Translate this page into:
Embolization of the Middle Meningeal Artery for the Treatment of Chronic Subdural Hematoma: A Path Less Travelled So Far
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction Chronic subdural hematoma (CSDH) is relatively common and usually encountered in elderly population. With steady increase in life expectancy, incidence of CSDH also is bound to increase proportionately. Though surgery is the treatment of choice and relatively a simpler procedure, recurrence is a cause of concern. Embolization of the middle meningeal artery (MMA) is a newly evolving treatment modality in CSDH and offers hope in some of the recently published case series.
Materials and Methods Five cases of CSDH were subjected to embolization of MMA over a period from October 2019 to July 2020. Among them, it was employed for treatment in four cases after at least two recurrences following surgery, and in one case, it was done as the patient was not fit for surgery. All procedures were done under general anesthesia and polyvinyl alcohol (PVA) particles were used for embolization. Follow-up of the patients were done with computed tomography brain at 4 weeks and after 6 months of the procedure.
Results There was no incidence of recurrence in our series. Furthermore, embolization per se did not cause any complication or side effect which could be directly attributable to the procedure itself.
Conclusion In carefully selected patients based on clinical profile and angiographic findings, MMA embolization can be an effective modality for the treatment in CSDH.
Keywords
MMA
CSDH
embolization
Introduction
Chronic subdural hematoma (CSDH) mainly affects the elderly population. With increase in life expectancy, present incidence rate of CSDH is predicted to duplicate by the end of this decade.1 2 Though surgery continues to be the most commonly employed treatment, recurrence is a major cause of concern.3 Embolization of the middle meningeal artery (MMA) is a new emerging treatment modality and offers hope in repeated recurrences and in patients not fit for surgery.4 5 6 In this article, we have tried to analyze the selection criteria and usefulness of this procedure in CSDH which was performed with minimal resources. To the best of our knowledge, this is the first such study done in a third-world country, like India, where affordability can be a potential limiting factor to employing this modality for the treatment of CSDH.
Materials and Methods
Five cases of CSDH from October 2019 to July 2020 were included in the study. Embolization was done in four cases after at least two episodes of recurrences following surgical evacuation of the hematoma and in one case because he was not fit for surgery. The details of the patients are mentioned in Table 1. All the procedures were done under general anesthesia. Exclusion criteria of the study were defined as following:
|
Age/sex |
Comorbidities |
Altered coagulation profile |
History of Trauma |
Recurrence before procedure |
Hematoma side |
Follow-up after 4 and 24 weeks |
|---|---|---|---|---|---|---|
|
78/M |
Diabetes |
No |
Yes |
3 episodes |
Bilateral |
No recurrence |
|
84/M |
PTCA, diabetes, hypertensive |
Yes |
No |
None |
Left |
No recurrence |
|
68/F |
Hypertension |
No |
Yes |
2 episodes |
Right |
No recurrence |
|
72/M |
Hypertension, Diabetes |
No |
Yes |
2 episodes |
Right |
No recurrence |
|
82/M |
Diabetes, hypertension |
No |
Yes |
3 episodes |
Right |
No recurrence |
Abbreviations: F, female; M, male; PTCA, percutaneous transluminal coronary angioplasty.
-
Patients with focal deficits.
-
Glasgow coma scale (GCS) less than 15.
-
Midline shift in computed tomography (CT) more than 1 cm.
-
No recurrence without any comorbid conditions.
-
Digital subtraction angiography(DSA) showing collateral circulation with ophthalmic artery.
-
DSA not showing any abnormal architecture of MMA.
The method of embolization was standardized. Initially a diagnostic catheter was passed through a short sheath of 5 French in the femoral artery. It is then navigated and manipulated over a guide wire into the common carotid artery. It is now used as a guiding catheter, and through it, a microcatheter (Echelon; Medtronic) is passed over a guide wire (Avigo; Medtronic). Selective angiography of the MMA is then done. If DSA findings fulfilled the exclusion criteria, microcatheter is advanced to the end branches of MMA for embolization. Material used was polyvinyl alcohol (size: 250 µm) in all cases in a mixture of heparinized saline. Immediately, following procedure, CT brain was done and patients were kept on follow-up, and CT brain was repeated 4 weeks and 6 months after the procedure (Table 1).
Results
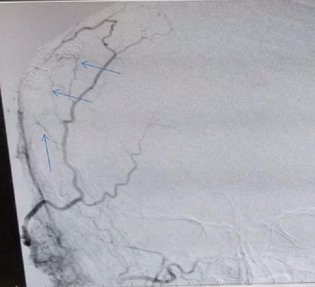
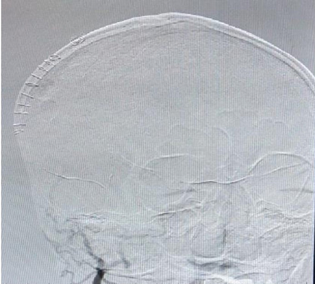
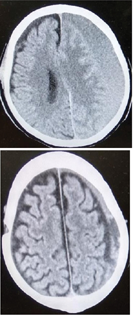
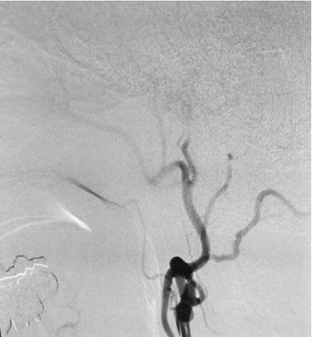
Table 1 depicts the clinical profile of all the cases. Mean age was 76.8 years. MMA embolization was done in four cases with previous history of CSDH who were treated surgically. One patient had bilateral disease. MMA embolization was offered as a primary therapy in one case due to multiple comorbidities. Four out of five cases had definite history of major or trivial trauma. Angiographically, complete occlusion of the frontal and parietal branches of the MMA was achieved in all the cases (Figs. 1-4). Contrast pooling in the subdural cavity immediately following embolization was observed in two cases (Fig. 5). No complication or side effect attributable to the procedure itself was encountered.
