Translate this page into:
Which Classification of Cavernous Sinus Syndrome is Better - Ishikawa or Jefferson? A Prospective Study of 73 Patients
Address for correspondence: Dr. Vivek Lal, Department of Neurology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. E-mail: vivekl44@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Ishikawa and Jefferson are the two most commonly used systems used for the classification of cavernous sinus syndrome (CSS). However, relative utilities of these two classification systems have not been evaluated in detail in developing countries. In this study, we compared relative utilities of these two classification schemes in the evaluation of CSS.
Objective:
To compare the utility of Jefferson and Ishikawa classifications in the evaluation of CSS.
Patients and Methods:
A total of 73 consecutive patients of CSS were prospectively classified using either Ishikawa or Jefferson classification and relative utility of these two classification schemes in determining etiology of CSS was compared.
Results:
While only 46.6% of patients could be classified using Jefferson classification, 95.5% of patients could be classified using Ishikawa scheme. CSS was classified as anterior, middle, and posterior in 17.8%, 21.9%, and 8.2% of patients, respectively, as per the Jefferson classification. As per the Ishikawa classification, 37% of patients each showed anterior and posterior CSS, 16.4% showed middle CSS, whereas 4.1% had whole CSS. Middle CSS was significantly associated with the presence of fungal infections (P = 0.045) as per Jefferson classifications, and anterior CSS was significantly associated with a vascular etiology (P = 0.005) as per Ishikawa classification. Overall, inflammatory causes were the most common cause for anterior CSS, while tumors accounted for maximum cases of posterior CSS.
Conclusion:
Although more number of patients could be classified using Ishikawa classification, there was no advantage of Ishikawa classification over Jefferson with regard to determination of etiology of CSS.
Keywords
Cavernous sinus syndrome
Ishikawa
Jefferson
INTRODUCTION
The term cavernous sinus syndrome (CSS) is used to denote any disease process which affects the CS.[1234] Determination of exact etiology of CSS is often difficult due to the lack of amenability to tissue diagnosis. Thus, treatment is often empirical and based on clinical presentation and radiological findings. Thus, if the classification of CSS into different types can throw light on underlying etiology, it might help in further management.
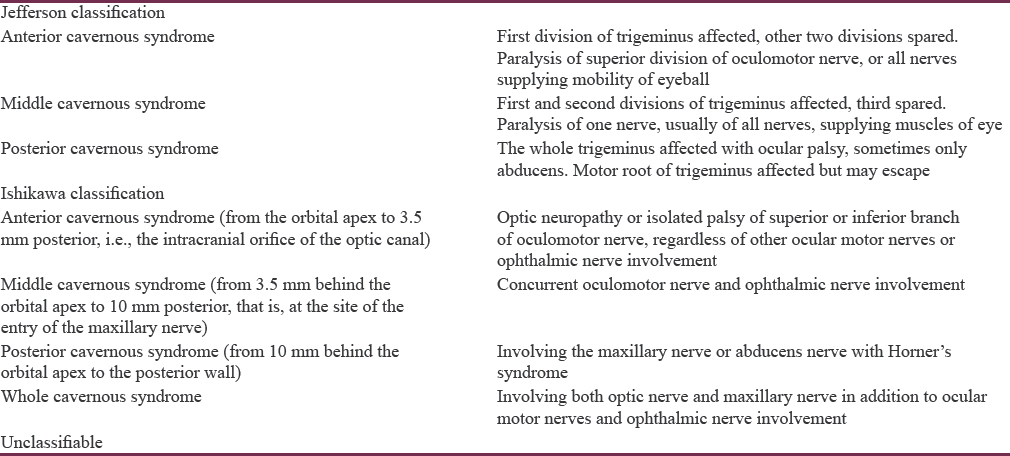
CSS was first classified by Jefferson[5] into three types based on the extent of involvement of trigeminal nerve [Table 1]. Since then, this classification has been the gold standard and given in most textbooks of neurology. In 1996, Ishikawa[6] emphasized the lack of clinico-anatomical correlation in Jefferson's classification and proposed a new classification of CSS [Table 1].[7] Subsequently, a Japanese study found that majority of patients who remained unclassified by Jefferson classification can be classified using Ishikawa scheme. Furthermore, when classified according to Ishikawa's scheme, anterior CS lesions were often due to inflammatory etiologies, whereas middle and posterior CS lesions were due to malignancies, suggesting that this classification system may play a role in determining etiology of CSS.[7] However, etiological profile of CSS is likely to be different in developing countries (e.g., India) where infections constitute a major chunk. There is no data regarding the utility of these two classification schemes from developing world. Thus, we planned this study to compare utility of these two systems of classification in CSS.
