Translate this page into:
Accessory middle cerebral artery: An uncommon finding
Address for correspondence: Dr. Luis Rafael Moscote-Salazar, RED LATINO, Latin American Trauma and Intensive Neuro-Care Organization, Bogota, Colombia. E-mail: mineurocirujano@aol.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Circle of Willis may present with anatomical variants in up to 60% of cases, some of the associated with vascular malformations such as aneurysms.[1] The incidence of accessory middle cerebral artery (aMCA) varies from autopsy series (0.3%–2.7%) and angiographical studies (0.26%–4%).[2] Abanou et al. reported an incidence of 0.31% of aMCA in the review of 6000 angiograms.[3] Some cases may be overlooked due to the small diameter of the aMCA and the tract parallel to the MCA, resulting in superimposed images.[45] In 1961, Crompton described the duplication of the MCA (dMCA), and defined an aMCA as the “anomalous vessel arising from the horizontal portion of the anterior cerebral artery.”[6] Blackburn in 1908 described a vessel with a retrograde tract, which originated from the anterior cerebral artery (ACA) but supplying part of the MCA cortical territory.
The MCA develops after the ACA, which is considered a continuation of the primitive internal carotid artery (ICA).[4] A 52-year-old male patient who presented a clinical picture of syncope. Brain computed tomography evidence subarachnoid hemorrhage is performed. It is performed with dimensional reconstruction cerebral angiography which demonstrates the presence of anomalous artery originating in the ACA system supplying the lateral and medial striatum territory (Manelfe's Classification Type 2).
The MCA is considered a vessel favored with very little anatomical variations. (TRAN) nonetheless, the aMCA, including the dMAC and fenestrated MCA, are among the most common variations found in the intracranial vasculature, but their embryological origin is still in doubt.[7] One speculation of the origin of the aMCA between the A1 and proximal A2 segment of the ACA is that the anterior cerebral artery supply is an embryological obligation [Figure 1a and b], [Figure 2].
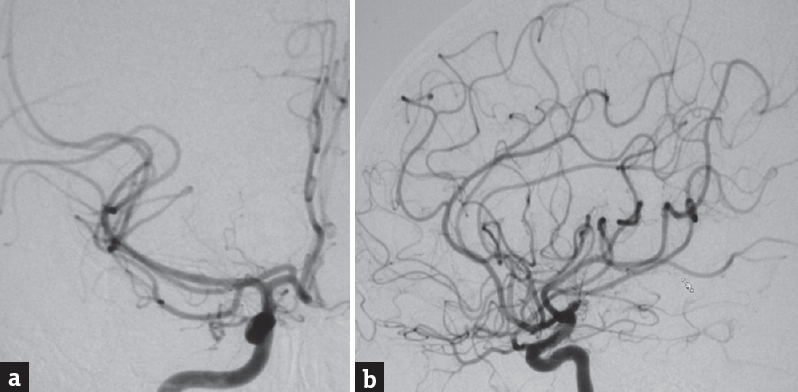
- (a and b) Computed tomography angiography showing a accessory middle cerebral artery and supplies the medial and lateral striate territories and arises from anterior cerebral artery system
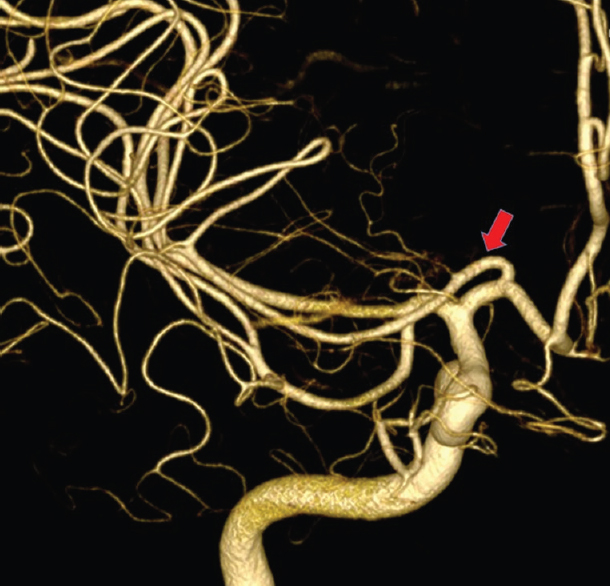
- Angiography three-dimensional showing an accessory middle cerebral
Anatomical variants may be found incidentally in magnetic resonance angiography studies.[8] In an anatomical series, of 192 cerebral hemispheres, three variants were found, corresponding to a median artery of the corpus callosum (8.3%), and aMCA (5.2%), and azigos ACA (2.1%).[1] The association of more than one anatomical variant is rarely reported, such as the case of a 45-year-old woman with a right aMCA, right bihemispheric ACA, and a median artery of the corpus callosum.[9]
In the seminal paper by Teal et al.[10] the aMCA was differentiated in two types:[5]
-
Type 1: Originated from the ipsilateral ACA near the anterior communicating artery (true aMCA)
-
Tyep 2: Originated for the distal internal carotid artery between the anterior choroidal artery and the termina bifurcation of the ICA (dMCA).
