Translate this page into:
Pain outcome of non-instrumented lumbar decompressive surgery for degenerative lumbar spine disease using patient-reported pain outcome instruments
*Corresponding author: Moses Osaodion Inojie, Department of Surgery, Federal Medical Centre, Asaba, Delta State, Nigeria. mosege2000@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Inojie MO, Ndubuisi CA, Okwunodulu O, Inojie OV, Ndafia NM, Ohaegbulam SC. Pain outcome of non-instrumented lumbar decompressive surgery for degenerative lumbar spine disease using patient-reported pain outcome instruments. J Neurosci Rural Pract. 2024;15:47-52. doi: 10.25259/JNRP_80_2022
Abstract
Objectives:
A clinical disorder known as degenerative lumbar spine disease (DLSD) is characterized by persistent low back pain (LBP) coupled with radiculopathy and other signs of neurologic impairment. Using patient-reported pain outcome assessment tools, this study evaluated the pain outcome of non-instrumented lumbar decompressive surgery for DLSD.
Materials and Methods:
A prospective longitudinal research was conducted. Using the metric visual analog scale (VAS) score and the Oswestry disability index (ODI), consenting patients who underwent non-instrumented lumbar decompressive surgery for symptomatic DLSD were evaluated for radicular pain and LBP. The evaluation was conducted both immediately before surgery and 6 months after surgery. Data generated by comparing the pre-operative and post-operative VAS and ODI scores were then analyzed using descriptive and inferential statistics.
Results:
Sixty-seven patients in total completed the study. Thirty-six (54%) males and 31 (46%) females, with a mean age and body mass index of 55.28 years and 29.5 k/m2, respectively. At 6 months postoperatively, there was significant pain reduction from the pre-operative baseline VAS for LBP (67.12–32.74) with P < 0.001, VAS for radicular pain (75.39–32.75) with P < 0.001, and ODI (65.30–27.66) with P < 0.001. There was a greater decrease in radicular pain than in LBP following lumbar decompressive only surgery (P = 0.03).
Conclusion:
Patients with symptomatic DLSD and high pre-operative back pain scores without considerable listhesis should anticipate a significant reduction in radicular and back pain intensity, as well as pain-related functional disability, 6 months after non-instrumented lumbar decompressive surgery.
Keywords
Degenerative lumbar spine disease
Decompressive surgery
Pain outcome
INTRODUCTION
Chronic low back pain (LBP) with radiculopathy and other signs of neurologic dysfunction is a characteristic of degenerative lumbar spine disease (DLSD), a clinical disorder. The pain associated with DLSD is among the most common reasons that patients with this condition seek expert neurosurgical consultation.[1,2] There have been reports of a 60–90% lifetime incidence of LBP worldwide.[3] A comprehensive analysis carried out in Africa revealed that the lifetime prevalence of LBP ranged from 28% to 74%.[4] The most frequent cause of LBP worldwide and a major contributor to morbidity and disability is DLSD.[3,5]
Patients who have failed conservative treatment for LBP or radiculopathy, sphincter dysfunction, and motor impairments typically present for lumbar decompressive surgery for DLSD. The primary goal of treatment is to enhance health-related quality of life by reducing pain intensity and pain-related impairment; therefore, pain evaluation is a crucial component of determining how well lumbar spine surgery works. Aspects such as pain severity, pain duration, and pain-related disability characterize pain and its impacts.[6,7] In some cases, surgical decompression has been demonstrated to be more effective than conservative treatments for these indications. However, researchers have disagreed on the level of pain reduction after surgical decompression.[1,8,9]
Depending on how surgical success is determined, a good surgical outcome can be defined. In the past, surgeons’ subjective opinions were frequently used to evaluate outcomes, and the outcomes were graded using phrases such as “excellent,” “good,” “moderate,” and “bad.” These classification systems were also influenced by the technical success of the procedure in terms of decompression, as determined by imaging tests done during the patients’ follow-up appointments.[10] The opinions of surgeons and the outcomes of imaging tests, however, usually do not correspond with patients’ satisfaction. In this perspective, the patient’s assessment of the outcomes obtained from patient-reported outcomes (PRO) instruments should be the best indicator of the quality of the treatment. The PRO instruments commonly used to assess pain intensity and pain-related functional disability are the visual analog scale (VAS) and the Oswestry disability index (ODI), and they are considered the “gold standard” for assessing LBP.[10-13]
A study of the literature turned up some reports on pain management after surgical decompression for DLSD in Western countries. However, the majority of these investigations are retrospective and lack appropriate biostatistical techniques.[2,8,14-16] At the same time, studies have shown that perceptions of pain and behaviors associated with it are influenced by the sociocultural context of the individuals experiencing them and that there are significant ethnic differences in pain tolerance.[17,18] Furthermore, in the research setting, patients with LBP and leg pain from DLSD typically come to hospitals late, delaying diagnosis for a number of reasons, including a lack of resources and ignorance. They frequently suffer from more serious diseases and have tried numerous analgesics and other drugs in extremely high quantities to ease their pain. As a result, the results of the pain assessment following lumbar decompressive surgery for DLSD in one research population could not entirely address the results of the pain evaluation in other populations.