Aims and objectives
To compare the utility of Jefferson versus Ishikawa classification in the evaluation of CSS.
Patients and Methods
This prospective observational study was conducted from January 2014 to July 2015, on 73 patients of CSS at a Tertiary Care Hospital and University Teaching Center in Northern India. The study was approved by the Institutional Ethics Committee and written informed consent was obtained from all the patients. CSS was defined as involvement of 2 or more of the third, fourth, fifth (V1, V2), or sixth cranial nerves, or involvement of only 1 of them in combination with a neuroimaging-confirmed lesion in the CS. Once enrolled, all the patients were subjected to meticulous history and detailed examination. All the patients underwent investigations including detailed hemogram with erythrocyte sedimentation rate and C-reactive protein, biochemistry profile, serum electrolytes, testing for human immunodeficiency virus as well as hepatitis B and C viruses, Gadolinium-enhanced magnetic resonance imaging brain on a 1.5 Tesla Magnetom with thin section cuts of the CS region. Further etiological work-up including biopsies, antinuclear, and cytoplasmic anti-neutrophilic antibody testing, serum galactomannan, serum angiotensin converting enzyme levels, contrast-enhanced computed tomography scan of chest and abdomen and cerebrospinal fluid examination, was carried out wherever indicated. All the patients were classified using Jefferson and Ishikawa schemes by two neurologists with experience in neuro-ophthalmology independently, and final decision was taken by consensus.
Statistical analysis
Statistical analysis was performed using SPSS version 22 (IBM Corp. Released 2013. IBM Statistics for windows, Version 22.0. Armonk, NY: IBM Corp). Quantitative data were expressed in mean and or median. Qualitative or categorical data were expressed in frequency or percentage. Chi-square or Fisher's exact test was applied to compare the discrete variables. P < 0.05 was considered statistically significant.
RESULTS
Demographic, clinical, and etiological profile of cavernous sinus syndrome
