Translate this page into:
Lumbar facet joint arthrosis on magnetic resonance imaging and its association with low back pain in a selected Ghanaian population
*Corresponding author: Klenam Dzefi-Tettey, Department of Radiology, Korle Bu Teaching Hospital, Accra, Ghana. k.dzefitettey@kbth.gov.gh
-
Received: ,
Accepted: ,
How to cite this article: Dzefi-Tettey K, Edzie EK, Mensah SK, Osei S, Piersson AD, Amedi MK, et al. Lumbar facet joint arthrosis on magnetic resonance imaging and its association with low back pain in a selected Ghanaian population. J Neurosci Rural Pract 2023;14:681-5.
Abstract
Objectives:
Facet joint arthrosis is a common radiologic finding but remains controversial as a source of low back pain. We conducted a study to evaluate some of the potential risk factors contributing to the development of facet joint arthrosis, such as age, gender, and body mass index (BMI). The study aimed at establishing an association between these factors and facet joint arthrosis in the Ghanaian population, as a foundation for further research on low back pain.
Materials and Methods:
This was a retrospective study done at the Department of Radiology, Korle Bu Teaching Hospital from January 2019 to December 2021. The study population included all cases referred to our department with complaints of low back pain. Patients below 18 years and those with a history of congenital lesions, trauma, infection, and malignancies were excluded. A total of 1017 cases were identified with facet joint arthrosis. The mean difference in age and BMI between males and females was compared using an independent sample t-test. Statistical association was done using Pearson’s Chi-square test. P ≤ 0.05 was used as statistical significance.
Results:
Majority of the study subjects were overweight with a mean BMI of 27.31 ± 5.37 kg/m2. The mean age was 53.61 ± 16.22 years, and majority were within the age of 51–60 years. Age was significantly associated with the prevalence of facet joint arthrosis.
Conclusion:
The prevalence of facet joint arthrosis is significantly associated with increasing age but not with the BMI. Lumbar facet joint arthrosis is more prevalent in women than in men, which may be due to the sensitivity of cartilage to female sex hormones.
Keywords
Facet joint arthrosis
Low back pain
Body mass index
Age
Magnetic resonance imaging
INTRODUCTION
Facet joint arthrosis is a degenerative condition that mainly occurs as a result of aging, excessive weight, poor body mechanics, repetitive motion, and minor traumatic events.[1] Some studies have demonstrated a strong correlation between intervertebral disc degeneration (IDD) and facet joint arthrosis, with IDD usually preceding the onset of facet joint degeneration.[2]
A strong positive correlation exists between lumbar facet joint arthrosis and age.[3] Other studies have linked the early onset of facet joint arthrosis in one’s life to the weight of work performed before the age of 20.[4] According to a study by Eubanks et al., nearly 60% of adults demonstrate evidence of degenerative changes before reaching 30 years of age.[5] The degree of severity of lumbar facet joint arthrosis and increasing age has been highlighted in some studies. One study indicated that 67% of individuals aged 45–64 years had moderate lumbar facet joint arthrosis and 89% of individuals aged 65 years and older had severe lumbar facet joint arthrosis.[6]
It has long been proposed that facet joint arthrosis, a frequent radiologic finding, could be a possible source of low back pain;[7] however, controversy surrounds the facet joint as a possible source of low back pain.[8] With a lifetime prevalence of between 70% and 85%, low back pain is arguably one of the chief complaints seen in primary, secondary, and tertiary care facilities.[9] Depending on how long the condition has been present, low back pain can be categorized as acute, subacute, or chronic. With regard to the therapeutic decision-making process, radiological imaging is very crucial to diagnose or rule out pathological conditions of low back pain.
The most common indication for pain in facet joints is arthrosis and can be examined by the use of radiograph, computed tomography scan, or magnetic resonance imaging (MRI).[10] Over the past two decades, significant improvements have been made in radiological examination of the lumbosacral spine.[11] MRI has emerged as one of the preferred imaging modalities in the assessment of back pain due to the absence of radiation use and improved delineation of soft tissues.