Hence, this study assessed the pain outcome of non-instrumented lumbar decompressive surgery for DLSD using patient-reported pain outcome assessment tools in our study environment.
MATERIALS AND METHODS
In this prospective study, 67 patients who underwent DLSD surgery at the Memfys Hospital for Neurosurgery (MHN), Enugu, Nigeria, between 2018 and 2020 are included in the study.
The clinical and radiological evaluation of patients 40 years of age and older who presented to MHN with symptoms suggestive of DLSD (conventional radiography and magnetic resonance imaging/computed tomography [CT] of the lumbar spine) led to the diagnosis of DLSD with compression of the neural elements without significant spondylolisthesis (less than grade II listhesis). Those who qualified for non-instrumented lumbar decompressive surgery had their surgical fitness assessed. Patients were serially included in the study after gaining a surgical fitness confirmation, meeting the inclusion requirements, and providing written informed consent for both surgery and the research. Each patient’s pre-operative pain was evaluated using VAS and ODI for LBP, radicular pain, and pain-related functional impairment.
A neurosurgical team made up of neurosurgeons, neurosurgery residents, anesthesiologists, and perioperative nurses performed non-instrumented lumbar decompressive procedures. At the various levels of interest, patients received open spine surgery that included lumbar laminectomy, ligamentum flavum excision, discectomy, lateral recess decompression, and exit foraminotomy. It is important to note that the use of any of the above surgical methods in combination was contingent on the location and nature of the neurological compression.
Following surgery, patients were observed for 6 months. Their post-operative pain was assessed again using VAS and ODI 6 months after surgery.
The IBM SPSS version 20 statistical tool for the social sciences was used to analyze the data. Frequencies were used to represent categorical variables while averages and standard deviations were used to represent continuous variables. The difference in means between the pre-operative and postoperative VAS and ODI scores was analyzed using a paired sample t-test. P < 0.05 was regarded as significant.
By comparing the VAS and ODI values before and 6 months after decompressive surgery, the pain outcome was determined.
Exclusion criteria
The following criteria were excluded from the study:
Patients with grade II or higher lumbar spondylolisthesis
Patients with lumbar scoliosis, whether it is congenital or acquired
Individuals who have had lumbar fusion or fixation procedures
Those who underwent lumbar spine decompression on three or more levels, as this may raise the risk of iatrogenic spondylolisthesis
Those who have previously undergone spinal surgery
People who have advanced osteoporosis, as shown by poor bone mineral density on a lumbar CT scan done before surgery.
RESULTS
A total of 67 patients completed the study with 36 (54%) males and 31 (46%) females. The mean age of the study population was 55.28 years, and the mean body mass index was 29.60 kg/m2 [Table 1].
| Groups categories | Total No. n (%) | Mean±SD | Chi-square (χ2) | P-value |
|---|---|---|---|---|
| Sex | ||||
| Male | 36 (54) | 0.541 | ||
| Female | 31 (46) | 0.373 | ||
| Mean age | 55.28±10.58 | |||
| BMI | ||||
| <30 kg/m2 | 37 (55.2) | 0.392 | ||
| ≥30 kg/m2 | 30 (44.8) | 0.731 | ||
| Mean BMI | 29.60±5.32 | |||
| Radiculopathy locations | ||||
| Right | 14 (20.9) | 0.008* | ||
| Left | 19 (28.4) | |||
| Bilateral | 34 (50.7) | 9.701 |
SD: Standard deviation, BMI: Body mass index. *Significant P-value. Pearson Chi-square χ2 (1, n=67) test applied. There was no significant difference in the proportion of males versus females, or obese versus non-obese. Bilateral radicular pain was the most common pattern of presentation, and this was statistically significant (P=0.008)
The mean duration of low back and radicular pains was 38.39 and 23.58 months, respectively [Figure 1].