The data regarding demographic and clinical profile are given in Table 2. The exact etiology of CSS was obtained in 63/73 (86.3%) patients of CSS. The detailed etiological profile is also given in Table 2. Among the ten patients, in which, we could not establish exact etiology, six had probable fungal CSS; two had probable diabetes-related ophthalmoplegia, and two remain unclassified.
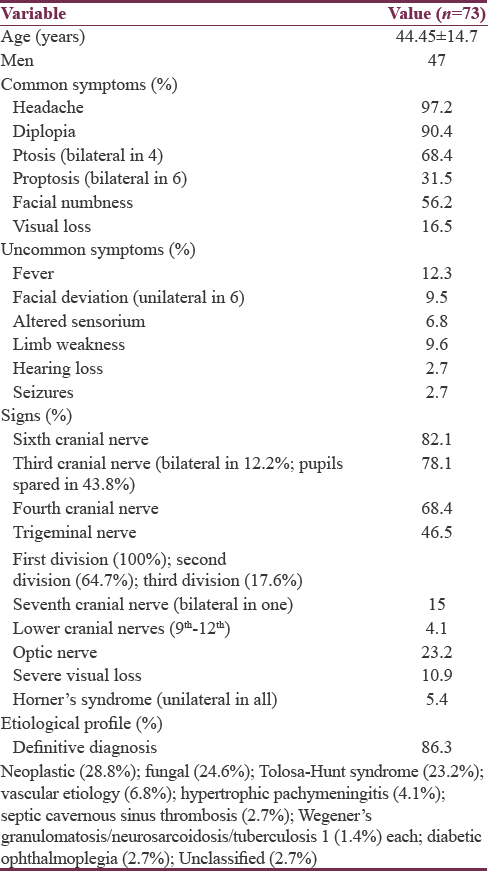
Jefferson versus Ishikawa classification of cavernous sinus syndrome
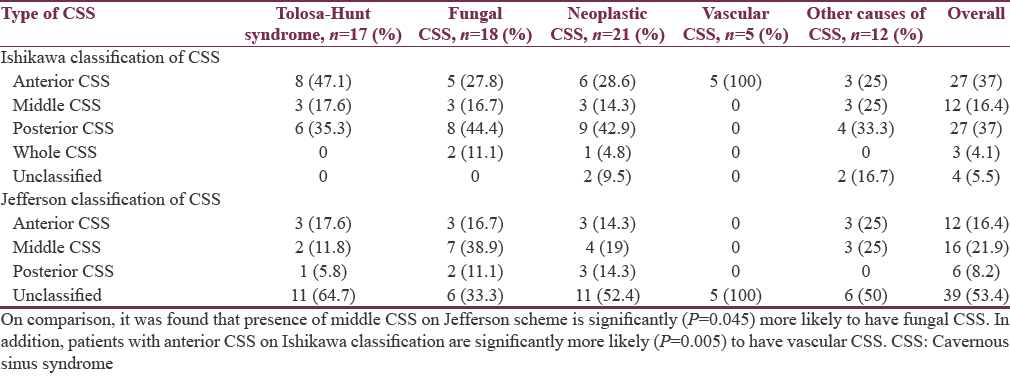
All the patients were classified by Ishikawa and Jefferson schemes [Table 3]. The number of patients which could be classified using Ishikawa classification (n = 69; 95.5%) was much higher than Jefferson classification (n = 34; 46.6%). Using Jefferson classification, CSS could be classified as anterior, middle, and posterior in 12 (16.4%), 16 (21.9%), and 6 (8.2%) patients, respectively. Patients with middle CSS were significantly (P = 0.045) more likely to have fungal CSS. As per Ishikawa classification, 27 patients each (37%) had anterior and posterior CSS [Figure 1] whereas 12 (16.4%) had middle CSS and 3 (4.1%) had whole CSS. Patients with anterior CSS were significantly more likely (P = 0.005) to have vascular etiology. Overall, inflammatory causes accounted for maximum number of anterior CSS while tumors accounted for maximum cases of posterior CSS, although the difference was not statistically significant.
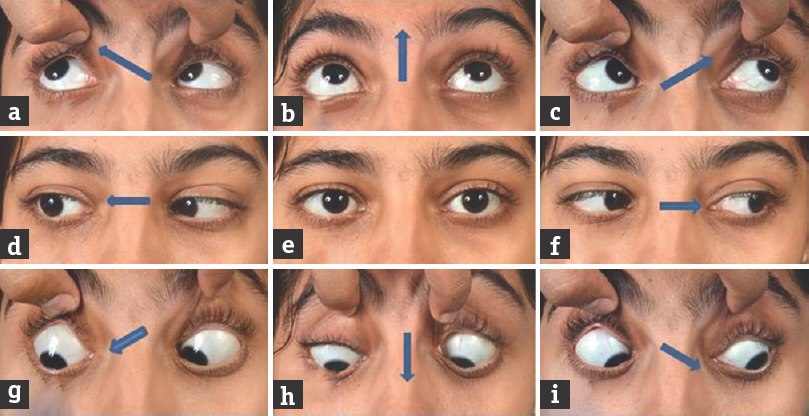
- Meningioma in a 34-year-old female presenting with right lateral rectus palsy and numbness over mandibular division of trigeminal nerve. Extraocular movements in 9 cardinal positions of gaze (a-i) (the black and white arrows indicate the direction of intended movement of eyeballs). Note: Restriction of right eye in lateral gaze (two-dimensional) suggestive of the right lateral rectus palsy; contrast-enhanced magnetic resonance imaging of the brain (3J-K) was suggestive of a meningioma (3J-coronal, 3K-axial) (black and white arrows). As per Jefferson classification, she would come under the unclassifiable category while as per the Ishikawa classification; she could be classified as a posterior cavernous sinus syndrome
DISCUSSION
Ishikawa was the first author who studied CS structure by stereotaxically analyzing 30 µm serial CS sections. Based on his observations, Ishikawa proposed his classification for CS lesions.
