Translate this page into:
Epidemiological Risk Factors of Suicidal Behavior and Effects of the Components of Coping Strategies on Suicidal Behavior in Medical Students: A North-Indian Institution-Based Cross-Sectional Study
Sunny Garg, MD Department of Psychiatry,, Bhagat Phool Singh Government Medical College for Women Khanpur Kalan, Sonipat, Haryana 131305 India docter.sunny@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Mental stresses and adoption of poor coping strategies can be a cause of suicidal behavior in medical students.
Objective The aim of this study is to evaluate the prevalence and risk factors of suicidal behavior, and effects of the components of coping strategies on suicidal behavior among medical students
Methodology An institution-based cross-sectional study was conducted among medical students of a college located in North India for a period of 2 months from February to March 2021. A total of 531 study participants (calculated sample size) were selected, and then allocated proportionally to each academic year, both through stratified random sampling technique. Then, the participants were asked to complete a self-administered questionnaire consisting of sociodemographic characteristics, Patient Health Questionnaire-9, Suicidal Behaviors Questionnaire-Revised (SBQ-R), and coping inventory. A pretest was done to modify the coping inventory and then exploratory factor analysis was performed on it to classify the components of coping strategies. Chi-square test and multiple logistic regression analysis were used to determine the risk factors and their association with suicidal behavior.
Results A total of 104 (19.6%) respondents had reported SBQ-R cutoff score > 7 and had suicidal behavior. The rate of lifetime suicidal ideation, plan, and attempt was 20.3, 10.3, and 2.3%, respectively, among medical students, with 1-year prevalence of suicidal ideation at 33%. The mean age of the participants was 21.26 years (standard deviation = 1.99). The identified risk factors significantly associated with higher suicidal behavior were depression (odds ratio [OR] = 9.6), dissatisfaction with academic performances (OR = 4.9), and coping with mental disengagement (OR = 4.6), while coping with supportive strategies (OR = 0.57) was investigated as a preventive factor for the suicidal behavior.
Conclusion The prevalence of suicidal behavior is found to be highly alarming, revealing that depression and poor coping strategies are risk factors among medical students. The analysis recommends that quantification of the problems, treatment at an early stage, and proactive student counseling to help them embrace the appropriate coping strategies, should be the first steps in prevention of suicidal behavior.
Keywords
coping strategies
depression
factor analysis
medical students
risk factors
suicidal behavior
Introduction
Suicidal behavior is a term incorporating suicidal ideation and its consequences, including suicidal thoughts, plans, attempts, and completed suicide.1 It is a remarkable contributor to the global burden of disease, resulting from complex interconnections of bio-psycho-sociological along with environmental and cultural factors.2 3 The literature concluded that medical workforce of the future are at higher risk of suicidal behavior as compared with students of other courses and the general population.4 Suicidal behavior despite being a paramount public health crisis, is one of the unrecognized concerns in younger medical students.5 It was lamentable for the medical students that they started facing numerous mental stresses at the beginning of their course and became overburdened until their transformation into skilled physicians which enhanced the greater psychological problems.6 7 Medical students with poor mental quality or with poor coping strategies might desert their profession which might lead to suicidal behavior.8 9 10 Recent studies revealed that 1.3 to 32.7% and 1. to –53.6% of medical students experienced suicidal behavior11 and life-time suicidal ideation, respectively.12 It was found that medical students are under overwhelming mental stress, not only related to academic or professional issues, but also chronic nonacademic issues like maladaptive personality and stressful life incidents.13 Previously, it was also established that danger of suicidal behavior increased manifold in medical students with family history of mental illnesses, having had suicidal ideation,14 preexisting psychiatric disorders,15 dissatisfaction with life, decreased self-esteem, and decreased engagement in social dealings.16 17 However, there is limited data available about suicidal behavior and its risk factors in them.5 17 18 A recent study conducted in India18 found that 29.6% of the medical students had suicidal behavior while a previous study showed a higher proportion (53%).5 Given the limited amount of research conducted, more information on suicidal behavior and associated risk factors is necessary in Indian medical students as their recognition at an appropriate time can help in mitigating it and in staging prompt interventions.19
Coping strategies are dynamic processes involving cognitive and behavioral efforts that individuals use to conceptualize the thoughts, feelings, and actions encountered during various stressful conditions, with considerable inter- or intraindividual variability.20 21 There has been concordance that, appropriate coping strategies estimates favorable future outcomes, encompasses higher degree of ego development, higher self-esteem, fewer psychological problems or behavioral problems, and act as a deterrent of suicidal behavior even in the presence of stress22 23 24 while few other studies consistently demonstrated that ineffective coping skills could produce unfavorable emotions and enhance the risk of suicidal behavior during confronted stressful situations.25 26 Furthermore, studies on students suggested that maladaptive coping skills with object of maintaining well-being (such as reducing the negative emotions related to stressors and temporarily alter the focus from stressful conditions to other important things) could arrest the suicidal behavior.25 27 However, the diverse coping skills of medical students to alleviate the suicidal behavior is emphatically pronounced across the globe4 27 28 but the available research in conceptualizing and classifying the distinct coping strategies is inconsistent.27 29 To the best of our knowledge, none of the previous studies have evaluated the suicidal behavior and its risk factors, and different components of coping strategies and their effects on suicidal behavior in medical students in the same study sample, especially in Indian context. Therefore, the present study has endeavored to assess the magnitude of suicidal behavior and the risk factors affecting it, and classifying the dimensions of coping strategies and their influence on suicidal behavior in medical students in an institution located in Northern India.
