymptomatic intracranial stenosis in patients with transient ischemic attack and minor stroke. JAMA Neurol. 2020;77:947-54.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial atherosclerotic stenoses: Pathophysiology, epidemiology, risk factors and current therapy options. Adv Ther. 2020;37:1829-65.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic and asymptomatic intracranial atherosclerotic stenosis: 3 years' prospective study. J Neurol. 2020;267:1687-98.
- [CrossRef] [PubMed] [Google Scholar]
- China angioplasty and stenting for symptomatic intracranial severe stenosis (CASSISS): A new, prospective, multicenter, randomized controlled trial in China. Interv Neuroradiol. 2015;21:196-204.
- [CrossRef] [PubMed] [Google Scholar]
- Concomitant asymptomatic intracranial atherosclerotic stenosis increase the 30-day risk of stroke in patients undergoing symptomatic intracranial atherosclerotic stenosis stenting. J Stroke Cerebrovasc Dis. 2018;27:479-85.
- [CrossRef] [PubMed] [Google Scholar]







