Translate this page into:
Spontaneous Complete Absorption of a Large Prolapsed Lumbar Intervertebral Disc with Extrusion and Cranial Migration
Address for correspondence: Dr. Prasad Krishnan, National Neurosciences Centre, Peerless Hospital Campus, 2nd Floor, 360 Panchasayar, Kolkata - 700 094, West Bengal, India. E-mail: prasad.krishnan@rediffmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 35-year-old female had sudden onset low back pain followed by right lower limb radicular pain 7 months ago. She had no neurological deficits except absent right ankle jerk. Magnetic resonance imaging (MRI) showed a large L4-L5 extruded right paracentral prolapsed intervertebral disc with cranial migration [Figure 1]. Contrast imaging showed peripheral enhancement around the extruded fragment. She was advised surgery but chose to be on conservative treatment (rest and medications). Her pain gradually decreased and she had no fresh deficits. A repeat MRI done after 7 months showed spontaneous disappearance of the extruded fragment [Figure 2].
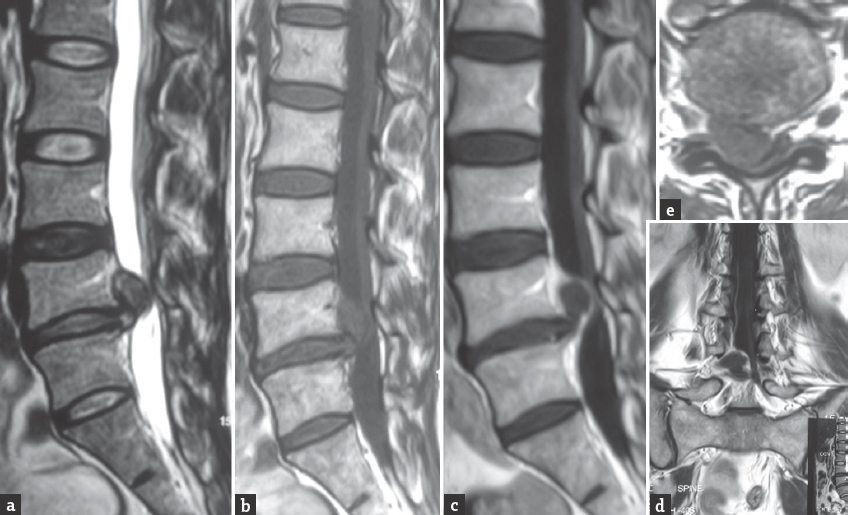
- Initial magnetic resonance imaging sequences showing a large extruded L4-L5 and cranially migrated intervertebral disc on T2 sagittal (a), T1 sagittal (b), and T1 axial (e) sections. There is contrast enhancement at the periphery suggestive of inflammation as seen on postcontrast T1 sagittal (c) and T1 coronal (d) sections
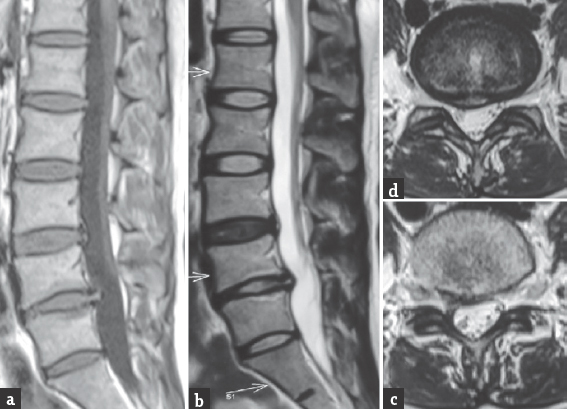
- Repeat magnetic resonance imaging sequences after 7 months showing complete absorption of the extruded fragment with restitution of the normal shape of the thecal sac on T1 sagittal (a), T2 sagittal (b), and T2 axial images (c and d). A small residual disc bulge is seen which is not causing any symptom
Low back pain with sciatica is the most common presentation of a prolapsed lumbar intervertebral disc. However, surgery is not the “final common pathway” for every patient with this problem.[1] Disc herniation can be seen without any symptom and also symptomatic discs are known to regress spontaneously.[2] Three hypotheses are commonly advanced to explain this process of spontaneous regression – retraction of the disc into the intervertebral space, shrinkage following dehydration of the extruded nucleus pulposus, and inflammatory reaction to the “foreign body” in the spinal canal resulting in its absorption.[34] Further, Komori et al.[5] have stated that extruded discs are more likely to disappear on follow-up imaging while not much change occurs in “protruded” discs and suspect that lack of vascular supply may play a role in this occurrence.
All these factors may have played a role in our patient. In fact, contrast imaging demonstrated a peripheral enhancement in the initial MRI that probably represented inflammatory granulation tissue. This case once again highlights the fact that, if situations such as impending cauda equina syndrome, intractable pain resistant to medications, and demonstrable segmental instability are excluded, a trial of conservative treatment is always warranted before taking a decision to operate since improvement might occur spontaneously as the extruded disc undergoes regression. Moreover, though in our patient the pain had disappeared, pain may persist despite the disc resorption, and hence, Reddy et al.[4] have stressed the need for fresh imaging to rule out such an occurrence, if, in future, any surgery is contemplated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Surgical vs. nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT): A randomized trial. JAMA. 2006;296:2441-50.
- [Google Scholar]
- Spontaneous regression of a large lumbar disc extrusion. J Korean Neurosurg Soc. 2010;48:285-7.
- [Google Scholar]
- Spontaneously disappearing large herniated lumbar disc fragment. J Orthop Allied Sci. 2014;2:26-8.
- [Google Scholar]
- The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976). 1996;21:225-9.
- [Google Scholar]