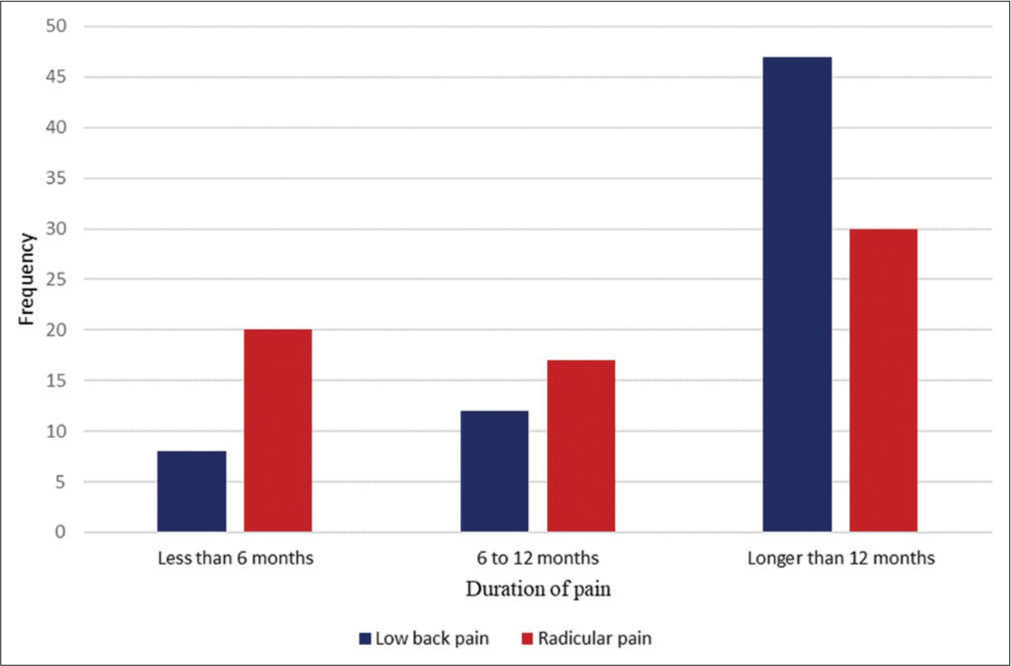
- The pre-operative duration of the axial and radicular pain in the subjects.
At 6-month postoperatively, there was significant pain reduction from pre-operative baseline VAS for LBP (67.12–32.74), VAS for radicular pain (75.39–32.75), and ODI (65.30–27.66) with P < 0.001 [Table 2].
| Mean pre-op scores |
Mean post-op scores |
Mean difference in scores | SE | 95%CI | t-value | P-value | |
|---|---|---|---|---|---|---|---|
| VAS-LBP (mm) | 67.12 | 32.75 | 34.37 | 2.93 | (28.51–40.23) | 11.71 | <0.001* |
| VAS-RP (mm) | 75.39 | 32.48 | 42.91 | 3.13 | (36.66–49.16) | 13.71 | <0.001* |
| ODI (%) | 65.30 | 27.66 | 37.64 | 2.26 | (33.13–42.14) | 16.67 | <0.001* |
VAS: Visual analog scale, ODI: Oswestry disability index, LBP: Low back pain, RP: Radicular pain, SD: Standard deviation, SE: Standard error, CI: Confidence interval, pre-op: Pre-operative, post-op: Post-operative. *Significant P-value. A paired sample t-test was applied. The mean pre-operative VAS score for low back pain was 67.12 (SD=15.54); the score decreased after surgery to a mean of 32.75 (SD=20.42). This decrease was statistically significant, P<0.001. The mean pre-operative VAS score for the radicular pain was 75.39 (SD=14.92) while it decreased to 32.48 (SD=22.93) after the surgery, P<0.001. The mean pre-operative ODI score was 65.30 (SD=17.23), while the post-operative score was 27.66 (SD=15.97), P<0.001
Radicular pain was more significantly reduced than LBP by lumbar decompression surgery (P = 0.03) [Figure 2].