The diagnosis of spinal pain resulting from facet joint arthrosis can be challenging. Due to the varied causes of facet joint disorders and the likelihood of a chronic back pain, a precise diagnosis is of utmost importance.[10] This study was carried out to evaluate some potential risk factors that might lead to the development of facet joint arthroses, such as age, gender, and body mass index (BMI). Establishing an association between these elements and facet joint arthrosis could serve as a foundation for additional research on low back pain in the African population.
MATERIALS AND METHODS
Study design
This was a retrospective study involving the review of all lumbar spine magnetic resonance (MR) images of patients referred to the radiology department of the Korle Bu Teaching Hospital on account of low back pain from January 2019 to December 2021. To identify patients who underwent MRI of the lumbar spine for low back pain as a clinical indication, we searched the institutional Picture Archiving and Communication System database after receiving ethical review board approval. We included all lumbar spine images of patients aged 18 years and above and excluded patients with evidence or history of congenital lesions, trauma, infections, and malignancies.
Image evaluation
Two experienced radiologists, each with over 15 years of experience in interpreting spinal images, conducted independent reviews of the MR images. The evaluations were performed to assess for exclusion criteria and to examine all lumbar levels (L1–S1) for the presence of facet joint arthrosis. The diagnosis of facet joint arthrosis was made using criteria consistent with those described by Pathria[12] and Weishaupt.[13]
MRI protocol
The MRI examinations were done on a 1.5 Tesla Toshiba Vantage Titan MRI machine with serial number GH-0029-01-CMR-01 using a surface coil, and patients were scanned in the supine position. Routine lumbar MRI protocol was used; 4-mm sagittal T1 weighted (T1W), coronal T2 weighted (T2W), sagittal T2W, short tau inversion recovery, stacked or contiguous axial T2W, and axial T1W turbo spin-echo sequences. Most of the subjects had been scanned without intravenous (IV) gadolinium, however, if infectious, inflammatory, or neoplastic etiologies were suspected, IV gadolinium was given.
Statistical analysis
The Statistical Package for the Social Science (SPSS Inc., Chicago, IL, USA) version 25.0 was the statistical tool used for statistical analysis. The patients were stratified by age and BMI. The independent sample t-test was used to compare the mean difference in age and BMI between males and females. Pearson’s Chi-square test for association was used to explore any association existing between the various BMI categories and gender. Statistical significance was considered at a P ≤ 0.05.
RESULTS
A total of 1017 out of 2194 lumbar spine images were identified to have facet joint arthrosis of which 50.54% were females. The mean age was 53.61 ± 16.22 years, ranging from 21 to 84 years, with females being younger than males. Both the minimum and maximum BMI were found in females (15.76 kg/m2 and 58.80 kg/m2), respectively. The differences in BMI between males and females were not statistically significant (P = 0.735). On average, we recorded a BMI of 27.31 ± 5.37 kg/m2 [Table 1]. The most frequent level involved was L4/L5 followed by L5/S1 level [Figure 1]. Patients with facet joint arthrosis affecting all lumbar levels were found to be 118 out of 1017 and those involving a single level were 393 out of 1017.