In the current study, 35 (48.9%) additional patients could be classified using Ishikawa scheme similar to that reported by Yoshihara et al.[7] The reason for this is the presence of some inherent deficiencies in Jefferson classification. Jefferson classification is heavily biased toward trigeminal nerve and ignores other structures contained within CS such as optic nerve, oculosympathetic fibers, inferior division of the 3rd cranial nerve and maxillary nerve either alone or in combination with mandibular nerve. This may lead to an increase in number of unclassifiable cases in Jefferson scheme. For instance optic nerve was involved in 17 (23.2%) patients in this study. After leaving the internal carotid artery, oculosympathetic fibers join 6th cranial nerve in the posterior CS for a short distance. Lesions here may affect 6th nerve and sympathetic fibers alone. Although such lesions will remain unclassifiable as per Jefferson scheme, these will be classified as posterior CSS in Ishikawa scheme. In the current study, we had one patient secondary to carotid aneurysm. Similarly, while patients with isolated maxillary nerve involvement or both maxillary and mandibular nerve involvement would fall into posterior CSS in Ishikawa classification, these will remain unclassified as per Jefferon scheme. Similar results have been reported by other authors.[789]
In the present study, CSS could be classified as anterior, middle, and posterior in 12 (17.8%), 16 (21.9%), and 6 (8.2%) patients, respectively, as per the Jefferson classification and 27 (37%), 27 (37%), and 12 (16.4%) as per Ishikawa classification. Yoshihara et al.[7] showed anterior CS involvement to be the most common (35%) followed by posterior (22%) and middle (10%) as per Ishikawa classification. The difference between above series and ours is likely related to the different etiological profile of CSS in these series.
Using Jefferson classification, middle CSS was significantly associated with the presence of fungal infections (P = 0.045). Using Ishikawa classification, all the patients with vascular etiology has anterior CSS. Overall, inflammatory causes were the most common cause for anterior CSS, while tumors accounted for maximum cases of posterior CSS, although the difference was not statistically significant. The explanation for these observations is straightforward. Anterior CS is likely to be affected by inflammatory pathologies more often due to its close proximity to ethmoid sinus (most common site of paranasal sinusitis), while posterior CS is likely to be affected by tumors especially pituitary adenomas due to anatomical reasons. Our findings are similar to Yoshihara et al.,[7] who reported inflammation to dominate in anterior CSS and tumors to dominate in posterior CSS.
CONCLUSION
Our study further emphasizes that many more patients with CSS can be classified using Ishikawa scheme as compared to Jefferson scheme. However, when it comes to etiological profile of CSS, Ishikawa classification did not score over Jefferson scheme. In fact, Jefferson scheme gave a better idea to etiology as middle CSS in this scheme had a significantly higher chances of fungal CSS.
Main limitation of our study was small sample size. That may be the main reason why some of our results did not reach statistically significance. Future studies with more patients may help to understand the utility of these two classification systems better.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The cavernous sinus syndrome. An anatomical and clinical study. Clin Neurol Neurosurg. 1988;90:311-9.
- [Google Scholar]
- Cavernous sinus syndrome: A series of 126 patients. Medicine (Baltimore). 2007;86:278-81.
- [Google Scholar]
- Lateral sellar compartment O.T. (cavernous sinus): History, anatomy, terminology. Anat Rec. 1998;251:486-90.
- [Google Scholar]
- On the saccular aneurysms of the internal carotid artery in the cavernous sinus. Br J Surg. 1938;26:267-302.
- [Google Scholar]
- Clinical anatomy of the cavernous sinus. Shinkei Ganka (Neuroophthalmol Jpn). 1996;13:357-63.
- [Google Scholar]
- The Ishikawa classification of cavernous sinus lesions by clinico-anatomical findings. Jpn J Ophthalmol. 2001;45:420-4.
- [Google Scholar]
- Studies on the cavernous sinus syndrome 1. Incidence, aetiology and differential diagnosis of infranuclear ophthalmoplegias. Acta Neurol Scand. 1964;40:69-75.
- [Google Scholar]