Methodology
Study Design and Settings
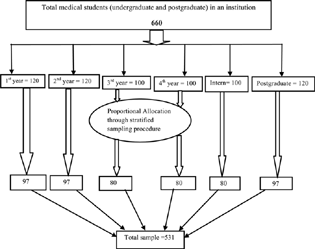
This was a descriptive cross-sectional study, performed on undergraduate and postgraduate medical students of Bhagat Phool Singh Government Medical College for Women and Hospital, an institution located in Northern part of India, conducted from February 2, 2021 to March 29, 2021. Every year, around 100 undergraduates (except first and second academic years where 120 students were enrolled) and 40 postgraduate medical students get admitted to the college. Currently, a total number of 660 medical students are studying in this institution, as shown in Fig. 1. This study was performed after getting ethical approval from the Institutional Ethical Committee Board and in accordance with Ethical Committee standards and the Helsinki Declaration. During the study, the anonymity and confidentiality of the participants were maintained as their personal information, like name or contact, was not asked.
-
Fig. 1 Graphic representation of sampling procedure of medical students.
Fig. 1 Graphic representation of sampling procedure of medical students.
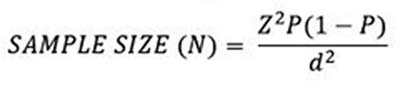
Sample Size
The study's required sample size (N = 531) was calculated by using single population proportion formula. It was calculated on the basis of following assumptions: the prevalence or expected proportion of suicidal behavior (P) is 29.6% as evaluated in previous survey,18 the absolute precision is 4% (d), 95% confidence interval (CI) (Z) where value of Z is 1.96 (constant), and nonresponse rate was also considered to be 5%.
Study Sample
Students from all batches of undergraduate and postgraduate courses, aged 18 years or older (both male and female), able to read and understand English, and willing to give informed consent, were included in the study while medical officers, house-officers, and consultants were not included in the study.
Sampling and Data Collection Procedure
A stratified random sampling method was applied to make the strata of the students of each academic year, and then the total sample size was allocated proportionately to each academic year of undergraduates (1 to 4 and internship) and postgraduates. Finally, computerized generated random number table was used to select and enlist each study participant from different academic years as shown in Fig. 1. The purpose of the study and importance of honest answers were briefed to the participants, and privacy and confidentiality of their information was also assured. Then, questionnaire sheets were distributed to the selected participants by hand in their classrooms before lectures and during breaks, and written informed consent was obtained from them before eliciting the required information. All the respondents were instructed that they could avail any help from the department of psychiatry if they required.
Data Collection Measures
The data was collected by using the self-administered questionnaires which had six sections (A to F), consisting of brief information regarding the study purposes in section A, written informed consent in section B, and about the basic information of students in section C. Section D had Patient Health Questionnaire-9 (PHQ-9) to measure the depression in students. Four questions related to Suicidal Behaviors Questionnaire-Revised (SBQ-R) scale which measured suicidal behavior, formed the section E of the questionnaire. The last part of the questionnaire (section F) had the coping inventory to analyze the coping strategies adopted by students.
Basic Information
This section of the survey had seven questions regarding basic characteristics which were collected in the form of current age, gender (male/female), residence (urban/rural), year of study, satisfaction with their academic performance (satisfied/unsatisfied/can't say), and about their tobacco smoking and alcohol consumption status (yes/no).
Patient Health Questionnaire-9 Scale
PHQ-9, a 9-item depression module, is easy to administer.30 Participants were asked, over the last 2 weeks, how often they had been bothered by the depressive symptoms. Each item is scored from 0 to 3 (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day). A total score ranges from 0 to 27. The level of depression is categorized as “0–4 = minimal,” “5–9 = mild,” “10–14 = moderate,” “15–19 = moderately severe,” and “> 20 = severe.” In context of the present study, during the analysis, two groups were created by using score < 10 for nondepressed group and > 10 for depressed group, because the cutoff score of 10 had shown good sensitivity (82%) and specificity (93%) in a structured diagnostic interview.31 The Cronbach's α of scale in the present study is 0.884, presenting good internal consistency reliability.
Suicidal Behaviors Questionnaire-Revised
SBQ-R is a very useful tool to measure the different dimensions of suicidality. It has four items that evaluate lifetime suicidal ideation/suicidal plan/suicide attempt (item-1 with 4 points), the frequency of suicidal ideation over the past 12 months (item-2 with 5 points), the threat of suicide attempt (item-3 with 3 points), and self-reported likelihood of suicidal behavior in the future (item-4 with 6 points). In the present study, item-1 question # 2 for lifetime suicidal ideation; item-1 question # 3a and 3b for suicidal plan; and item-1 question # 4a and 4b for suicidal attempt were used. A total calculated score > 7 was considered the cutoff score for the students to have suicidal behavior, had shown very good sensitivity (93%) and good specificity (95%) in a structured diagnostic interview.18 32 Responses can be used to identify at-risk individuals and specific risk behaviors. The Cronbach's α of scale in the present study is 0.801, presenting good internal consistency reliability.
The Coping Inventory
The coping mechanisms adopted by the students were assessed by using the selected 14 items of Brief Coping Orientation to Problems Experienced (Brief-COPE) scale. The instruction related to coping mechanisms in the scale was like “these items deal with ways you have been coping with the problems in your life….” These items are rated using a 4-point Likert-type scale from 1 to 4 with 1 being “I have not been doing this at all” and 4 being “I have been doing this a lot.” Then, the prefinal version of the questionnaire was tested on randomly chosen 25 medical students for the purpose of testing contextual clarity, layout, language transparency, ease of understanding the content and use, comprehensibility of the instructions, and response. None of these students faced any difficulty in either understanding or answering the questions. The Cronbach's α for this modified inventory is 0.842, with a range from 0.823 to 848, showing good internal consistency reliability while the original Brief-COPE scale Cronbach's α ranged from 0.623 to 0.926.33 Therefore, finally these 14 items representing each coping strategy were chosen for the self-administered questionnaire of the present research.
