Translate this page into:
The effects of needle deformation during lumbar puncture
Address for correspondence: Dr. Hasan Hüseyin Özdemir, Department of Neurology, Dicle University, Diyarbakır, Turkey. E-mail: drhasanh@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The aim of this study is to assess deformation of the tip and deflection from the axis of 22-gauge Quincke needles when they are used for diagnostic lumbar puncture (LP). Thus, it can be determined whether constructional alterations of needles are important for predicting clinical problems after diagnostic LP.
Materials and Methods:
The 22-gauge Quincke needles used for diagnostic LP were evaluated. A specially designed protractor was used for measurement and evaluation. Waist circumference was measured in each patient. Patients were questioned about headaches occurring after LP.
Results:
A total of 115 Quincke-type spinal needles used in 113 patients were evaluated. No deflection was detected in 38 (33.1%) of the needles. Deflection between 0.1° and 5° occurred in 43 (37.3%) of the needles and deflection ≥ 5.1° occurred in 34 patients (29.6%). Forty-seven (41.5%) patients experienced post lumbar puncture headache (PLPH) and 13 (11.5%) patients experienced intracranial hypotension (IH). No statistically significant correlation between the degree of deflection and headache was found (P > 0.05). Epidural blood patch was performed for three patients. Deformity in the form of bending like a hook occurred in seven needles and IH occurred in six patients using these needles. Two of the needles used in three patients requiring blood patch were found to be bent.
Conclusion:
Deformation of needles may increase complications after LP. Needle deformation may lead to IH. In case of deterioration in the structure of the needle, termination of the puncture procedure and the use of a new needle could reduce undesirable clinical consequences, especially IH.
Keywords
Headache
intracranial hypotension
Lumbar puncture
needle deflection
Introduction
Lumbar puncture (LP) is performed for a variety of reasons including spinal anesthesia, intrathecal drug administration, myelography, sample collection, pressure measurement and cerebrospinal fluid (CSF) collection. Complications such as headache, labyrinthine and ocular cranial nerve disorders, meningitis, subdural hematoma and fistula can occur.[12] Post lumbar puncture headache (PLPH) may be associated with age, sex, pregnancy, needle diameter, needle type, PLPH history, needle tip deflection, dural entrance angle, and the number of LPs.[3] Age, gender, pregnancy, and PLPH history are risk factors that cannot be changed, however the size and proper shape of the dural tear can be changed with correct needle usage. Although tear size has been associated with the frequency and severity of PLPH, previous studies have not evaluated the shape of the tear. Nonetheless, dural tears have been examined after upright input position and parallel input position into the spinal axis (axle) of the needle in cadavers.[4]
Intracranial hypotension (IH) is a clinical condition which presents with orthostatic headache and is characterized by low CSF pressure and pakimeningeal-dural thickening that can be detected by cranial magnetic resonance imaging (MRI).[56] In particular, IH may develop after LP and spinal anesthesia. The aim of this study is to evaluate the possible relationship between changes occurring in LP needles complications arising after LP by assessing the needles.
Materials and Methods
This study evaluated needles used in LP in the Department of Neurology at Fύrat and Dicle University Hospital from April 2012 to February 2014. The LP procedure was performed in the left lateral position without the use of local anesthesia in all patients. We evaluated needles used during LP for the purpose of diagnosis of patients admitted for various neurological symptoms. The study group included patients from whom approximately 5-10 ml CSF samples were collected. Only 22-gauge Quincke-type spinal needles were included in the study. The spinal needles were 8.9 cm long. Adherent labels indicating patient information were used to link the used needles to the patient medical history.
An angle meter (protractor) specially designed for measurement and evaluation processes of the 9 cm needles was used to evaluate the needle deflection [Figure 1]. The transparent holding portions of each pin were placed on the mid-point of the horizontal and vertical axes of the protractor and needle deflection was examined objectively using the point lines to detect deviation from the vertical axis.