| Male (n=503) | Female (n=514) | P-valueβ | Total subjects | |
|---|---|---|---|---|
| Age (years) | 0.089 | |||
| Min | 21 | 26 | 21 | |
| Max | 84 | 84 | 84 | |
| Mean±SD | 54.49±16.77 | 52.75±15.63 | 53.61±16.22 | |
| BMI (kg/m2) | 0.735 | |||
| Min | 17.10 | 15.76 | 15.76 | |
| Max | 54.58 | 58.80 | 58.80 | |
| Mean±SD | 27.25±5.19 | 27.37±5.55 | 27.31±5.37 | |
| Number of lumbar levels (%) | 0.142 | |||
| 1 | 192 (38.2) | 201 (39.1) | 393 (38.6) | |
| 2 | 68 (13.5) | 79 (15.4) | 147 (14.5) | |
| 3 | 149 (29.6) | 123 (23.9) | 272 (26.7) | |
| 4 | 45 (8.9) | 42 (8.2) | 87 (8.6) | |
| 5 | 49 (9.7) | 69 (13.4) | 118 (11.6) |
SD: Standard deviation, βCompare differences between males and females
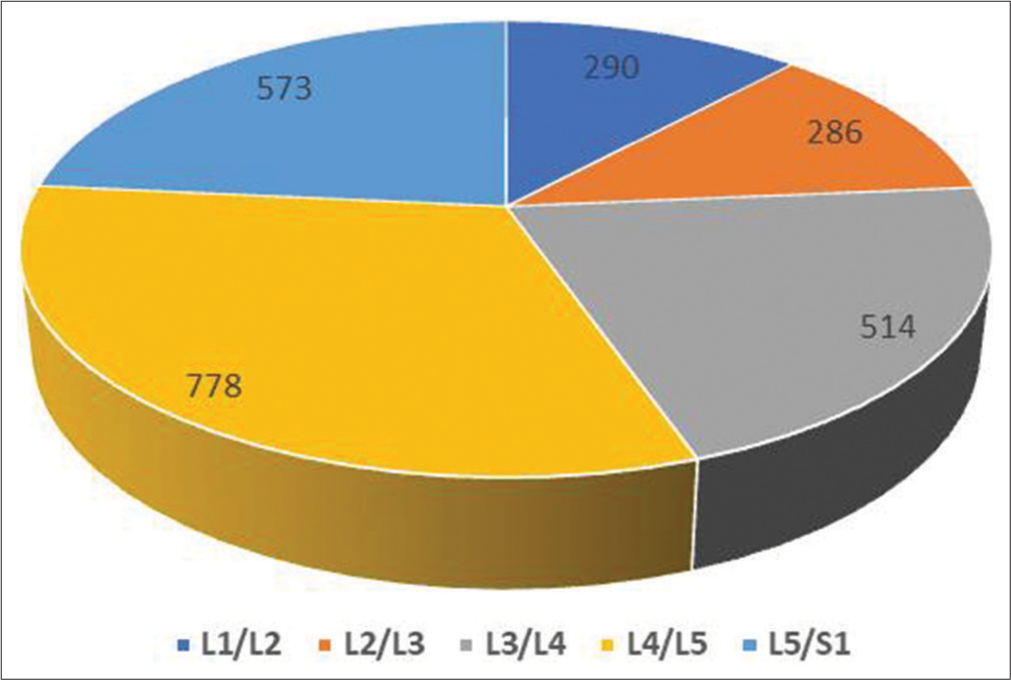
- Distribution of spinal levels involved.
With respect to BMI, most of the patients were overweight (i.e., 368 out of 1017) and few (1.3%) were underweight. Statistically, we found that the prevalence of facet joint arthrosis between males and females did not depend on the BMI of the patient (P = 0.460) [Table 2]. We found an increasing trend in the prevalence of facet joint arthrosis with respect to the different lumbar levels. However, the trend was different in patients who were overweight and obese [Figure 2].