Statistical Analysis
The data was entered and analyzed using Statistical Package for Social Sciences SPSS version 25.0 (IBM, Chicago, Illinois, United States). Cronbach's α coefficient was used to assess the internal consistency of the scales. Exploratory factor analysis (EFA), using varimax rotation and principal component analysis (PCA), was performed to unmask the components of these 14 coping items and to assess the construct validity. Factor loadings value of > 0.5 was set for the variables to be a contributing variable in the factor analysis. Categorical variables were calculated as frequencies and percentages, and were compared by chi-square test (or Fisher's exact test where frequency in any cell was less than 5). Continuous variables were calculated as mean and standard deviations, and were compared by independent Student's t-test. Pearson's correlation was used to find out the correlation between suicidal behavior and designated dimensions of coping strategies. Finally, multivariable logistic regression analysis was applied to find out the independent factors by adjusting the variables significant in univariate analysis, and adjusted odds ratios (AORs) and 95% CI were used to evaluate the strength of association between independent factors and suicidal behavior. Statistically significant level was set at p < 0.05 (two-tailed).
Results
Description of Basic Characteristics of Study Participants
Five hundred and thirty-one medical students were enrolled in the present study. Out of them, a mass majority, 85% (449) of medical students were female and the remaining were male. The mean age of the participants was 21.26 years (standard deviation = 1.99), with the age ranging between 18 and 30 years. Most of the participants (60%) were within the age group of 21 to 25 years followed by age group of 18 to 20 years (35%). Around more than half of them belonged to rural areas as showed in Table 1. Table 1 also illustrates that more than two-thirds (69%) of medical students were dissatisfied with their academic performance and the rest were satisfied. Additionally, almost all the participants, 95.5 and 90%, respectively, reported that they did not smoke tobacco and consume alcohol. Around 55.2% medical students were free from any depressive symptoms. A large number, 44.8%, of medical students were moderate to severely depressed (PHQ-9 score > 10).
|
Sr. no. |
Variables |
Subgroups |
Numbers (%) |
|||
|---|---|---|---|---|---|---|
|
Total medical students (N = 531) |
Nonsuicidal group (SBQ-R score < 7) (N = 427) |
Suicidal group (SBQ-R score ≥ 7) (N = 104) |
p- Value |
|||
|
1. |
Age (in y) |
18–20 |
187 (35.2) |
146 (34.2) |
42 (40.4) |
0.601 |
|
21–25 |
318 (59.9) |
260 (60.9) |
58 (55.8) |
|||
|
More than 25 |
26 (4.9) |
21 (4.9) |
4 (3.8) |
|||
|
2. |
Gender |
Male |
82 (15.5) |
67 (15.7) |
15 (14.4) |
1.000 |
|
Female |
449 (84.5) |
360 (84.3) |
89 (85.6) |
|||
|
3. |
Residence |
Urban |
242 (45.6) |
195 (45.7) |
47 (45.2) |
1.000 |
|
Rural |
289 (54.4) |
232 (54.3) |
57 (54.8) |
|||
|
4. |
Satisfaction with academic performance |
Dissatisfied |
365 (68.7) |
265 (62.1) |
100 (96.1) |
< 0.001 a |
|
Satisfied |
156 (29.3) |
152 (35.6) |
4 (3.9) |
|||
|
Can't say |
10 (1.9) |
10(2.3) |
0 |
|||
|
5. |
Smoking status |
Yes |
24 (4.5) |
17 (3.9) |
7 (6.7) |
0.288 |
|
No |
507 (95.5) |
410 (96.1) |
97 (93.3) |
|||
|
6. |
Alcohol status |
Yes |
51 (9.6) |
39 (9.1) |
12 (11.5) |
0.459 |
|
No |
480 (90.4) |
388 (90.9) |
92 (88.5) |
|||
|
7. |
Depression |
Nondepressed group (PHQ-9 score < 10) |
293 (55.2) |
275 (64.4) |
18 (17.3) |
< 0.001 a |
|
Depressed group (PHQ-9 score ≥ 10) |
238 (44.8) |
152 (35.6) |
86 (82.7) |
|||
Abbreviations: PHQ-9, Patient Health Questionnaire-9; SBQ-R, Suicidal Behaviors Questionnaire-Revised.
Prevalence of Suicidal Behavior (Suicidal Ideation/Attempt/Plan) on SBQ-R and Its Association with Basic Variables
A small number, 104 (19.6%), of respondents had reported suicidal behavior (SBQ-R score > 7) while the remaining, 427 medical students, having SBQ-R score < 7 were included in the nonsuicidal group. The rate of lifetime suicidal ideation, plan, and attempt was 20.3, 10.3, and 2.3%, respectively, among medical students. A higher number, 179 (33.7%) participants, had suicidal ideation over the past 1 year. Around 101 students had threatened to suicide attempt more than once. A minimum number (48) of study participants, revealed self-reported likelihood of suicidal behavior in the future. Mean score on SBQ-R was 4.97 (standard deviation = 2.80) as shown in Table 2. The prevalence of suicidal behavior did not vary significantly among the basic factors, although it was found to be highest in female and in students aged 18 to 20 years. Chi-square analysis showed that a larger percentage of students in the suicidal group were significantly dissatisfied with their academic performance (96% vs. 63%). The rate of suicidal behavior also varied significantly in students who had moderate to severe depressive symptoms (83% vs. 35%). The study did not reveal any significant effect of substance consumption behavior (tobacco/alcohol) of students on their suicidal behavior (Table 1).