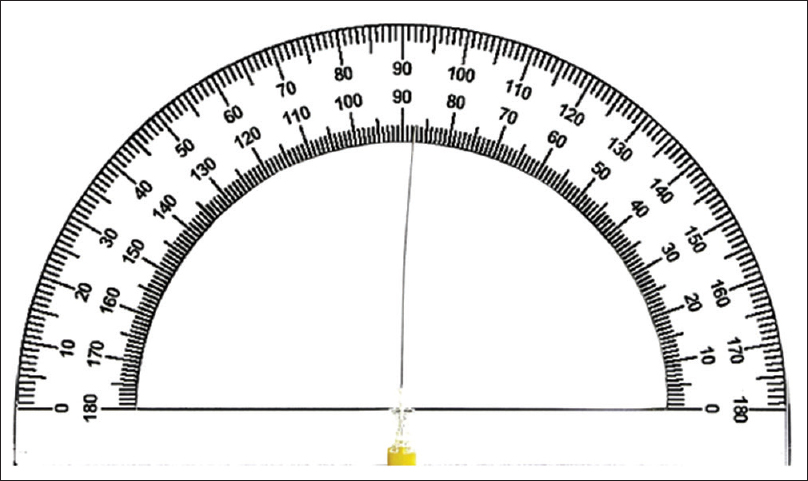
- Angle meter (protractor)
Waist circumference was measured in each patient. The measurement was made by ensuring that the tape measure ensured full contact with the body and did not shift during measurement. The measured values were recorded in centimeters. Puncture operations were performed by neurologists. All patients were hospitalized for at least 2 days after the puncture operation. Bed rest in the recumbent position was recommended. Patients were followed up on an outpatient basis for 1 month following discharge.
Patients were questioned regarding headache symptoms before and after the LP operation. Brain MRI and venography were performed for patients with IH criteria. Starting 1 week after the puncture procedure, patients were contacted by telephone once per week for a month and questioned regarding headache symptoms, in particular, the association between position (lying, sitting or standing) and headache symptoms. Patients diagnosed with IH according to imaging and clinical characteristics were followed up and treated. Puncture site pain and other symptoms were also evaluated.
Statistical analysis
All statistical analyses were conducted using the SPSS for Windows 16.0 statistical software package. Data distributions were evaluated using the Kolmogorov–Smirnov test. Student's t-test and Spearman correlation tests were used to compare difference between independent groups. Experimental values are expressed as mean ± standard deviation (SD). A P value of less that 0.05 was considered statistically significant.
Results
Evaluation of patients
A total of 113 patients and 115 Quincke-type needles were evaluated in the study. The mean age of patients was 24.66 ± 6.9 years (min-max 14-64 years). According to PLPB criteria specified in the second edition of the International Classification of Headache Disorders, typical PLPH was detected in 47 (41.5%) patients.[5] Thirteen (11.5%) cases of IH were observed according to the same criteria. Bed rest, hydration and conservative treatment with analgesics were applied in the patients with PLPH. Intravenous fluid therapy and analgesic treatments were applied in 13 patients with IH. Complete clinical improvement was achieved with conservative treatment in 10 patients. CT-myelography was planned in three patients whose condition did not improve with conservative treatment and had dural thickening. Blood patch was applied to two patients whose leak locations were identified and one patient whose location of leak was not identified. Complete clinical improvement was achieved in all three patients. An autologous epidural blood patch was applied in patients who did not respond to conservative treatment. 10-20 ml of autologous venous blood was injected into the epidural space with an 18-gauge needle to the level at which the CSF leak was present.
Evaluation of used needles according to age and waist circumference
A total of 115 Quincke-type spinal needles used in 113 patients were evaluated. Two of these needles were used for repetition of failed puncture operations in two patients. Mean patient waist circumference was 78.8 ± 8.44 cm (min-max 55.0 to 99.0). No evidence of needle deflection was detected in 38 (33.1%) of 115 needles. Deviation between 0.1° and 5° was detected in 43 (37.3%) patients and deviation greater than 5.1° was detected in 34 (29.6%) patients. The mean age and waist circumference were 21.8 years and 71.5 ± 7.15 cm, respectively, among the patients for whom needle deflection was observed. The means waist circumference and age were 80.7 ± 5.8 cm and 24.4 years, respectively, among the patients where needle deflection occurred between 0.1° and 5°. The mean waist circumference and age were 84.6 ± 6.5 cm and 28.0 years, respectively, among patients for whom deflection occurred greater than 5.1°. A statistically significant positive correlation between age and needle deflection was observed (P < 0.05). There was no significant difference in mean age between patients with headache symptoms and those who did not have headaches (P > 0.05). The degree of needle deflection was positively correlated with the waist circumference (P < 0.05). There was no statistically significant correlation between the degree of deflection and headache symptoms (P > 0.05).