| Male | Female | Total | P-value | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Underweight | 4 (0.8) | 9 (1.8) | 13 (1.3) | 0.460 |
| Normal weight | 179 (35.6) | 184 (35.8) | 363 (35.7) | |
| Overweight | 189 (37.6) | 179 (34.8) | 368 (36.2) | |
| Obesity | 131 (26.0) | 142 (27.6) | 273 (26.8) |
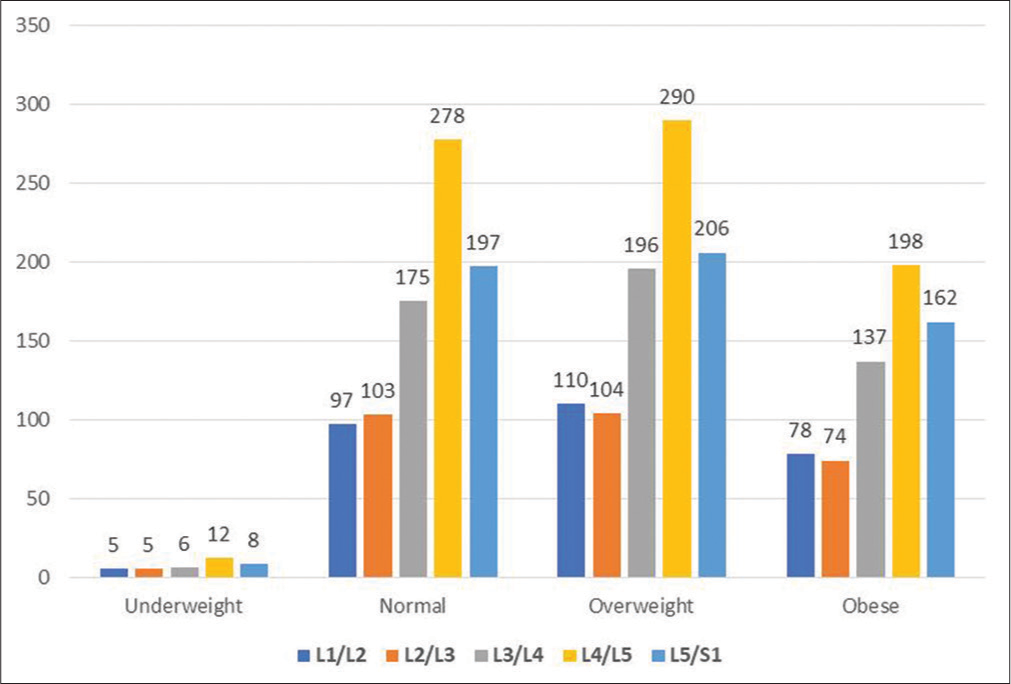
- Distribution of body mass index categories showing the number of facet joint arthrosis at each level.
Individuals within the age of 51–60 years were the dominant group with facet joint arthrosis [Table 3]. Males constituted majority in both the youngest age bracket and the oldest age bracket. Similar to the BMI categories, we found an increasing trend in age and the prevalence of patients with facet joint arthrosis up to the age of 60. At a P = 0.033, the increasing trend between males and females significantly depends on the age groupings. There was facet joint arthrosis at all levels in all the age groups [Figure 3].
| Age group | L1/L2 (%) | L2/L3 (%) | L3/L4 (%) | L4/L5 (%) | L5/S1 (%) | Total (%) |
|---|---|---|---|---|---|---|
| 20–30 | 24 (25.5) | 25 (26.6) | 46 (48.9) | 75 (79.8) | 58 (61.7) | 94 (9.2) |
| 31–40 | 49 (28.8) | 38 (22.4) | 70 (41.2) | 127 (74.7) | 73 (42.9) | 170 (16.7) |
| 41–50 | 39 (32.5) | 36 (30.0) | 63 (52.5) | 89 (74.2) | 74 (61.7) | 120 (11.8) |
| 51–60 | 69 (26.6) | 68 (26.3) | 138 (53.3) | 187 (72.2) | 156 (60.2) | 259 (25.8) |
| 61–70 | 61 (29.3) | 68 (32.7) | 111 (53.4) | 165 (79.3) | 122 (58.7) | 208 (20.5) |
| >70 | 48 (28.9) | 51 (30.7) | 86 (51.8) | 135 (81.3) | 90 (54.2) | 166 (16.3) |
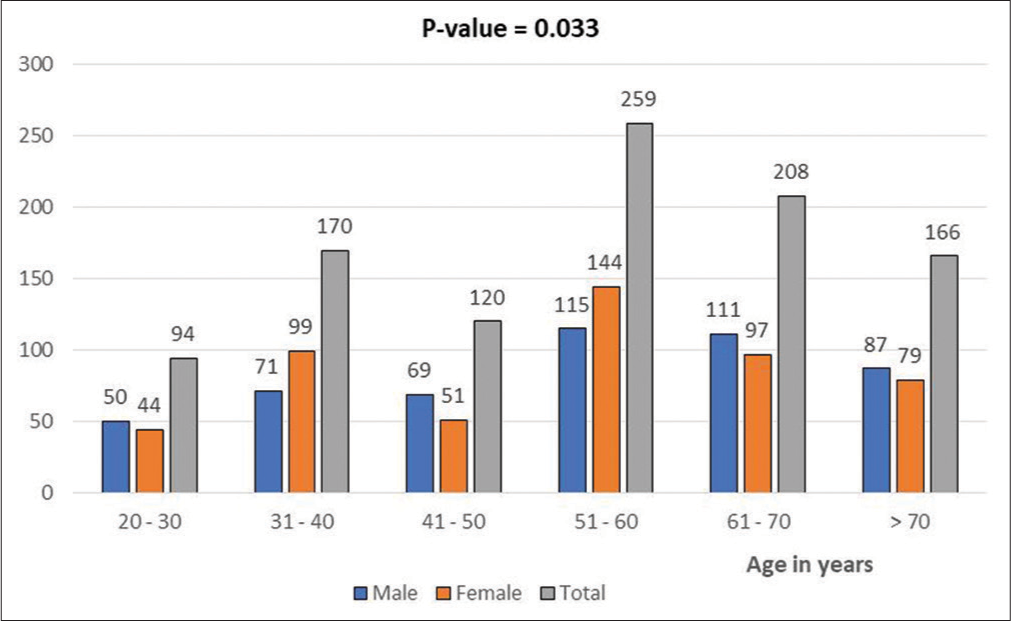
- Proportion of males and females with facet joint arthrosis stratified by age.
DISCUSSION