|
Numbers (%) |
||
|---|---|---|
|
Overall suicidal behavior |
(SBQ-R score ≥ 7) |
104 (19.6) |
|
Q1. Have you ever thought about or attempted to kill yourself? |
(Cutoff score ≥ 2) |
175 (32.9) |
|
(a) Lifetime suicidal ideation |
|
108 (20.3) |
|
(b) Suicidal plan |
|
55 (10.3) |
|
(c) Suicidal attempt |
|
12 (2.3) |
|
Q2. How often have you thought about killing yourself in past one year? |
(Cutoff score ≥ 2) |
179 (33.7) |
|
Q3. Have you ever told someone that you were going to commit suicide or that you might do it? |
(Cutoff score ≥ 2) |
101 (19) |
|
Q4. How likely is it that you will attempt suicide someday? |
(Cutoff score ≥ 3) |
48 (9) |
|
Mean (SD) |
||
|
SBQ-R scale score |
4.97 ± 2.80 |
Abbreviations: SBQ-R: Suicidal Behaviors Questionnaire-Revised; SD: standard deviation.
Factor Loadings of Coping Strategies and Their Psychometric Properties
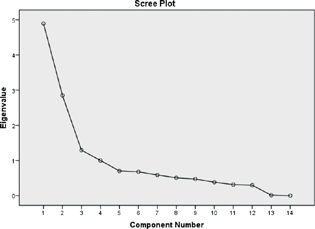
EFA on the 14 items of coping strategies yielded 4 potential latent factors explaining 71.7% of total variance, with satisfactory eigenvalue (> 1) and factor loadings (> 0.5). The Kaiser-Meyer-Olkin measure of sampling adequacy (0.856) and the Bartlett test of sphericity (chi-square = 2702.274; degrees of freedom = 91; p < 0.001) showed that the sample size for factor analysis was adequate.34 The scree plot revealed high eigenvalue for the first four components, and thereafter, the curve began to falloff gradually before the final plateau was reached (Fig. 2). The four factors/components identified from the EFA and PCA followed by varimax rotation with Kaiser normalization, assess the participant's level of coping strategies with respect to (1) psychological resilience (factor 1) comprised of five coping items (Q1, Q4, Q5, Q6, Q9) which explained 34.9% of the variance, (2) supportive strategies (factor 2) comprised of two coping items (Q2, Q3) which explained 20.3% of the variance, (3) religiosity and humor (factor 3) consisted of two coping items (Q7, Q8) which explained 9.2% of the variance, and (4) mental disengagement (factor 4) consisted of five coping items (Q10, Q11, Q12, Q13, Q14) which explained 7.2% of the variance. The internal consistency (Cronbach's α) of each factor was 0.84, 0.79, 0.83, and 0.70, respectively, which evaluated the excellent reliability as Cronbach's α was > 0.7. The reliability analysis also illustrated that all the 14 items were to be retained as shown in Table 3. For further analysis, each item of the four factors were summed up to derive continuous variables (with a range from 5 to 20 for factor 1 and factor 4, and range from 2 to 8 for factor 2 and 3) and two binary variables (with cutoffs at > 15 and > 6, respectively), corresponding to a mean value of at least a “medium amount of time” of using the corresponding coping strategies by medical students.
|
Sr. no. |
Statements |
Factor 1 |
Factor 2 |
Factor 3 |
Factor 4 |
Cronbach's α coefficient if items deleted |
|---|---|---|---|---|---|---|
|
Q1. |
I have been concentrating on my efforts/taking action to make the situation better |
0.725 |
0.829 |
|||
|
Q2. |
I have been getting emotional support/comfort from others |
0.799 |
0.824 |
|||
|
Q3. |
I have been getting help and advice from other people |
0.805 |
0.826 |
|||
|
Q4. |
I have been trying to see/looking good in what is happening |
0.696 |
0.823 |
|||
|
Q5. |
I have been thinking to come up with a strategy about what to do |
0.729 |
0.824 |
|||
|
Q6. |
I have been accepting the reality and learning to live with fact that it has happened |
0.783 |
0.826 |
|||
|
Q7. |
I have been trying to find comfort in religious or spiritual beliefs like praying or meditation |
0.596 |
0.825 |
|||
|
Q8. |
I have been making fun of the situation |
0.574 |
0.824 |
|||
|
Q9 |
I have been turning to other activities such as movies, sleeping, watching TV, reading, and shopping and it works to take my mind off the things |
0.739 |
0.825 |
|||
|
Q10. |
I have been refusing to believe that it is real |
0.567 |
0.836 |
|||
|
Q11. |
I have been using alcohol or other drugs to get rid of it and feel better |
0.571 |
0.845 |
|||
|
Q12. |
I have been giving up the attempts to deal/cope with it |
0.750 |
0.846 |
|||
|
Q13. |
I have been expressing my negative feelings and saying to let my unpleasant feelings escape |
0.687 |
0.835 |
|||
|
Q14. |
I have been blaming/criticizing myself for the things that have happened |
0.754 |
0.848 |
|||
|
Eigenvalue |
4.894 |
2.851 |
1.293 |
1.002 |
||
|
% of variance |
34.956 |
55.321 |
64.555 |
71.712 |
||
|
Cronbach's α coefficient |
0.843 |
0.799 |
0.830 |
0.704 |
Abbreviation: Brief-COPE, Brief Coping Orientation to Problems Experienced.
Note: Extraction method: principal component analysis with varimax rotation with Kaiser normalization.
-
Fig. 2 Screenplot of the coping inventory.
Fig. 2 Screenplot of the coping inventory.