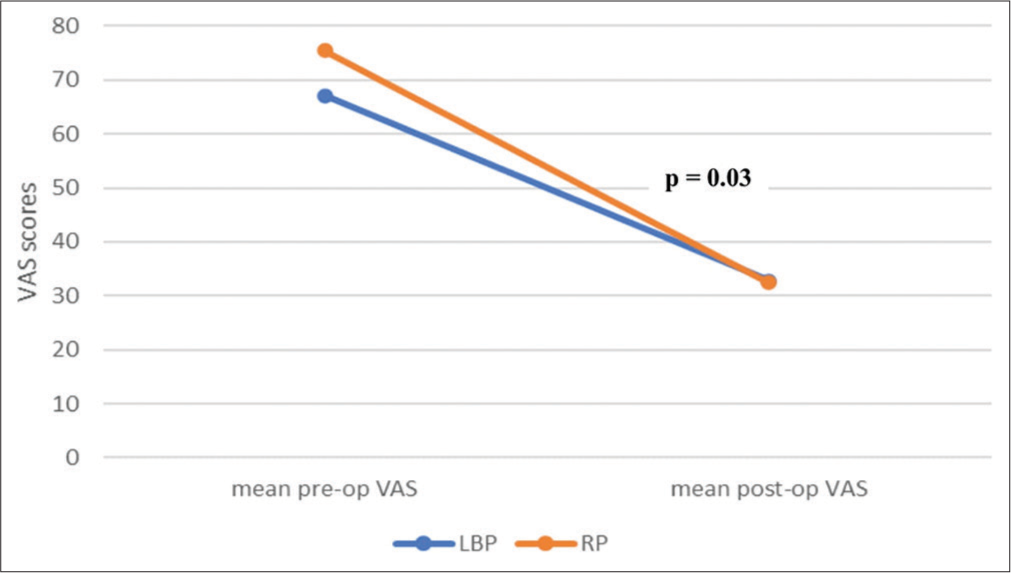
- A line graph comparing the difference between pre-operative and 6-month post-operative VAS scores for low back pain and radicular pain. VAS: Visual analog scale.
DISCUSSION
The VAS and ODI pain assessment instruments, which have good test-retest reliability and validity in assessing pain, were employed in this study to evaluate the efficacy of lumbar decompressive surgery for DLSD in controlling patients’ pre-operative pain.[13,19]
The pre-operative baseline mean VAS ratings for LBP, radicular pain, and ODI in this study were 67.12, 75.35, and 65.30, respectively. These were considered high in comparison to research of a comparable nature conducted in western climates when pre-operative pain levels at baseline were lower.[9,20] This suggests that patients in the index study environment had more severe pain-related symptoms. This might be because of disparities between this study environment and Western society in terms of patients’ genetics, demography, socioeconomic level, and health-care system. Patients in this study also experienced persistent chronic symptoms, with a mean duration of 38.39 months. This delayed presentation could be due to patients’ concerns about the benefits of decompressive surgery. This could also explain why the index study had greater pre-operative pain levels. A better comparison would have been with studies from other African populations due to genetic and socio-demographic commonalities among Africans. However, similar studies in Africa available in the literature did not employ PRO pain measurement techniques, making appropriate comparison difficult.[21,22]
The post-operative reduction in VAS scores demonstrated improvements in patients LBP and radicular pain in the index study. The patient’s LBP had a mean pre-operative baseline VAS score of 67.12. After 6 months, the score had dropped to a mean of 32.75. Furthermore, the mean pre-operative baseline VAS score for radicular pain was 75.39, which dropped to 32.48 6 months after surgery. At the same time, there was a reduction in patients’ pain-related functional disability, with the mean pre-operative baseline ODI score dropping from 65.30 to 27.66 6 months after surgery. There was a statistically significant reduction in the intensity of LBP, radicular pain, and pain-related functional disability after lumbar decompression for DLSD, as the resultant mean change in VAS for LBP, VAS for radicular pain, and ODI were 34.37, 42.91, and 37.42, respectively. Furthermore, the mean change in ODI in the current study is well above the cutoff value for the minimum clinically important difference (MCID) for the ODI in lumbar spine surgery patients based on the previous studies.[16,23,24] The MCID cutoff value for ODI is frequently interpreted as a significant change in clinical improvement or deterioration. Most Western studies reported a cutoff in the range of 8–10 points change in the ODI for patients with lumbar spinal stenosis undergoing decompressive surgery without instrumentation, which is well below the findings from the index study, which reported a 37.42 mean point change in the ODI.[16,23] Therefore, lumbar decompressive surgery effectively controlled patients’ pain and pain-related disability in this study population.