This study evaluated the prevalence of facet joint arthrosis in a selected Ghanaian population in relation to age, gender, and BMI. The study showed that facet joint arthrosis was significantly associated with increasing age but peaked at age 51–60. This result differs from previous studies that found an upward trend in all age groups.[3] The decreasing frequency in the number of patients with facet joint arthrosis beyond age 60 may be due to the less occupational exposure among this age group. Studies have shown that work-related activities increase the likelihood of low back pain in working-age adults.[14] An assessment of low back pain among subjects of a study conducted by Balagué et al. showed that the prevalence of low back pain increased progressively from teenage years to 60 years and then declined.[15]
This study showed that lumbar facet joint arthrosis was more common among women than in men. This is in contrast to other studies that suggest men have a greater share in the percentage of individuals presenting with facet joint arthrosis.[16] The reason for this difference may be due to the fact that cartilage is sensitive to female sex hormones, which could have an effect on the frequency of facet joint arthrosis between genders. Studies have also shown that females are more susceptible to chronic low back pain regardless of age.[17] Hormonal changes that occur during menopause, such as a decrease in estrogen levels, may result in loss of cartilage and an increased risk of developing arthritis, including lumbar facet joint arthrosis. The study by Fujiwara et al. supports the hypothesis of a gender-based disparity in the occurrence of facet joint arthrosis, showing that females are more prone to having the condition.[18] The study involved a cadaveric analysis that compared lumbar spinal motion segments between males and females with comparable clinical characteristics. The results showed that female motion segments exhibited more motion during lateral bending, flexion, and extension. Studies have also shown that increased spinal segment motion can cause excessive wear and tear[19] potentially resulting in a higher incidence of facet joint arthrosis.