Components of Coping Strategies Adopted by Medical Students and Their Correlation with Suicidal Behavior
Mean score of each component of coping strategy along with significant differences in the suicidal and nonsuicidal groups are shown in Table 4. Supportive strategies were significantly used by students in the nonsuicidal group (5.33 vs. 4.70) while mental disengagement was significantly used by students in the suicidal group (11.89 vs. 8.99). Correlational analysis between these two variables is also depicted in Table 4. Suicidal behavior among respondents was weakly negatively correlated to supportive strategies (r = –0.165, p < 0.001) which explained that more use of this component was associated with lower prevalence of suicidal behavior. In addition, suicidal behavior was moderately positively correlated to mental disengagement (r = 0.413, p < 0.001) which explained that more use of this component was associated with higher prevalence of suicidal behavior in medical students (Table 4). Psychological resilience (80%) and the religiosity and humor (61%) were more often used coping strategies in the study population as compared with supportive strategies (47%). Mental disengagement (denial, substance use, venting, behavioral disengagement, and self-blame) was a rarely used coping strategy (18%) in medical students as shown in Fig. 3.
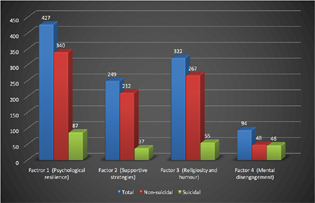
-
Fig. 3 Distribution of the components of coping mechanisms adopted by medical students.
Fig. 3 Distribution of the components of coping mechanisms adopted by medical students.
|
Sr. no. |
Coping strategies |
Total mean (SD) |
Nonsuicidal group mean (SD) |
Suicidal group mean (SD) |
p- Value |
Suicidal group (r) |
|---|---|---|---|---|---|---|
|
1. |
Factor 1 (psychological resilience) |
15.21 (3.65) |
15.28 (3.82) |
14.93 (2.84) |
0.381 |
–0.040 |
|
2 |
Factor 2 (supportive strategy) |
5.20 (1.88) |
5.33 (1.86) |
4.70 (1.90) |
0.002a |
–0.165 b |
|
3 |
Factor 3 (religiosity and humor) |
5.80 (1.58) |
5.85 (1.61) |
5.58 (1.48) |
0.109 |
–0.096 |
|
4 |
Factor 4 (mental disengagement) |
9.56 (3.36) |
8.99 (3.07) |
11.89 (3.54) |
< 0.001b |
0.413b |
Abbreviation: SD, standard deviation.
Note: r = Pearson's correlation coefficient.
Effects of Variables and Components of Coping Strategies on Suicidal Behavior
The statistically significant variables (dissatisfaction with academic performance, depression, supportive strategy, and mental disengagement) in chi-square analysis were assigned for adjusted multivariable logistic regression analysis and several factors were determined which were associated with potential risk of suicidal behavior along with protective factors. The value of R 2 (0.386) showed that the whole model explained 38.6% of variance in suicidal behavior. The most evident result was that the students who were dissatisfied with academic performance had significantly greater risk of suicidal behavior (AOR = 9.618, 95% CI = 3.351–27.600; p < 0.001) than those who were satisfied with their academic performance. The only protective factor for suicidal behavior was the use of supportive strategies (AOR = 0.577, 95% CI = 0.321–1.057; p < 0.05). The common significant variables in students were, having depression (AOR = 4.960, 95% CI = 2.760–8.915; p < 0.001) and coping with the component “mental disengagement” (AOR = 4.630, 95% CI = 2.561–8.371; p < 0.001), though the odds of developing suicidal behavior in any of these factors were around 5, as showed in Table 5.
|
Sr. no. |
Variables |
Suicidal behavior AOR (95% CI) |
|---|---|---|
|
1. |
Dissatisfaction with academic performance |
|
|
No |
1 |
|
|
Yes |
9.618 (3.351–27.600)b |
|
|
2. |
Depression |
|
|
No |
1 |
|
|
Yes |
4.960 (2.760–8.915)b |
|
|
3. |
Psychological resilience |
|
|
No |
1 |
|
|
Yes |
1.250 (0.600–2.602)0.551 |
|
|
4. |
Supportive strategies |
|
|
No |
1 |
|
|
Yes |
0.577 (0.421–1.057)a |
|
|
5. |
Religiosity and humor |
|
|
No |
1 |
|
|
Yes |
0.651 (0.358–1.183)0.159 |
|
|
6. |
Mental disengagement |
|
|
No |
1 |
|
|
Yes |
4.630 (2.561–8.371)b |
Abbreviations: AORs, adjusted odd ratios; CI, confidence interval.
Note: Model parameters for suicidal behavior: Cox and Snell R 2 = 0.243, Nagelkerke R 2 = 0.386.
Discussion
This descriptive cross-sectional study in an institution located in North India observed that one-third of medical students have suicidal ideation, and one-fifth have suicidal behavior along with few risk factors (dissatisfaction with academic performance and depression) contributing to it. However, exclusive evaluation of suicidal behavior might help in bolstering the well-being of medical students.
In the present study, the magnitude of suicidal behavior (SBQ-R > 7) among medical students was found to be 19.6%, suggesting higher rate among them as compared with general population (10.6 per 100,000 population).35 These findings are in assonance with the observations found in studies done among medical students in India,36 Ethiopia,14 and China27 where the prevalence rate was reported at 16.7, 20.6, and 21.4%, respectively. The reasons of such high prevalence of suicidal behavior could be due to the problems related to studies, families, and friends, and self-centered behavior in the medical students. In contrast to the present study, much higher prevalence of suicidal behavior on SBQ-R was estimated in studies conducted in India18 and Ethiopia,37 29.6 and 28.9%, respectively, while another study conducted in Malaysia38 revealed a much lower prevalence (7%) rate as compared with the present study.