This large improvement in patient satisfaction could be attributed to optimal patient selection, which is the result of accurate diagnosis, localization, and precise surgical decompression of the afflicted spine. However, because the study analyzed the outcome at 6 months post-surgery, this assessment is only in the medium term and should not be used as a reference for a long-term outcome, as this cannot be extended to a long-term (up to 5 years’ post-surgery) gain in patients’ pain control. Furthermore, a European study found some deterioration in pain levels after 5 years following surgery, despite the fact that pain was still greatly reduced from the baseline level.[25] Hence, a lengthier follow-up research of up to 5 years after surgery in the study population may be useful in determining whether these improvements are sustained in the long term. Additional research may be required to identify a cutoff value in MCID for ODI in this study population.
Some research in Western countries found a similar pattern of improvement.[9,20,25,26] However, the level of pain control varied. A Norwegian population with DLSD who underwent lumbar decompressive surgery saw a considerable reduction in their VAS and ODI scores following surgery, according to a study conducted by Jakola et al. At 12 months, the mean change in VAS scores for LBP, radicular pain, and ODI scores was 19.80, 26.60, and 10.60, respectively, which was lower than the results obtained in the current study (34.37, 42.91, and 37.42, respectively) at 6 months. This Norwegian trial, however, was limited to older patients over the age of 70, and post-operative pain assessment was performed 12 months following surgery, which differed slightly from the approach used in the index study. When studies from several European and American countries were compared, a similar pattern of difference in pain control was observed.[9,20,25,26] Compared to the existing literature, participants in the index study had significantly better pain control following surgery. This could be attributed in part to the current study’s stringent patient selection strategy. Furthermore, patients in the index trial had more advanced disease, as evidenced by very high pre-operative baseline VAS and ODI ratings. This could have resulted in the impressive pain reduction reported following surgery, and as such, it portrays surgery’s role as efficiently reducing patients’ pain in the medium term. Furthermore, several researches discovered a clear relationship between high pre-operative ODI levels and a more dramatic postoperative reduction in ODI.[16,27] It’s so remarkable that, despite their extreme pre-operative pain symptoms, patients in our society can expect a significant improvement in pain after 6 months of surgery.
Some African studies on lumbar decompression for DLSD, such as Andrew et al. in Ghana and Sherif in Egypt, reported a considerable reduction in pain, but PRO pain evaluation tools were not employed in these studies. As a result, comparing their level of pain control to the index study becomes challenging.[21,22]
The results of the current study also suggest that a high level of pre-operative LBP (VAS > 50 mm) should not be a contraindication to non-instrumented decompression surgery in patients who otherwise are candidates for surgical decompression for symptomatic DLSD. The mean pre-operative VAS score for the LBP in the current study was 67.12 mm. The score decreased to a mean of 32.75 mm 6 months after surgery. This showed significant LBP reduction despite the high pre-operative value. Although radicular pain had a better 6-month post-operative VAS score reduction than LBP, with a mean change in VAS score of 42.91 and 34.37, respectively, patients with severe LBP also clinically improved in other pain outcome measures, including ODI. This finding contradicts Kleinstück et al., previous observation that a high pre-operative LBP score is a poor prognostic factor and/or a contraindication to decompression-only surgery without instrumentation.[28] The index study’s findings suggest that such existing assumptions should be reconsidered. Hence, in properly selected patients with symptomatic stenosis and severe radiculopathy coexisting with severe pre-operative LBP, considerable back pain relief can be obtained with decompression-only surgery. This is substantiated by studies conducted by Crawford et al. in 2016 and Röder et al. in 2015, in which individuals with dominant LBP symptoms saw considerable pain reduction after 1 year of surgery following a decompression-only operation.[26,29] Nonetheless, more research may be required to identify the specific pre-operative factors that predict decompression-only surgery failure and thus justify the increased complexity and cost of fusion or stabilization during surgical decompression for DLSD in the absence of significant spondylolisthesis or scoliosis.
CONCLUSION
According to the index study, individuals with symptomatic DLSD and severe back pain who do not have considerable spondylolisthesis can significantly reduce their low back and radicular discomfort with lumbar decompression-only surgery. The results of this study offer valuable knowledge that may help spine surgeons when advising patients with DLSD regarding post-operative pain outcomes before surgery.
Study strengths and limitations
The adoption of precise inclusion and exclusion criteria, a very low loss to follow-up, and the appropriate application of PRO instruments enhanced the findings in the current investigation. However, the following represent a few study limitations:
Subjective tools are currently used to assess pain in general, including this study. The ability to accurately assess pain using derived objective techniques is currently lacking
The follow-up period was only 6 months long. Results from 6 months afterward were not included in this study.
