Translate this page into:
Radiologically Indistinguishable Contiguous Meningioma and Schwannoma in the Same Cerebellopontine Angle in a Patient with NF2: Case Report and Literature Review
Address for correspondence: Dr. Satyashiva Munjal, Department of Neurosurgery, Paras Hospital, Sector 43, Gurgaon, Haryana, India. E-mail: satyashivamunjal@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
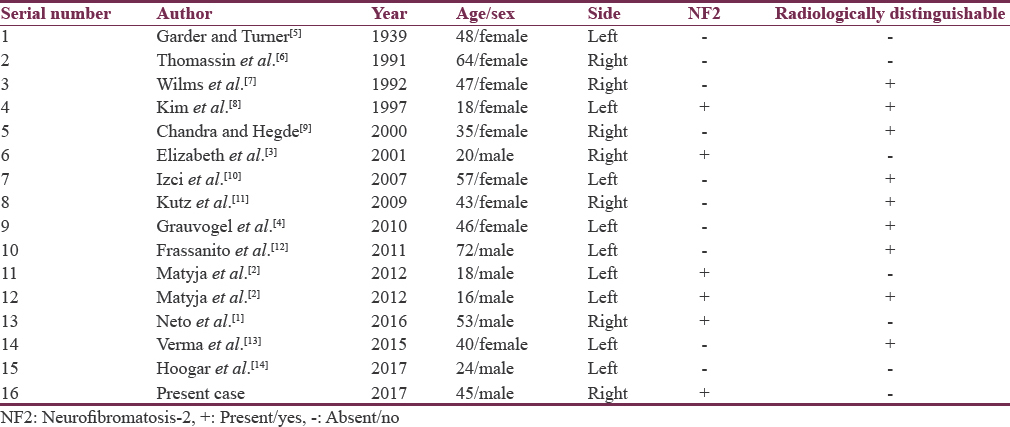
Schwannomas are the most common tumors in the cerebellopontine (CP) angle (accounting for 80%–85%), followed by meningiomas (5%–10%).[1] Simultaneous occurrence of these tumors in the same CP angle is rarely reported in literature even in patients with neurofibromatosis-2 (NF2).[23] We report a case of 45-year-old female with a contiguous acoustic schwannoma and a meningioma in the same CP angle which were radiologically indistinguishable. We also discuss the possible hypotheses leading to such a condition.
A 45-year-old female patient who was a known case of NF2, presented to us with progressively increasing difficulty in hearing from both ears (right >left) for the last 2 years. She also complained of imbalance while walking for the last 1 month. She had undergone right frontal craniotomy and Simpson Grade 1 excision of right frontal parasagittal meningioma 2 months ago when she had presented to us with difficulty in walking and climbing stairs. On examination, she had right-sided Grade 2 facial palsy and bilateral (right >left) sensorineural hearing loss. Gag reflex was impaired, and her tongue was deviated toward the right side. On tandem gait, she had tendency to fall to the right side. Magnetic resonance imaging brain [Figure 1] done revealed a 4.1 cm × 4.3 cm × 3.2 cm intensely enhancing extra-axial lesion with central necrosis in the right CP angle cistern. Another similar lesion of size 1.9 cm × 2.1 cm × 1.9 cm was seen in left CP cistern. Both lesions were hypointense on T1 weighted images and hyperintense on T2 weighted images. The cisternal and intracanalicular portions of bilateral seventh and eighth nerves were not seen separately from the lesion suggestive of bilateral acoustic schwannoma (right >left). The patient underwent right-sided retromastoid suboccipital craniotomy in the lateral position. Two lesions were identified in the right CP angle after retraction of the cerebellum. The lateral part of the tumor was firm, vascular, fibrous, suckable, attached to posterior part of petrous bone suggestive of meningioma. The anterior part of the tumor was soft to firm, moderately vascular, and extending into the internal auditory canal (IAC) suggestive of schwannoma. Neurophysiological monitoring was used to identify VII nerve. IAC was then drilled and tumor extending into canal was removed. VII-VIII cranial nerves complex identified and preserved. Postoperative period was uneventful. Histopathology revealed that the anterior part of the tumor [Figure 2a and b] was composed of sheets and interlacing fascicles of cells along with Verocay bodies suggestive of a spindle cell tumor (schwannoma). The lateral part of the tumor [Figure 3a and b] was composed of a moderately cellular tumor with sheets and whorls of spindle to oval cells and few psammoma bodies suggestive of meningioma. On immunohistochemistry, focal positivity with epithelial membrane antigen (EMA) was seen.