Hook-like or other non-angular deformations occurred in seven needles. Outward curls occurred in four of these needles and inward curls were seen in three of needles [Figure 2a and b]. IH occurred in six patients treated with needles with hook-like deformations. One curved needle was associated with a patient diagnosed with PLPH. Outward hook-like deformations were seen in two needles used in three patients requiring blood patch and who were diagnosed with IH.
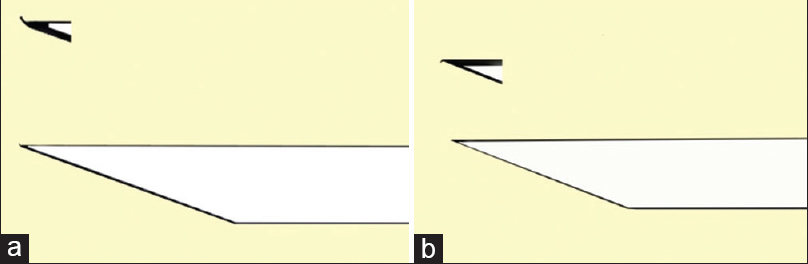
- (a) The curl outward. (b) The curl inward
Discussion
Although the use of LP for diagnostic purposes is a reliable process, some potential complications persist including PLPH. PLPH develops in approximately 30-40% of cases of diagnostic LP.[6] In the present study, PLPH was observed in 41% of cases, consistent with the literature.
Lybecker et al.[7] evaluated multiple factors predicting PLPH resulting from the use of 22, 25 and 26-gauge cutting needles, and determined by regression analysis that caliber was not a predictive factor for PLPH. The anesthesia literature has shown conclusively that atraumatic needles significantly reduce incidence of PLPH compared to the cutting Quincke-type needles typically used by non-anesthesia practitioners. Neurology residents can successfully adopt the atraumatic needle as standard of care for LPs.[8910] As a result of the potential relationship between LP side effects and needle diameter and needle type (2), only 22-gauge Quincke-type needles were used in the present study group. Deflection occurred in 66.9% of needles. The association between needle deflection and PLPH has not been previously evaluated.[11] Although a number of cases of PLPH were associated with needle deflection in the present study, we also observed numerous cases of PLPH that were not associated with PLPH. However, the effects of needle deflection may vary according to anatomical location.
Anatomical midline localization is difficult in patients with high waist circumference.[13] The depth at which CSF is collected in LP procedures increases in proportion with waist circumference. Moreover, increased needle deflection may be expected with increased waist circumference and epidural depth. We observed a significant increase in deflection angle associated with increasing waist circumference.
In a study made by Boon et al., width and height of the interlaminar space decreased with age according to measurements obtained by anterior–posterior lumbar spine radiographs.[12] Failed attempts (dry tap) are generally the result of the fact that the patients lose correct positioning and the direction of the needle is altered.[1] The position relative to the bone structure may also be a factor in failed LP attempts. Twisting of the needle is likely once contact with the bone structure has been made, particularly with the Quincke-type needle. The deflection ratio was associated with increasing age in the present study.
IH is a disorder caused by brain descent due to a CSF leak resulting from diagnostic, therapeutic or spontaneous lesions.[12] There is strong evidence indicating that most cases of IH result from a persistent CSF leak. These leaks most commonly occur after dural puncture for diagnostic LP, myelography, or spinal anesthesia.