In the present study, the magnitude of suicidal ideation over the past 1 year and lifetime suicidal ideation among medical students was found to be 33.7 and 20.3%, respectively. These findings were in line with a few cross-sectional surveys done in Pakistan,15 Ethiopia,37 and Belgium39 in context to suicidal ideation over the past 1 year, and also, with ones conducted in India18 and China40 in context to lifetime suicidal ideation. In contrast to the present study, much higher prevalence of suicidal ideation over the past 1 year was estimated (53%) in a study conducted in India by Goyal et al5 while a few studies conducted in Ethiopia41 and Oman42 revealed much lower suicidal ideation over the past 1 year than the present study. Additionally, the findings regarding lifetime suicidal ideation observed by a few cross-sectional studies done in Ethiopia (58%)37 and Oman (33%)42 were inconsistent with the prevalence rate revealed in the present study. In other words, the prevalence of suicide plan (10.3%) and attempts (2.3%) in the present study were lower compared with recent studies in India (12.5 and 5.4%)18 and Ethiopia (37.3 and 4.4%).37 Such heterogeneity in the observation could be attributed to diversities in used measurements for suicidal ideation like PHQ and Beck Suicidal Questionnaire which assesses the suicidal ideation for past 2 weeks only, and differences in economic growth, legal system, attitudes, and values.43
Suicidal behavior in the present study population was not influenced by basic characteristics (gender, place of residence, and tobacco/alcohol consumption behavior), similar to a study done by Adhikari et al44 and Torres et al.45 On contrary to present study, a few cross-sectional surveys5 14 pointed out that suicidal ideation was significantly higher in female medical students. Recently, a few authors from Ethiopia41 and Portugal46 established a significant association where alcohol consumption behavior increases more than two times odd risk of suicidal behavior among medical educators, which is incongruent to the findings observed in the present study. Among the basic characteristics variables, only dissatisfaction with academic performance was significantly associated with suicidal behavior in participants which is a finding precisely similar with observations revealed by studies done in Asian countries like Pakistan,15 China,27 and India.36 47 The present study investigated that the propensity of suicidal behavior increased 10 times in medical students who were dissatisfied with their academic performances than their counterparts which was identified as the strongest risk factor of such behavior. This result is in concordance with research showing dissatisfaction with academic performance to be a significant strong risk factor (2–3 times odd risk) for suicidal behavior.15 27 The present study evaluated that the second strongest predictor for suicidal behavior in medical students was depression. Respondents with depressive symptomatology (PHQ-9 score > 10) had 4.9 times higher odd risk of suicidal behavior than those without depression. An analytical cross-sectional study conducted in Malaysia on 657 medical students also established depression as one of the strongest predictors for suicidal behavior (5.9 times higher odd risk).38 Another institution-based cross-sectional study showed that depressed students were 10.1 times more likely to have suicidal behavior than their counterparts.14 Abdu et al observed that multivariable logistic analysis did not confirm the evidence regarding the significant association between suicidal behavior and depression in students.37 Dissatisfaction with academic performance revolves performance in academics, leading to fear of failure in exam and doubts about academic competence, due to which students might have the feelings of worthlessness, hopelessness, and uselessness, that ultimately leads to depression, which could be the possible explanation for increasing risk of suicidal behavior in these students.41 48
Coping Strategies and Suicidal Behavior
This was the first attempt in assessing the possible association between suicidal behavior and the components of coping strategies in medical students. In the present study, it was observed that psychological resilience was the most common coping strategy used by medical students followed by religiosity and humor, and supportive strategy was found to be a significant protective factor while mental disengagement a significant risk factor for suicidal behavior.
A qualitative study49 reported that a spectrum of psychological factors (passive acceptance, active coping, and positive reframing) were the potential contributing factors of psychological resilience, as evaluated in the present study. Previous researches among medical students have shown that enhancing psychological resilience could buffer the influence of negative emotions and have positive effects on psychological well-being as it is a dynamic process involving outcomes, attributes, or process of coping with, adapting to, and rebounding from adverse stressful events.50 51 Recently, few studies52 53 identified that psychological resilience was a significant protective factor against the risk of suicidal behavior, inconsistent to the findings of the present study in which no significant association was revealed between suicidal behavior and psychological resilience. Medical students accepting the problems as a challenge and solving them by distracting themselves with other activities by setting a positive path cognitively could explain the insignificant association between suicidal behavior and psychological resilience. Although having religiosity and humor affiliation was not statistically significant with suicidal behavior, in contrast to expectations, it was found that religiosity and humor as a coping strategy was used by nonsuicidal group of medical students in higher proportion. It was noted that in Brief-COPE scale, the item under “religion” also includes spirituality and under “humor” it was not clearly indicated about the use of either affiliative or self-defeating humor, which could be the possible justification for these items not to be presented as a protective factor against suicidal behavior. Eskin et al54 also found that those who were spiritual but not religious might not have experienced the protection against suicidal behavior. This nonsignificant association with suicidal behavior, similar to the present study, was only observed in a few cross-sectional studies where religiosity and humor were evaluated as a separate entity.27 54
Interestingly, the present study established a significant association between lower risk of suicidal behavior and supportive strategies. In multivariate analysis, students who used supportive strategies had more than half time (AOR = 0.57) lower odd risk of suicidal behavior than those who did not use this component of coping strategy while facing stressful situations. This finding might have suggested that medical students adopted supportive strategies in response to emotional distress, and used supportive strategies as an escape mechanism from negative emotions to alleviate the suicidal risk. Previously in the literature, it was reported that social and emotional support were the protective factors that attenuated the probability of evolution of suicidal behavior in risky cases.55 56 It was revealed that mental disengagement was the only component among coping strategies more likely to be used by suicidal group and significantly associated with the higher risk of suicidal behavior among medical students. In multivariate analysis, students who practiced mental disengagement strategies had nearly five times higher odds of developing suicidal behavior than those who did not exert this strategy. These results reflected that student with high risk of suicidal behavior could have poor problem-solving skills and negative enthusiasm against stressful situations, and symbolized the mental disengagement as a maladaptive strategy to cope with the situations. In assonance with these notions of the present study, a study in China by Tang et al25 also established that students with higher risk of suicidal behavior were found to have increased reliance on maladaptive strategies when they have insufficient resolution of acute stressful incidents and sustained exposure to stressful state of affairs. Consistent with present study findings is what is known, maladaptive strategy as a coping mechanism is ineffectual and worsens the mental well-being of students, and is also a predictor of suicidal behavior.4 27
The main strength of the present study is that this study is, to our awareness, the first to assess the predictive effects and facilitates the understanding of different components of coping strategies on risk for suicidal behavior in medical students by using EFA method. Second, the study also helped in finding the vulnerable groups of medical students by using standardized validated tools with very good internal reliability. Thus, the results observed were intriguing and had effective therapeutic implications in prevention of suicidal behavior among medical students. Lastly, lifetime suicide ideation, suicide plan, and suicide attempt were also analyzed separately in the present study.
