Translate this page into:
Spontaneous Spinal Discitis and Spondylodiscitis: Clinicotherapeutic Remarks
Address for correspondence: Dr. Alessandro Landi, Department of Neurology and Psychiatry, Division of Neurosurgery, Sapienza University of Rome, Viale del Policlinico 155, Rome 00161, Italy. E-mail: dott.alessandro.landi@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
INTRODUCTION
Spinal infections are rare (their incidence is estimated in about the 5% of all osteomyelitis) and severe pathologies. They are usually identified with different names, as disk space infection, spondylodiscitis, and vertebral osteomyelitis. Spondylodiscitis is the most frequent among spinal infections. The etiology might be due to bacteria, fungi, and parasites and might affect many anatomical structures. The reported incidence is increased in the last years.[12] The disease can be classified according to the involved anatomical structure:
-
Vertebral osteomyelitis
-
Discitis and spondylodiscitis
-
Spinal canal infections
-
Adjacent soft tissue infections.
In adult patients, the terms osteomyelitis and spondylodiscitis can be considered as more appropriate since an isolated discitis is rarely an isolated entity,[3] but in pediatric patients, it can be occasionally found.[4] The diagnosis might be challenging, often causing a delay in the identification of the pathology. On the basis of a clinical suspicion, the diagnosis can be formulated with a rational use of radiological, microbiological, and bioptic examinations.
GENERAL FEATURES
In literature, the estimated incidence varies from 4 to 24/1 million, with different criteria of inclusion (clinical and etiological).[56789101112] Spondylodiscitis accounts for 3%–5% of the total amount of osteomyelitis.[1] There are two peaks of incidence: during the childhood and in patients older than 50. Men are generally more affected than women.
The advanced sensibility of the clinicians to this problem and the growth of susceptible population has led to the increased incidence. Staphylococcus aureus is the most frequently involved agent, mostly in patients over 50 and under 20 years old, in intravenous drug users or immunosuppressed patients (both iatrogenic and host-related), patients affected by diabetes, kidney failure, hepatic cirrhosis, cancer, rheumatological diseases, with central venous catheters, or who underwent chemotherapy or previous spinal surgery [Figure 1]. In specific geographical locations, the most frequently involved agents are Mycobacterium tuberculosis and Brucella.[413141516]
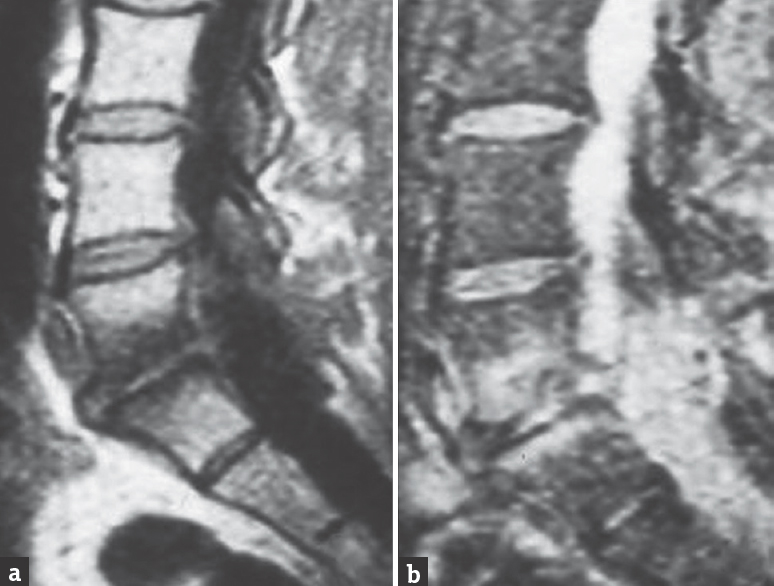
- Magnetic resonance imaging T1(a) and T2-weighted (b) images showing L4–L5 spontaneous spondylodiscitis; Staphylococcus aureus
The infectious agents can reach the final localization by hematogenous dissemination, external inoculation, and diffusion from contiguous site of infection.
Contiguous diffusion is a rare condition and might be related to upper respiratory tract infection or mediastinitis. External inoculation might be iatrogenic, related to previous spine surgery or lumbar puncture, and involving the posterior portion of the spine.[617]
Hematogenous dissemination is the most frequent cause of spondylodiscitis; the dissemination is mainly arterial, but sometimes, the diffusion can originate from the venous pelvic circulation.[31819]
The localization of the infection in the intervertebral space is frequently associated with the involvement of the adjacent vertebral bodies, and sometimes, it can be associated with spinal infections that might be located in epidural, subdural, or even intramedullary space.