The classification by Manelfe et al.[7] is based on the site of origin of the aMCA:
-
Type-1 aMCA: proximal to the ICA bifurcation and devoided of perforating arteries
-
Type-2 aMCA: just distal to the bifurcation from the A1-ACA and with central arteries
-
Type-3 aMCA: (Heubner artery) at the junction of the ACA and anterior communicating (ACOM) artery.
The aMCA is found to course along the horizontal portion of the MCA, supplying blood flow to the orbitofrontal, prefrontal, and precentral territories. The diameter of the aMCA is usually smaller than main MCA, but the acute occlusion of the aMCA may result in severe neurological deficit, especially in the dominant hemisphere.[11] This is highlighted by Bayer-Karpinska et al.,[12] in the case report of a 21-year-old woman with a thrombus at the right distal ICA and a well-perfused MCA; thrombolysis was ineffective, and a subsequent thrombectomy revealed an aMCA originating from the A1 segment. In Takahashi et al.[13] series of 400 carotid angiograms, the aMCA was identified in 4%, and nearly all aMCA followed a constant course: origin at the ACOM artery, lateral pass through the cistern in the anterior perforated substance and supplying blood flow to the insula, lateral orbital surface, and lateral aspect of the frontal lobe.
The ICA and the ACA may provide additional vessels parallel to the MCA.[14] In some cases, the aMCA may supply collateral blood flow to the basal ganglia and frontal lobe through perforating arteries, which may protect brain tissue from ischemic injury in an acute occlusion of the MCA.[7] Such is the case reported by Liu et al.[11] in which the aMCA provided collateral blood supply to the MCA territory after a cardioembolic stroke, through leptomeningeal anastomosis, and thus avoiding a massive cerebral infarction. Many anastomoses have been reported between the MCA and the aMCA on the cortical surface, but usually, the aMCA contributes to a smaller portion of the blood flow in the MCA territory.[5]
Most of cerebral aneurisms are formed in the anterior cerebral vascular complex, which is formed by the ACA and the recurrent artery of Heubner (RAH).[9] Cerebral aneurisms are frequently found in cases with anatomical variants,[8] but aneurisms of the aMCA are rare with only 12 cases reported in the literature.[2] Some have been associated with Moyamoya disease.