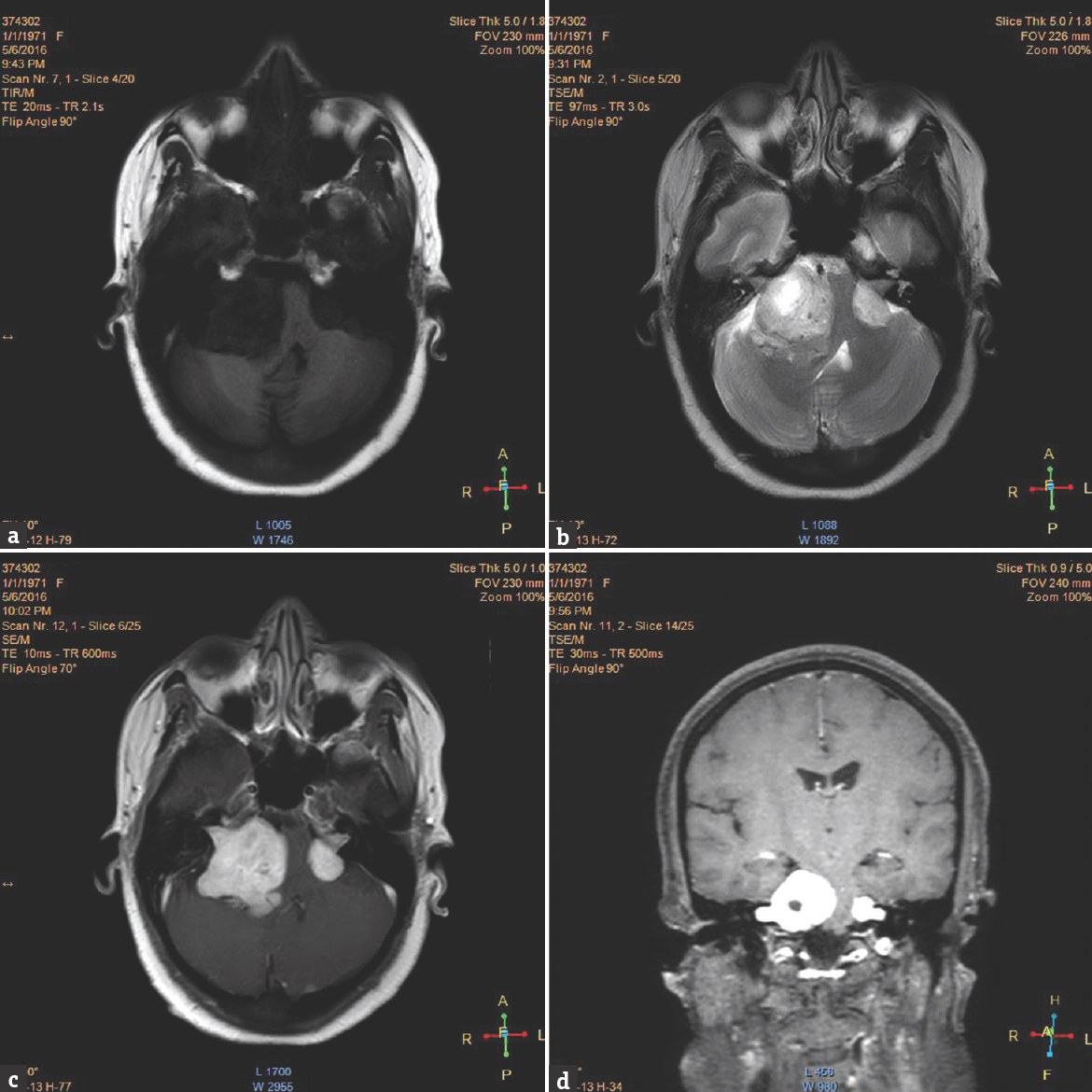
- Magnetic resonance imaging brain (a) T1-weighted image showing hypointense tumor. (b) T2-weighted image showing hyperintense tumor. (c and d) Contrast image showing homogenously enhancing tumor in bilateral cerebellopontine angle
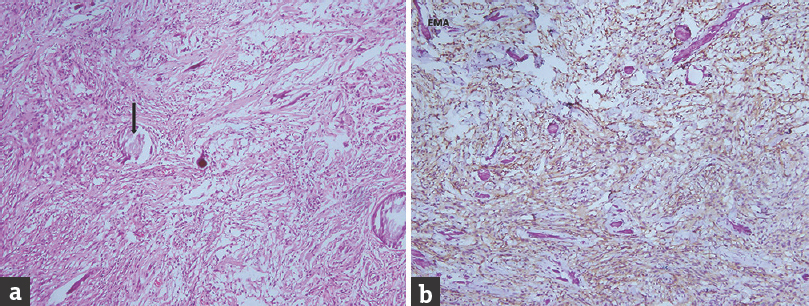
- (a) Spindle cell tumor with hypo- and hypercellular areas suggestive of schwannoma. Verocay bodies (thin arrow) are seen (H and E, ×20). (b) Tumor is negative for epithelial membrane antigen
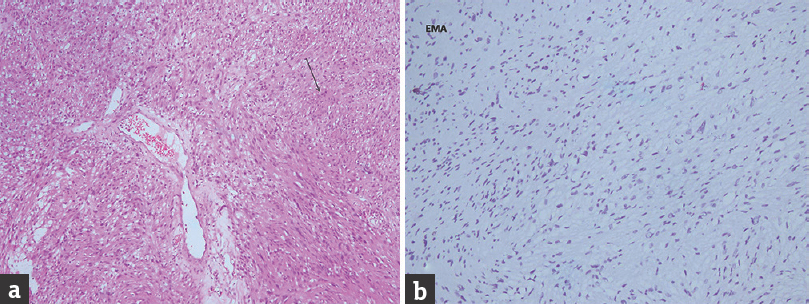
- (a) Moderately cellular tumor with oval to spindle cells arranged in sheets and whorls suggestive of a meningioma. Psammoma bodies (bold arrow) are also seen (H and E, ×20). (b) Tumor is positive to epithelial membrane antigen
Tumors of the CP angle comprise about 8% of all intracranial tumors.[4] Schwannomas form 80% to 85% while menigiomas form 5% to 10% of the CP angle tumors.[4] Simultaneous occurrence of these tumors in the same CP angle is a rare occurrence [Table 1].
NF2 is an autosomal dominant disorder affecting the central nervous system characterized by the occurrence of simultaneous bilateral acoustic schwannomas or family history of NF2 with either unilateral vestibular schwannoma or two other tumors such as glioma, schwannoma, or meningioma.[23] The disorder is caused by mutation of NF2 gene located on chromosome 22q12.2. Tumors in NF2 tend to present at an early age usually in the third decade[23] while in our case, the patient presented in the fifth decade.
The radiological differentiation of schwannoma and meningioma has been well described in literature.[411] Schwannomas are usually rounded and are centered on the IAC. They cause expansion of the canal and are associated with heterogeneous enhancement. Meningiomas on the other hand are usually broad based, have a dural tail, and are located eccentrically outside the IAC. They are associated with hyperostosis in about 70% of cases and have a uniform contrast enhancement. In our case, the tumors were not radiologically distinguishable.