The explanation for this fact is anatomical. In adulthood, the blood supply of the spine is of terminal type, and septic emboli then involve the vertebral body and the contiguous anatomical structures. In childhood, instead, there is an anastomotic circulation involving the intervertebral disk that tends to become atrophic within the age of 30.
Hematogenous dissemination affects more frequently the lumbar tract, then the cervical and the thoracic. Tuberculosis affects mainly the thoracic spine.[16]
S. aureus is the most frequently identified agent in industrialized countries, in a typically monomicrobial infection. In literature, have been described associations of S. aureus with other microbes in the setting of specific risk factors such as hematological diseases, intravenous drug users, and presence of vascular devices.
Pott's disease is the most frequent form of spondylodiscitis, accounting for 46% of cases in developing countries. In industrialized countries, instead, it is more common in immigrants coming from countries in which tuberculosis is endemic and in immunosuppressed patients. In Mediterranean area and in the Middle East, Brucella is another involved agent in spinal infections.[39202122]
DIAGNOSIS
Spondylodiscitis is not a common disease, and often, it is difficult to identify, with potential severe consequences if the diagnosis is delayed. The clinical onset has no specific signs and symptoms, with subacute or chronic presentation. Therefore, spondylodiscitis represents a diagnostical challenge, requiring both carefulness and expertise, and a thoughtful evaluation of radiological, biochemical, and microbiological examinations to formulate a correct diagnosis.[1313232425]
The main complaint of the patients is pain: it is localized in the area of the discitis and it evolves during time, often in weeks or months. In most cases, pain is the only symptom and its duration despite the use of pain medications and in the absence of a known cause should lead to the suspect of spondylodiscitis. Fever is not typical, and when occurs is only in an advanced phase of disease. Neurological involvement, with motor loss to lower and/or upper limbs, sphincter dysfunction, and sensory loss to trunk and limbs, is evidenced only in those cases of spinal cord or spinal root compression due to disruption of bone structures.[314] The routine protocol for approaching patients with clinical suspicion of spondylodiscitis includes clinical findings; laboratory findings such as erythrocyte sedimentation velocity, C-reactive protein (CRP), white blood cell, and blood cultures; and imaging findings such as plain X-ray, computed tomography (CT) scan, magnetic resonance imaging (MRI) [Figures 1 and 2], and when MRI was negative or inconclusive, radionuclide imaging findings [Figure 3]. The Oswestry Disability Index 2.0 (ODI) assessed the preoperative status and outcome. The criteria for indicating surgery are the presence of neurological deficits, spine instability, spine deformity, or pathological fractures with invasion of the canal or foramen. Patients without vertebral instability and neurological compression or without vertebral deformities were treated conservatively and underwent CT-guided biopsy, serial blood cultures, antibiogram, and specific antibiotic therapy. Patients with vertebral instability and\or spinal cord or radicular compression underwent surgery (debridement of the abscess followed by instrumented reconstruction of the vertebral integrity). The blood values of leukocytes, erythrocyte sedimentation rate (ESR), and CRP are sensible but not specific tests. The first test might not be altered in elder population while the other two tests might be altered during the onset of the disease but are not related to its severity.[2] For the identification of the microorganism responsible for the discitis, the microbiological investigation is mandatory. In all the cases with a concrete clinical suspect, blood cultures are very important. There is a higher chance to obtain a positive blood culture when the patient has fever, increasing the suspicion for endocarditis if multiple cultures are positive for the same bacterium (Gram-positive). A bioptic examination is mandatory in patients with negative blood cultures or in patients with uncertain diagnosis; it can increase the probability of an etiologic diagnosis and can be performed >1 time (both in percutaneous or in open surgical fashion) if there is persistent negativity or the clinical response to antibiotic drugs is unsatisfying.