Full flexion of the knees and neck can cause the elastic fibers in the dura to be stretched to provide space for the expansion of the interlaminar area. This can lead to resistance against the needle and a tent effect during entry.[4] In cases where the entry angle of the needle into the dura is perpendicular, a tent (flap-valve) effect will be seen [Figure 3]. If the tip of the needle becomes hook-like, this tent effect may be more pronounced. In these cases dural damage can result. This state may increase CSF leakage volume and duration, leading to PLPH and IH. Tears formed at the site of needle entry were examined in detail in the cadaveric studies by Reina et al.[4] Accordingly, the shape of the tear varies according to the entry of the needle in parallel or perpendicular to the axis of the spinal cord. However, the presence of irregular tearing has not been associated with hook-like distortions of the needle. In the present study, hook-like deformities were observed in needles used in six patients who developed IH and in two of three patients requiring autologous blood patch. We propose that hook-like needle deformations are more likely to cause these complications. Use of a new needle following contact with bone structures may prevent the development of IH in LP patients.
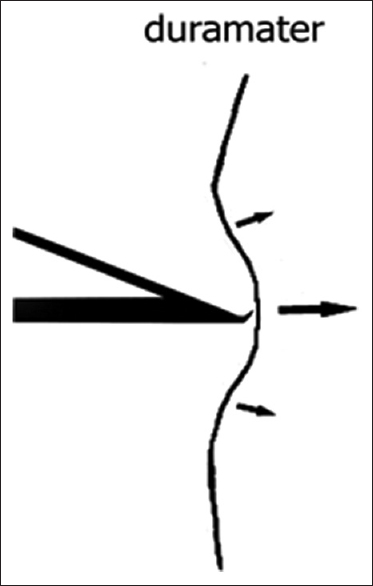
- Tent (flap-valve) effect
A limitation of the present study is the measurement of needle deflection at the level of CSF collection. Previous studies have reported that the deviation is proportional to the penetration depth of the needle.[1314] However, if waist circumference is proportional to the depth of CSF collection, the depth of needle penetration and the deviation may be proportional.[11] In this study, we observed that needle deflection had no effect on the development of PLPH, but that needle deformation may contribute to the development of IH. On the other hand, multiple meta-analyses have consistently demonstrated that needle caliber is a significant risk factor in the development of PLPH.[10]
As a result, we recommend the use of a new needle during LP in any case where needle axis deviation may have occurred, particularly cases in which hook-like deformations are possible. This change in practice may result in fewer unintended complications of LP, including IH.
Acknowledgments
We are grateful to Dicle University DUBAP for their sponsorship about English editing of this manuscript.
Source of Support: Nil
Conflict of Interest: None declared.
References
- The clinical anatomy of several invasive procedures. American Association of Clinical Anatomists, Educational Affairs Committee. Clin Anat. 1999;12:43-54.
- [Google Scholar]
- Dura-arachnoid lesions produced by 22 gauge Quincke spinal needles during a lumbar puncture. J Neurol Neurosurg Psychiatry. 2004;75:893-7.
- [Google Scholar]
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. In: Cephalalgia Vol 24. (2nd ed). 2004. p. :9-160.
- [Google Scholar]
- Postdural puncture headache: Diagnosis, prevention and therapy. Schmerz. 1999;13:332-40.
- [Google Scholar]
- Postdural puncture headache is a risk factor for new postdural puncture headache. Cephalalgia. 2008;28:5-8.
- [Google Scholar]
- Postdural puncture headache and spinal needle design. Metaanalyses. Anesthesiology. 1994;81:1376-83.
- [Google Scholar]
- Education research: Changing practice. Residents’ adoption of the atraumatic lumbar puncture needle. Neurology. 2013;80:e180-2.
- [Google Scholar]
- Post-dural (post-lumbar) puncture headache: Risk factors and clinical features. Cephalalgia. 2012;32:916-23.
- [Google Scholar]
- The effects of needle type, gauge, and tip bend on spinal needle deflection. Anesth Analg. 1996;82:297-301.
- [Google Scholar]
- Intracranial hypotension syndrome: A post dural puncture headache? Rev Colomb Anestesiol. 2013;41:57-60.
- [Google Scholar]
- Diagnostic lumbar puncture. Comparative study between 22-gauge pencil point and sharp bevel needle. J Headache Pain. 2005;6:400-4.
- [Google Scholar]