The present study also has several limitations. First, this study was cross-sectional and such a study design did not allow the investigation of causal association of outcomes and long-term impact of stressful events on suicidal behavior. Second, this study did not include psychological issues other than depression like anxiety or stress which has been associated with suicidal behavior. This study did not include the other variables like stressful events related to their college life, dependence of substances other than tobacco and alcohol, treatment obtained, and past/family history of psychiatric illness or suicidality, which might have influenced the suicidal behavior. Third, information, selection, recall, and response bias due to the use of self-administered questionnaire cannot be ruled out in the present study. The prevalence and risk factors for suicidal behavior in each academic year were not analyzed separately, which is also one of the major limitations. Finally, the study results of coping strategies could have been impacted due to COVID-19 situation.
Conclusion and Future Suggestions
This study concluded that a high proportion of medical students presented with suicidal behavior. It provides empirical evidence that depression and dissatisfaction with academic performance in students along with the use of mental disengagement as a coping strategy were the risk factors while supportive strategy was the preventive factor for suicidal behavior. It conveys that medical colleges should make concerted efforts early on to perceive depression along with suicidal behavior among medical students and plan accordingly to strengthen their mental health by organizing counseling sessions, seminars, and workshops at an institutional level. The medical educators should provide systemic support to encourage the students which might help in facing the stressful situations during medical education. The government should aim at integration of stress coping strategies and wellness medical curricula to encounter the academic pressure which might help in production of healthy physicians.
Conflict of Interest
None declared.
Funding None.
References
- Suicidal hanging in Manipal, South India - victim profile and gender differences. J Forensic Leg Med. 2008;15(8):493-496.
- [Google Scholar]
- Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 2019;364:l94.
- [Google Scholar]
- Gender differentials and state variations in suicide deaths in India: the Global Burden of Disease Study 1990-2016. Lancet Public Health. 2018;3(10):e478-e489.
- [Google Scholar]
- Coping mechanisms as predictors of suicidal ideation among the medical students of Pakistan. J Pak Med Assoc. 2018;68(11):1608-1612.
- [Google Scholar]
- Suicidal ideation among medical students of Delhi. J Mental Health Hum Behav.. 2012;17:60-70.
- [Google Scholar]
- Medical student mental health 3.0: improving student wellness through curricular changes. Acad Med. 2014;89(4):573-577.
- [Google Scholar]
- Demographic and psychological determinants of academic achievement of medical students. J Appl Environ Biol Sci. 2017;7:1-6.
- [Google Scholar]
- Burnout and serious thoughts of dropping out of medical school: a multi-institutional study. Acad Med. 2010;85(1):94-102.
- [Google Scholar]
- Factors associated with suicidal behaviour among depressed patients in Penang, Malaysia. Arch Med Sci. 2012;8(4):697-703.
- [Google Scholar]
- Depression and stress amongst undergraduate medical students. BMC Med Educ. 2015;15:141.
- [Google Scholar]
- The prevalence of suicidal thoughts and behaviours among college students: a meta-analysis. Psychol Med. 2018;48(4):554-565.
- [Google Scholar]
- Suicidal ideation in medical students: recent insights. Adv Med Educ Pract. 2018;9:873-880.
- [Google Scholar]
- Chronic stress and suicidal thinking among medical students. Int J Environ Res Public Health. 2016;13(2):212-220.
- [Google Scholar]
- Suicide ideation, attempt, and determinants among medical students Northwest Ethiopia: an institution-based cross-sectional study. Ann Gen Psychiatry. 2020;19:44.
- [Google Scholar]
- Suicidal ideation among medical students of Pakistan: a cross-sectional study. J Forensic Leg Med. 2014;27:65-68.
- [Google Scholar]
- The association between suicide risk and self-esteem in Japanese university students with major depressive episodes of major depressive disorder. Neuropsychiatr Dis Treat. 2014;10:811-816.
- [Google Scholar]
- A study on perceived stress and coping mechanisms among students of a medical school in South India. J Evid Base Med Healthc.. 2016;3:1889-1895.
- [Google Scholar]
- Indian medical students with depression, anxiety and suicidal behavior: why do they not seek treatment? Indian J Psychol Med. 2021;43:1-7.