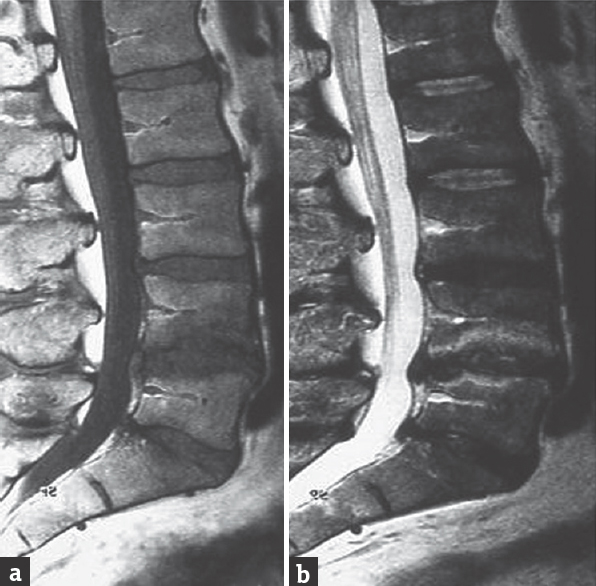
- Magnetic resonance imaging T1(a) and T2-weighted (b) images showing L4–L5 spontaneous spondylodiscitis; Escherichia coli
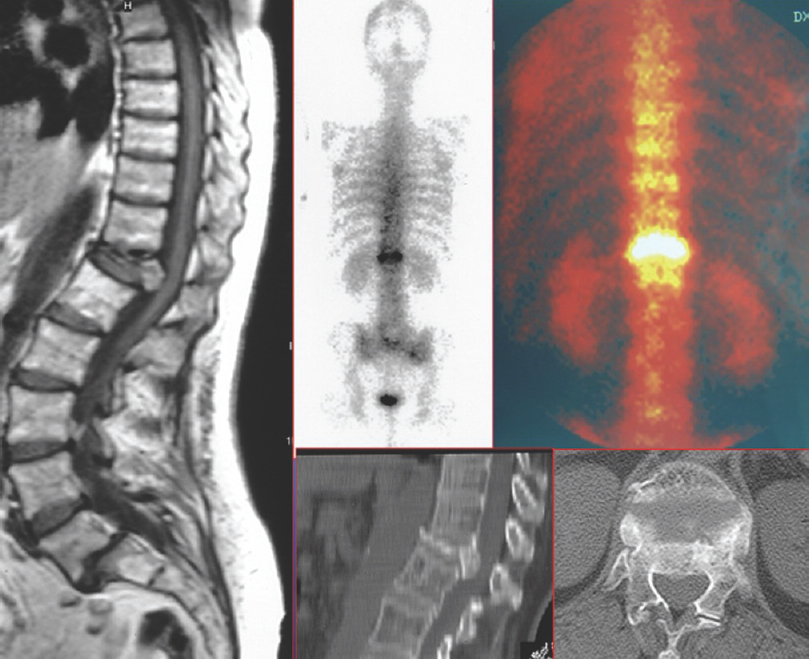
- Magnetic resonance imaging, computed tomography scans and scintigraphy with gallium 67 in an HIV immunocompromised patient. T12–L1 spontaneous spondylodiscitis; Pseudomonas aeruginosa
In immunosuppressed patients or if brucellosis is suspected, might be useful to perform also a bone marrow biopsy.
Once the biopsy has been performed, the collected material has to be sent both for microbiological and histological examination. The histological examination is useful for a correct diagnosis when the germs responsible for the discitis do not grow properly in the culture medium or in case of anaerobic bacteria. An indication about the clinical suspicion has to be sent with the collected material.
Recently, the use of bacterial DNA probes seems to be promising, even if not yet standardized. When Brucella or M. tuberculosis is involved, immunological tests are of primary importance.