Schwannomas exhibit interlacing bundles of spindle cells arranged in compact or loose arrangement referred to as Antoni A or B, respectively. There may also be areas of dense concentration of cells with palisading nuclei (Verocay bodies). They are positive for S-100 and negative for EMA while meningiomas are EMA positive and S-100 negative. Both the tumors in our case were confirmed with immunohistochemistry [Figure 2b and 3b].
Simultaneous occurrence of intracranial tumors is a rare occurrence in the absence of phakomatoses or prior irradiation. Simultaneous or contiguous tumors must be differentiated from mixed tumors which are schwannomas associated with meningeal cell proliferation reported to occur in about 21% of NF2 patients.[2312] Our patient is a case of “contiguous tumor” as the tumor was radiologically indistinguishable but histologically distinct.
The possible mechanism for such an occurrence seems debatable. The simultaneous occurrence of different tumors in the same location may occur due to metaplasia in the original tumor, collision of two different tumors, or differentiation into various cell lines from a common progenitor.[8121314] l date, however, there is no evidence of a common progenitor cell for schwannoma and meningioma. Meningothelial reaction or hyperplasia adjacent to the main tumor (schwannoma) has been proposed as a plausible mechanism for such an occurrence and may have been responsible for contiguous tumors in our case.
Simultaneous occurrence of multiple tumors in the same location is a rare occurrence. It is more likely to occur in case of phakomatoses or postirradiation. In many cases, these tumors may not be distinguishable radiologically preoperatively. Histopathology leads to diagnosis in such cases which may be confirmed with immunohistochemistry.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Collision tumour of cerebellopontine angle in a patient without neurofibromatosis criteria: Case report. J Pain Manage Med. 2016;2:112.
- [Google Scholar]
- Coexistence of meningioma and schwannoma in the same cerebellopontine angle in a patients with NF2. Folia Neuropathol. 2012;50:166-72.
- [Google Scholar]
- Mixed tumour of schwannoma and meningioma in a patient with neurofibromatosis-2: A case report. Neu India. 2001;49:398-400.
- [Google Scholar]
- A rare case of radiologically not distinguishable coexistent meningioma and vestibular schwannoma in the cerebellopontine angle – Case report and literature review. Case Rep Neurol. 2010;2:111-7.
- [Google Scholar]
- Tumors of the cerebellopontine angle. Fortuitous association of meningioma and neurinoma. Ann Otolaryngol Chir Cervicofac. 1991;108:248-52.
- [Google Scholar]
- The radiological differentiation of acoustic neurinoma and meningioma occurring together in the cerebellopontine angle. Neurosurgery. 1992;30:443-5.
- [Google Scholar]
- Mixed tumour of schwannoma and meningioma components in a patient with NF-2. Acta Neurochir (Wien). 1997;139:1061-4.
- [Google Scholar]
- A case of coexisting cerebellopontine angle meningioma and schwannoma. Neu India. 2000;48:198.
- [Google Scholar]
- Simultaneously occurring vestibular schwannoma and meningioma in the cerebellopontine angle: Case report and literature review. Clin Neuropathol. 2007;26:219-23.
- [Google Scholar]
- Concurrent vestibular schwannoma and meningioma mimicking a single cerebellopontine angle tumor. Skull Base. 2009;19:443-6.
- [Google Scholar]
- Simultaneously occurring tumours within the same cerebello-pontine angle: Refining literature definitions and proposal for classification. Acta Neurochir (Wien). 2011;153:1989-93.
- [Google Scholar]
- Rare case of radiologically distinct but pathologically admixed vestibular schwannoma and meningioma in the cerebellopontine angle: A case report. J Cancer Res Ther. 2015;11:1029.
- [Google Scholar]
- Collision tumour of cerebellopontine angle in a patient with no neurofibromatosis criteria: A rare, peculiar and interesting case. Int Surg J. 2017;4:1107-9.
- [Google Scholar]