- [Google Scholar]
- Who attempts suicide among medical students? Acta Psychiatr Scand. 2020;141(3):254-264.
- [Google Scholar]
- Coping theory and research: past, present, and future. Psychosom Med. 1993;55(3):234-247.
- [Google Scholar]
- Listening to depression and suicide risk in medical students: the Healer Education Assessment and Referral (HEAR) Program. Acad Psychiatry. 2014;38(5):547-553.
- [Google Scholar]
- Clinical and developmental perspectives on adolescent coping. Child Psychiatry Hum Dev. 1999;30(2):87-101.
- [Google Scholar]
- Age, gender, and self-esteem differences in adolescent coping styles. J Soc Psychol. 2000;140(4):539-541.
- [Google Scholar]
- Influence of personal social network and coping skills on risk for suicidal ideation in Chinese university students. PLoS One. 2015;10(3):e0121023.
- [Google Scholar]
- The interplay of stressful life events and coping skills on risk for suicidal behavior among youth students in contemporary China: a large scale cross-sectional study. BMC Psychiatry. 2015;15:182.
- [Google Scholar]
- Predicting effects of psychological inflexibility/experiential avoidance and stress coping strategies for internet addiction, significant depression and suicidality in college students: a prospective study. Int J Environ Res Public Health. 2018;15(4):788-796.
- [Google Scholar]
- Coping strategies and suicidality: a cross-sectional study from China. Front Psychiatry. 2020;11:129.
- [Google Scholar]
- Association of stress coping strategies with suicidality in young adults: the mediation effects of depression, anxiety and hostility. Neuropsychiatr. 2017;7:974-982.
- [Google Scholar]
- Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129(2):216-269.
- [Google Scholar]
- Validity of the brief Patient Health Questionnaire mood scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28(1):71-77.
- [Google Scholar]
- The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613.
- [Google Scholar]
- The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8(4):443-454.
- [Google Scholar]
- Personality and coping. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:276-283.
- [Google Scholar]
- Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess, Res Eval. 2005;10:173-178.
- [Google Scholar]
- World Health statistics 2019: monitoring health for the SDGs, sustainable development goals. Geneva: WHO: 2019 [Last accessed on March 25, 2021]
- [Google Scholar]
- A study on suicide ideation among medical students in Mangalore. Indian J Public Health Res Dev. 2020;11:328-333.
- [Google Scholar]
- Suicidal behavior and associated factors among students in Mettu University, Southwest Ethiopia, 2019: an institution based cross-sectional study. Psychol Res Behav Manag. 2020;13:233-243.
- [Google Scholar]
- Prevalence and predictors of suicidality among medical students in a public university. Med J Malaysia. 2015;70(1):1-5.
- [Google Scholar]
- A risk algorithm for the persistence of suicidal thoughts and behavior during college. J Clin Psychiatry. 2017;78(7):e828-e836.
- [Google Scholar]
- Suicidal ideation, plans and attempts among medical college students in china: the effect of their parental characteristics. Psychiatry Res. 2017;247:139-143.
- [Google Scholar]
- Prevalence and associated factors of suicidal ideation and attempt among undergraduate medical students of Haramaya University, Ethiopia. A cross sectional study. PLoS One. 2020;15(8):e0236398.
- [Google Scholar]
- Prevalence and determinants of suicidality among medical students in Oman. Egypt J Psychiatry. 2020;41:103-110.
- [Google Scholar]
- A narrative review of suicide and suicidal behavior in medical students. Indian J Psychiatry. 2020;62(3):250-256.
- [Google Scholar]
- Prevalence of poor mental health among medical students in Nepal: a cross-sectional study. BMC Med Educ. 2017;17(1):232-238.
- [Google Scholar]
- Suicidal ideation among medical students: prevalence and predictors. J Nerv Ment Dis. 2018;206(3):160-168.
- [Google Scholar]
- Assessment of depression and suicidal behaviour among medical students in Portugal. Int J Med Educ. 2016;7:354-363.
- [Google Scholar]
- Suicide ideation among medical students: a cross-sectional study from south India. Inj Prev. 2012;18:A166. (Suppl1):
- [Google Scholar]
- Factors that distinguish college students with depressive symptoms with and without suicidal thoughts. Ann Clin Psychiatry. 2013;25(1):41-49.
- [Google Scholar]
- Factors that contribute to psychological resilience to suicidal thoughts and behaviours in people with schizophrenia diagnoses: qualitative study. BJPsych Open. 2019;5(5):e79.
- [Google Scholar]
- Psychological resilience in people experiencing schizophrenia and suicidal thoughts and behaviours. J Ment Health. 2019;28(6):597-603.
- [Google Scholar]
- Resilience and psychological distress in psychology and medical students. Acad Psychiatry. 2017;41(2):185-188.
- [Google Scholar]
- Preventing suicide, promoting resilience: is this achievable from a global perspective? Asia-Pac Psychiatry. 2019;11(4):e12371.
- [Google Scholar]
- Resilience as a focus of suicide research and prevention. Acta Psychiatr Scand. 2019;140(2):169-180.
- [Google Scholar]
- Associations of religiosity, attitudes towards suicide and religious coping with suicidal ideation and suicide attempts in 11 Muslim countries. Soc Sci Med. 2020;265:113390. (113390):
- [Google Scholar]
- The importance of coping and emotion regulation in the occurrence of suicidal behavior. Psychol Rep. 2019;122(4):1192-1210.
- [Google Scholar]
- Social support and coping styles in predicting suicide probability among Turkish students. Universal J Educ Res.. 2018;6:145-154.
- [Google Scholar]