Great importance has the radiological examinations. Roentgenograms do not have enough sensitivity and specificity for the diagnosis, if not in advanced stages when there is a clear deformity of the involved vertebral segment. CT scans allow a good visualization of the bony structures, allowing the detection in an early stage of bone anomalies and its possibility to serve as a guide for the bioptic examination. The diagnostic possibilities are augmented by the association of the CT scan with scintigraphy with gallium-67.[3232425]
MRI is the technique that allows a better visualization of the neural structures and of the paravertebral tissues. It is considered as the gold standard for the diagnosis of spondylodiscitis, given its high sensitivity and specificity.[23]
The examination of T1- and T2-weighted images and the use of gadolinium as contrast medium allow the differential diagnosis between spondylodiscitis and tumoral disease or degenerative conditions of the spine. Recently, in literature, has been also described the use of F-18 fluorodeoxyglucose positron emission tomography-CT (18 FDG PET-CT) for the diagnosis of spondylodiscitis. Despite the promising results in terms of sensitivity, its use is actually limited by the limited accessibility to this molecule and its high cost.[2627]
TREATMENT AND MANAGEMENT
Aims of the treatment of spondylodiscitis are pain reduction, restoration and preservation of structure and function of the spine, and eradication of the infectious process.[3] Antibiotic treatment allows to improve the prognosis so that, in recent statistics, the mortality has decreased to <5%.[28] The antibiotic treatment should be started as soon as is available the identification of the responsible bacterial agent.[29] An empirical treatment should be attempted only when sepsis or neurological impairment is present or when a spontaneous fungal spondylodiscitis is suspected, especially in immunocompromised patients.
Recently, elaborated guidelines suggest a proper duration for 6 weeks, except for infections of Brucella, Salmonella, and tuberculosis.[25] Surgery is mandatory when there is spinal instability or progressive neurological impairment, even if the patient is in treatment with antibiotics.[13253031] In general, all patients underwent antibiotic therapy for a period of at least 8 weeks and underwent a 6-month and 1-year follow-up with ESR, CRP, and MRI with gadolinium. The antibiotic therapy was based on the antibiogram germ isolated, or when it was not possible to isolate the germ, it has been set on empiric therapy. Antibiotic therapy had a variable duration, from a minimum of 8 weeks to a maximum of 48 weeks. In the light of this, the antibiotic therapy plays a fundamental role. Spontaneous discitis rarely represents an emergency, and therefore, antibiotic therapy should be initiated whenever possible after the final etiological diagnosis. When is impossible to obtain an etiologic diagnosis or in case of sepsis or of any emergency necessitating starting antibiotic promptly, this can be established empirically. Antibiotic spectrum should be extended to cover S. aureus and Escherichia coli, the two most common pathogens causing spontaneous spondylodiscitis, however, bearing in account the local epidemiological data and the possible presence of multi-resistant microorganisms, in particular, when there are predisposing risk factors (such as the use of intravenous drugs). Concerning the duration of the antibiotic therapy, the literature does not provide clear indications; in general, an initial parenteral antibiotic therapy is indicated, lasting from 4 to 8 weeks. After this period, antibiotic therapy can be continued by oral administration for a variable period based on the individual patient response and the microorganism involved. In general, a further period of oral antibiotic therapy is recommended for a period variable from 6 weeks to 3 months. Basing on our experience, recently published in the Journal of Neurosurgical Sciences,[31] antibiotic therapy is fundamental both for conservative than surgical treatment.
Spinal cord compression requires emergency surgery, aiming to decompress the spinal cord and restore neurological function. Surgical debridement must be evaluated in cases of persistent bacteremia or worsening pain. Immobilization with external bracing (i.e., Philadelphia collar or C-35 brace) is mandatory to reduce pain and promote bone healing, in the cases not requiring surgical treatment.[23] From a therapeutic point of view, the most relevant problem is not the treatment, conservative or surgical, but early diagnosis, so a careful physical, laboratory, and imaging examination is fundamental, with an important help provided by isolation of the pathogen and histology. In the light of this, early diagnosis has a fundamental role. On the basis of our clinical experience, an increase of 1 day from the onset of symptoms and the start of therapy leads to an increase in the ODI scale both at 6 months than at 1 year, with a statistical relevance.[31]
During the follow-up, the patient has to be evaluated clinically and with blood tests to assess the evolution of inflammation markers and to monitor kidney and liver function. MRI scans are not useful in this phase because it shows alterations even after the infection has been removed.[30]
Promising seems to be the use of FDG-PET CT, but its use is not widespread and has not been standardized. If the antibiotic therapy does not produce any effect, it might be useful to perform again biopsies aiming to isolate the responsible bacterium.
In the last 20 years, mortality and neurological impairment have been significantly reduced, as showed in prolonged follow-up studies.[3032] Even after healing is possible a relapse, but is not clear the incidence of the relapse.
CONCLUSION
Spondylodiscitis is a rare condition, but its sequelae can be really invalidating. Its incidence has increased in the last 20 years because of the increase of both the susceptible population and the sensitivity of the clinicians toward this condition. The technological improvement has allowed the formulation of an early diagnosis and as a consequence, a better outcome.