Ethical approval
The study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Five-year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. 2010;19:1883-91.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and surgical outcomes after lumbar laminectomy: An analysis of 500 patients. Surg Neurol Int. 2015;6:S190-3.
- [CrossRef] [PubMed] [Google Scholar]
- Vital statistics of the United States Washington, DC: Government Printing Office; 1988. p. :208-12.
- [Google Scholar]
- The prevalence of low back pain in Africa: A systematic review. BMC Musculoskelet Disord. 2007;8:105.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology: The magnitude of the problem In: Wiesel SW, Weinstein JN, Herkowitz HH, Dvorak J, eds. The lumbar spine. Vol 2. Philadelphia, PA: WB Saunders Company; 1996. p. :14-28.
- [Google Scholar]
- Complications and outcomes of lumbar spine surgery in elderly people: A review of the literature. J Am Geriatr Soc. 2008;56:1318-27.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of surgical treatment of degenerative lumbar stenosis. MJSBH. 2015;14:7-10.
- [Google Scholar]
- Why and how should we measure outcomes in spine surgery? J Taibah Univ Med Sci. 2016;11:91-7.
- [CrossRef] [Google Scholar]
- The oswestry low back pain disability questionnaire. Spine (Phila Pa 1976). 2001;25:2940-53.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of pain rating scales by sampling from clinical trial data. Clin J Pain. 2000;16:22-8.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol. 1990;17:1022-4.
- [Google Scholar]
- A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med. 2016;374:1413-23.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of surgery for lumbar spinal stenosis: A systematic review and meta-analysis. PLoS One. 2015;10:e0122800.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of getting dorse: Predictors of deterioration after decompressive surgery for lumbar spinal stenosis: A multicenter observational study. World Neurosurg. 2015;84:1095-102.
- [CrossRef] [PubMed] [Google Scholar]
- Ethnic differences in pain tolerance: Clinical implications in a chronic pain pop-ulation. Psychosom Med. 2001;63:316-23.
- [CrossRef] [PubMed] [Google Scholar]
- Inter-ethnic differences in pain perception. Pain. 1991;44:157-62.
- [CrossRef] [PubMed] [Google Scholar]
- Roland-Morris disability questionnaire and oswestry disability index: Which has better measurement properties for measuring physical functioning in nonspecific low back pain? Systematic review and meta-analysis. Phys Ther. 2016;96:1620-37.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes and safety assessment in elderly patients undergoing decompressive laminectomy for lumbar spinal stenosis: A prospective study. BMC Surg. 2010;10:34.
- [CrossRef] [PubMed] [Google Scholar]
- Long term results of decompressive laminectomy in treatment of lumbar spinal canal stenosis (A thirty years retrospective study) Semant Sch Organ. 2014;1:84-96.
- [Google Scholar]
- Decompressive laminectomy for lumbar stenosis: Review of 65 consecutive cases from Tema, Ghana. West Afr J Med. 2007;26:283-7.
- [CrossRef] [PubMed] [Google Scholar]
- Minimum clinically important difference in lumbar spine surgery patients: A choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008;8:968-74.
- [CrossRef] [PubMed] [Google Scholar]
- Surgery with disc prosthesis versus rehabilitation in patients with low back pain and degenerative disc: Two year follow-up of randomised study. BMJ. 2011;342:2786-91.
- [CrossRef] [PubMed] [Google Scholar]
- The outcome of spinal decompression surgery 5 years on. Eur Spine J. 2007;16:1842-7.
- [CrossRef] [PubMed] [Google Scholar]
- Back pain improvement after decompression without fusion or stabilization in patients with lumbar spinal stenosis and clinically significant preoperative back pain. J Neurosurg Spine. 2016;25:596-601.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of “getting worse” after lumbar microdiscectomy. Eur Spine J. 2005;14:49-54.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of preoperative back pain on the outcome of lumbar decompression surgery. Spine (Phila Pa 1976). 2009;34:1198-203.
- [CrossRef] [PubMed] [Google Scholar]
- Superior outcomes of decompression with an interlaminar dynamic device versus decompression alone in patients with lumbar spinal stenosis and back pain: A cross registry study. Eur Spine J. 2015;24:2228-35.
- [CrossRef] [PubMed] [Google Scholar]