Another important risk factor we considered was BMI. Previous investigations in this regard have been inconsistent, with some suggesting a positive relationship between increase in BMI[20] and others indicating a lack of such association.[21] Our study showed no statistically significant variation in BMI between male and female participants in relation to the overall prevalence of facet joint arthrosis. Majority of the patients with facet joint arthrosis were overweight. Clinically, being overweight puts extra stress on the joints, particularly in the lower back, causing cartilage in the joints to wear down more quickly, leading to degeneration and the development of arthrosis. In relation to low back pain, other works have specifically investigated the association of BMI and low back pain, and most of these are cross-sectional in design.[20] The cross-sectional studies seem to support an association between BMI and low back pain. In contrast, some works have found that the association of BMI and low back pain is diminished or absent, suggesting that some factors other than BMI are responsible for the perceived association.[20]
L4/L5 level was the most commonly affected by facet joint arthrosis in our study. Some studies have shown that facet joints at this level tend to degenerate more quickly than at any other level of the spine.[22] The possibility that L4/L5 may be the commonly affected level may be dependent on certain factors. First, the L4/L5 level is the most mobile segment of the lumbar spine, and it bears a significant amount of stress and weight from daily activities.[23] This constant movement and weight bearing can lead to wear and tear on the facet joints, making them more susceptible to degeneration. Furthermore, it is well established that L4/L5 level is one of the most common levels for lumbar herniated discs[24] and that the degenerative condition is strongly associated with facet joint arthrosis.[25] [Figure 4] showed an axial T2W MRI image at the level of L4 vertebra in one of the subjects with facet joint arthrosis.
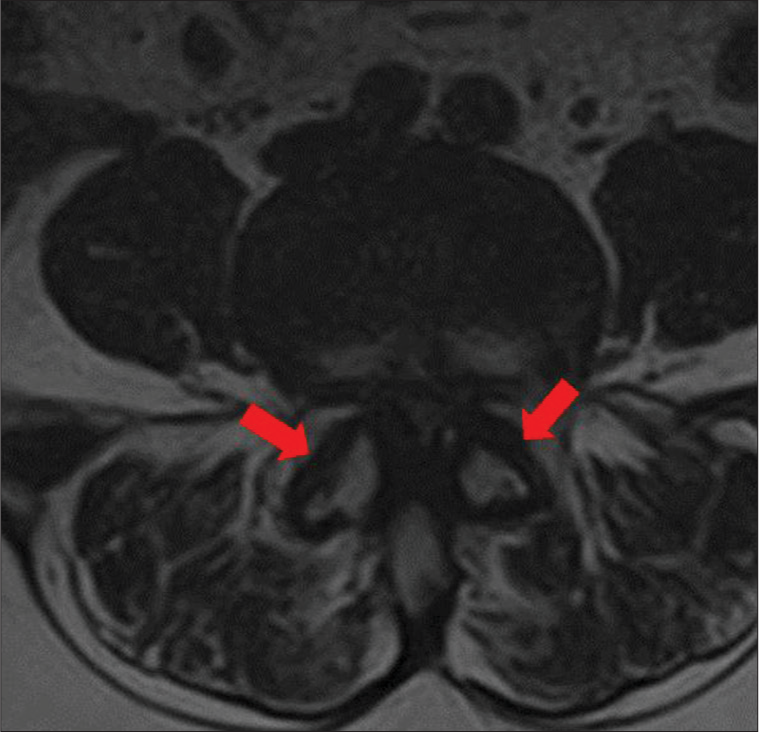
- Axial T2-weighted magnetic resonance imaging at the level of L4 vertebrae shows narrowing of bilateral facet joint spaces, marginal osteophytes, and joint hypertrophy (red arrows). There is also severe spinal canal stenosis.
Limitation
Data on occupation of the subjects were not available, and hence, we could not derive any significant association.
CONCLUSION
The prevalence of facet joint arthrosis in the Ghanaian population is significantly associated with increasing age but not with the BMI. The study also found that lumbar facet joint arthrosis was more prevalent in women than in men, which may be due to the sensitivity of cartilage to female sex hormones.