A detailed anamnesis, a careful clinical examination, and a series of blood tests and radiological examination of the spine are mandatory to evaluate the extension and the localization of the infection.
After the diagnostic procedures have been performed, antibiotic treatment has to be started and prolonged for at least 6 weeks. Surgical treatment is needed in those cases with spinal instability or neurological impairment.
A correct management allows to reach a complete resolution of the infection, with a good prognosis. Given its intrinsic complexity, this condition needs to be treated by both a specialist in infectious diseases and a spinal surgeon with adequate expertise.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- MR imaging findings in spinal infections: Rules or myths? Radiology. 2003;228:506-14.
- [Google Scholar]
- Admission inflammatory markers and isolation of a causative organism in patients with spontaneous spinal infection. Ann R Coll Surg Engl. 2013;95:604-8.
- [Google Scholar]
- Spinal epidural abscess: A report of 40 cases and review. Surg Neurol. 1992;38:225-31.
- [Google Scholar]
- Spinal epidural abscess: An analysis of 24 cases. Surg Neurol. 2005;63(Suppl 1):S26-9.
- [Google Scholar]
- General principles in the medical and surgical management of spinal infections: A multidisciplinary approach. Neurosurg Focus. 2004;17:E1.
- [Google Scholar]
- Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976). 2000;25:1668-79.
- [Google Scholar]
- Percutaneous transpedicular discectomy and drainage in pyogenic spondylodiscitis. Am J Orthop (Belle Mead NJ). 1998;27:188-97.
- [Google Scholar]
- Epidemiological and clinical features of pyogenic spondylodiscitis. Eur Rev Med Pharmacol Sci. 2012;16(Suppl 2):2-7.
- [Google Scholar]
- Increasing frequency of vertebral osteomyelitis following Staphylococcus aureus bacteraemia in Denmark 1980-1990. J Infect. 1997;34:113-8.
- [Google Scholar]
- A comparative study of pyogenic and tuberculous spondylodiscitis. Spine (Phila Pa 1976). 2010;35:E1096-100.
- [Google Scholar]
- Pyogenic vertebral osteomyelitis: A systematic review of clinical characteristics. Semin Arthritis Rheum. 2009;39:10-7.
- [Google Scholar]
- Osteomyelitis of the cervical spine: A potentially dramatic disease. J Spinal Disord Tech. 2002;15:110-7.
- [Google Scholar]
- Spontaneous pyogenic vertebral osteomyelitis and endocarditis: Incidence, risk factors, and outcome. Am J Med. 2005;118:1287.
- [Google Scholar]
- Spinal tuberculosis (Pott's disease): Its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev. 2001;24:8-13.
- [Google Scholar]
- Tuberculous spondylitis and pyogenic spondylitis: Comparative magnetic resonance imaging features. Spine (Phila Pa 1976). 2006;31:782-8.
- [Google Scholar]
- Spinal infection: State of the art and management algorithm. Eur Spine J. 2013;22:2787-99.
- [Google Scholar]
- The clinical use of erythrocyte sedimentation rate in pyogenic vertebral osteomyelitis. Spine (Phila Pa 1976). 1997;22:2089-93.
- [Google Scholar]
- Vertebral osteomyelitis in Göteborg, Sweden: A retrospective study of patients during 1990-95. Scand J Infect Dis. 2001;33:527-32.
- [Google Scholar]
- Surgical strategies for vertebral osteomyelitis and epidural abscess. Neurosurg Focus. 2004;17:E4.
- [Google Scholar]
- Surgical site infection in spinal surgery: Detection and management based on serial C-reactive protein measurements. J Neurosurg Spine. 2010;13:158-64.
- [Google Scholar]
- Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop. 2008;79:650-9.
- [Google Scholar]
- Expanding role of 18F-fluoro-D-deoxyglucose PET and PET/CT in spinal infections. Eur Spine J. 2010;19:540-51.
- [Google Scholar]
- Multidisciplinary management of spontaneous spinal infections: There is a correlation between timing, type of treatment and outcome? A multivariate analysis of an observational cohort study. J Neurosurg Sci 2016 Nov 23
- [Google Scholar]
- Radionuclide imaging of spinal infections. Eur J Nucl Med Mol Imaging. 2006;33:1226-37.
- [Google Scholar]