The RAH was first described in 1872 by Johann Otto Leonhard Heubner as the artery originating from the ACA providing blood flow to the head of the caudate nucleus.[15] In the anatomical series, of 15 human brains from Mexican population, it was found in 93% of hemispheres; in the absence of the RHA, aMCA was found with branches irrigating the RAH tract.[1] The RAH represents phylogenetically a remnant of the anastomotic channels over the tuberculum olfactorium, between the original stem of the MCA and the ACA.[13]
The RAH is relatively constant and arises within 4 mm of the ACOM and has a recurrent course parallel to the A1-ACA.[16] The difference between RAH and aMCA is that RAH provides perforating branches to the anterior perforated substance and the aCMA only provides collateral branches to the frontal cortex.[9]
It has been proposed that the RAH and aMCA have a common origin, to the point of considering the aMCA to be a hypertrophic RAH.[15] Handa et al.[17] were the first to suggest that the aMCA is a variant of RAH. However, three differences are strongly accepted: RAH enters the anterior perforated substance while the aMCA runs laterally only providing collateral branches,[15] RAH may coexist with aMCA and perforating arteries originate from aMCA in few occasions.[5] Nonetheless, most patients with aMCA do not have RAH.[13]
For the neurosurgeon, it is essential to be familiar with the extracerebral anatomy of the RAH and aMCA in the surgical approach of ACA aneurysms, because of the temporal stapling of the ACA which may damage the RAH or aMCA.[15] During surgery or endovascular treatment, it is important to preserve the aMCA, since it may supply sufficient blood flow to the MCA territory.[18]
Even though, it is not surgically difficult to treat aneurysms of the anterior circulation, the preoperative recognition of these vascular variants is important.[4]
Understanding the collateral blood supply in cerebral ischemia and treatment of cerebral aneurysms associated with duplicated or accessory MCAs.[7]
AMCA may be important in supplying collateral blood flow to the frontal lobe and basal ganglia through the perforating arteries. Understanding the collateral blood supply in cerebral ischemia and treatment of cerebral aneurysms associated with duplicated or accessory MCAs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Variants of the anterior circle of Willis. Anatomic and angiografic correlation and its implications in the surgery of intracranial aneurysms. (Acigos anterior cerebral artery, median artery of the corpus callosum and accessory middle cerebral artery) Neurocirugia (Astur). 2004;15:578-88.
- [Google Scholar]
- Caudate haemorrhage caused by pseudoaneurysm of accessory middle cerebral artery. BMJ Case Rep. 2015;2015:Bcr2015213335.
- [Google Scholar]
- The accessory middle cerebral artery (AMCA). Diagnostic and therapeutic consequences. Anat Clin. 1984;6:305-9.
- [Google Scholar]
- Middle cerebral artery variations: Duplicated and accessory arteries. AJNR Am J Neuroradiol. 1998;19:45-9.
- [Google Scholar]
- The accessory middle cerebral artery as a collateral blood supply. AJNR Am J Neuroradiol. 1997;18:587-90.
- [Google Scholar]
- The pathology of ruptured middle-cerebral aneurysms with special reference to the differences between the sexes. Lancet. 1962;2:421-5.
- [Google Scholar]
- Incidental bilateral accessory middle cerebral arteries on MR imaging and MR angiography. Diagn Interv Radiol. 2007;13:10-2.
- [Google Scholar]
- Arteria cerebral media accesoria: Caso clínico radiológico. Acta Méd Grupo Ángeles. 2016;14:101-3.
- [Google Scholar]
- Association of three anatomical variants of the anterior cerebral circulation. Cir Cir. 2012;80:333-8.
- [Google Scholar]
- Anomalies of the middle cerebral artery: Accessory artery, duplication, and early bifurcation. Am J Roentgenol Radium Ther Nucl Med. 1973;118:567-75.
- [Google Scholar]
- Sufficient collateral blood supply from accessory middle cerebral artery in a patient with acute ischemic stroke. Interv Neuroradiol. 2015;21:215-7.
- [Google Scholar]
- Severe MCA stroke without MCA occlusion. Thrombectomy uncovers accessory middle cerebral artery? Neurology. 2015;85:831-2.
- [Google Scholar]
- Accessory middle cerebral artery: Is it a variant form of the recurrent artery of Heubner? AJNR Am J Neuroradiol. 1989;10:563-8.
- [Google Scholar]
- Accessory middle cerebral artery as a source of collateral blood flow. AJNR Am J Neuroradiol. 1991;12:1223-4.
- [Google Scholar]
- [Article in English, Spanish] Microsurgical anatomy of the extracerebral segment of recurrent artery of Heubner in the Mexican population. Cir Cir. 2011;79:201.
- [Google Scholar]
- Endovascular glue embolization of dissecting aneurysm of type-3 accessory middle cerebral artery: A contralateral approach. Interv Neuroradiol. 2015;21:664-8.
- [Google Scholar]
- The accessory middle cerebral artery: Report of further two cases. Clin Radiol. 1970;21:415-6.
- [Google Scholar]
- Endovascular treatment of a ruptured accessory middle cerebral artery aneurysm. J Clin Neurosci. 2010;17:383-4.
- [Google Scholar]