Declaration of patient consent
Patient’s consent is not required as patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Lumbar facet arthropathy In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538228 [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Prevalence of facet joint degeneration in association with intervertebral joint degeneration in a sample of organ donors. J Orthop Res. 2011;29:1267-74.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoarthritis of the spine: The facet joints. Nat Rev Rheumatol. 2013;9:216-24.
- [CrossRef] [PubMed] [Google Scholar]
- Facet joint syndrome: From diagnosis to interventional management. Insights Imaging. 2018;9:773-89.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of lumbar facet arthrosis and its relationship to age, sex, and race: An anatomic study of cadaveric specimens. Spine (Phila Pa 1976). 2007;32:2058-62.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar Facet Arthropathy Article. Available from: https://www.statpearls.com/articlelibrary/viewarticle/24455 [Last accessed on 2023 Jan 23]
- [Google Scholar]
- The provocative lumbar facet joint. Curr Rev Musculoskelet Med. 2009;2:15-24.
- [CrossRef] [PubMed] [Google Scholar]
- Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976). 2008;33:2560-5.
- [CrossRef] [PubMed] [Google Scholar]
- Characterization of degenerative human facet joints and facet joint capsular tissues. Osteoarthritis Cartilage. 2015;23:2242-51.
- [CrossRef] [PubMed] [Google Scholar]
- Differential diagnosis of facet joint disorders. Radiographics. 2021;41:543-58.
- [CrossRef] [PubMed] [Google Scholar]
- The American College of Radiology, with more than. Available from: https://www.acr.org/-/media/acr/files/practice-parameters/mr-adult-spine.pdf [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Pathria Grading System of Lumbar Facet Joint Degeneration Radiology Reference Article Radiopaedia.org. Available from: https://radiopaedia.org/articles/pathria-grading-system-of-lumbar-facet-joint-degeneration?lang=us [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Weishaupt Grading System of Lumbar Facet Joint Degeneration Radiology Reference Article Radiopaedia.org. Available from: https://radiopaedia.org/articles/weishaupt-grading-system-oflumbar-facet-joint-degeneration [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Occupational status and self-reported low back pain by gender: A nation-wide cross-sectional study among the general population in Japan. Environ Health Prev Med. 2021;26:111.
- [CrossRef] [PubMed] [Google Scholar]
- Facet Joint Arthropathy Radiology Reference Article Radiopaedia.org. Available from: https://radiopaedia.org/articles/facet-joint-arthropathy [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Prevalence of facet joint arthritis and its association with spinal pain in mountain population-A cross-sectional study. J Craniovertebr Junction Spine. 2020;11:36-45.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila Pa 1976). 2000;25:3036-44.
- [CrossRef] [PubMed] [Google Scholar]
- Materials for the spine: Anatomy, problems, and solutions. Materials (Basel). 2019;12:253.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between obesity and spinal diseases: A medical expenditure panel study analysis. Int J Environ Res Public Health. 2017;14:183.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar Spondylosis (Osteophytes, Bone Spurs): Practice Essentials, Epidemiology, Presentation. Available from: https://emedicine.medscape.com/article/249036-overview [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Lumbar degenerative disk disease In: StatPearls. Treasure Island, FL: StatPearls Publishing; Available from: https://www.ncbi.nlm.nih.gov/books/NBK448134 [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Biomechanical effect of L4-L5 intervertebral disc degeneration on the lower lumbar spine: A finite element study. Orthop Surg. 2020;12:917-30.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar disc herniation In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: http://www.ncbi.nlm.nih.gov/books/NBK560878 [Last accessed on 2023 Jan 23]
- [Google Scholar]
- Association between lumbar disc herniation and facet joint osteoarthritis. BMC Musculoskelet Disorders. 2020;21:56.
- [CrossRef] [PubMed] [Google Scholar]