-
Fig. 1 Preembolization image showing branches of MMA with parent vessel. Marked arrow shows the abnormal vascular network in CSDH. CSDH, chronic subdural hematoma; MMA, middle meningeal artery.
Fig. 1 Preembolization image showing branches of MMA with parent vessel. Marked arrow shows the abnormal vascular network in CSDH. CSDH, chronic subdural hematoma; MMA, middle meningeal artery.
-
Fig. 2 Complete occlusion of the frontal and parietal branches of MMA following embolization. MMA, middle meningeal artery.
Fig. 2 Complete occlusion of the frontal and parietal branches of MMA following embolization. MMA, middle meningeal artery.
-
Fig. 3 (Top) Preembolization CT image of a case of Left sided CSDH. (Bottom) Gradual absorption of the hematoma post embolization at 1-month follow-up. CSDH, chronic subdural hematoma; CT, computed tomography.
Fig. 3 (Top) Preembolization CT image of a case of Left sided CSDH. (Bottom) Gradual absorption of the hematoma post embolization at 1-month follow-up. CSDH, chronic subdural hematoma; CT, computed tomography.
-
Fig. 4 Postembolization image showing occlusion of the MMA branches in the same patient. MMA, middle meningeal artery
Fig. 4 Postembolization image showing occlusion of the MMA branches in the same patient. MMA, middle meningeal artery

-
Fig. 5 Immediate post embolization CT brain of a patient showing pooling of the contrast material used in DSA in the hematoma cavity. CT, computed tomography.
Fig. 5 Immediate post embolization CT brain of a patient showing pooling of the contrast material used in DSA in the hematoma cavity. CT, computed tomography.
Discussion
Exact pathophysiology of CSDH is still a matter of debate. The most accepted theory is rupture of the cortical bridging veins following trivial trauma or sometimes by indirect mechanisms.7 Afterward, stripping of the outer layer of duramater leads to a series of events culminating in cell proliferation, inflammatory response, and granulation tissue formation.8 9 End result is hyper fibrinolysis within the clots and formation of microcapillaries.9 10 11 These microvessels in the outer membrane form anastomotic channels with the MMA perforators.12 13 They are very fragile and can lead to recurrent hematomas.12 14 15 Because there is a definite role of MMA in the pathology of CSDH, addressing the root cause of the formation of CSDH can be a viable solution to treat primary event, as well as to prevent repeated recurrences following surgery. Link et al while describing radiographic findings of MMA embolization of CSDH showed irregular cotton wool staining of the distal MMA vessels and contrast filling in the hematoma cavity.16 Because of these reasons, over the years, embolization in CSDH has gained ground and there are several reports of employing this modality to interrupt the blood supply of the CSDH membrane. The details of MMA embolization are being elaborated in detail by authors in a detailed review on this topic.17
However, in our opinion careful case selection is mandatory. Surgical evacuation can provide immediate relief unlike embolization. In our series, all the cases presented with only headache or milder symptoms and did not require urgent decompression. Also cost of the procedure, availability of necessary infrastructure, and trained manpower can be limiting factors more, so in a developing country like us to suggest this therapy routinely in CSDH cases.
Though embolization is relatively a safe procedure and complications are very unlikely, we should keep in mind the embolic complications. Link et al has described the presence of a petrosal branch of MMA in some cases supplying the vasa nervorum of cranial nerve VII in the petrous bone and the importance of keeping the microcatheter tip well past the petrous tip, even if this branch is not visualized to prevent complication. He also described the importance to identify and avoid the ophthalmic collaterals with the orbital/meningolacrimal branch of MMA to prevent complications.16 In author's opinion, these branches are of very small caliber and can be missed in the angiogram if the vessels are in spasm. Therefore we have done all the procedures under general anesthesia for optimum pain control and to prevent vasospasm. There is no uniformity regarding the choice of embolic material and a variety of materials have been used in different studies.17 We have taken into account the affordability of patients and hence used polyvinyl alcohol in our study. Particle size used was between 150 and 200 µm to ensure uniform and effective embolization of MMA and to prevent embolism. In our study, despite embolization being done at different time intervals for different patients, satisfactory results were seen in all the cases. In literature too, there is no consensus regarding the timing of embolization. Depending on patient variables like age, recurrence, comorbidities, and coagulation parameters, ideal timing should be decided.
Limitations
Our study is not without limitations. First of all, it is a retrospective analysis of a very small sample with inherent reporting biases to arrive at a definite conclusion about the utility of this procedure compared. Second, we have not compared the effectiveness of this study to other modalities of treatment including conservatively managed cases with mild symptoms and therefore cannot comment that it is superior to surgery. Third, longer follow-up duration is required to conclusively comment about recurrence. Data are entirely descriptive and are based on the report at a definite time period.
Conclusion
Till date, there is no randomized controlled trial reported in the literature of large sample comparing MMA embolization to surgical treatment. Initial reports mostly of very small sample size; however, they do offer hope. Being minimally invasive, requiring less hospital stay and avoiding wound complications, this procedure addresses the main etiological factor of the genesis of CSDH and hence may be effective. However careful case selection based on angiographic findings, clinical profile, and presenting symptoms of the patients are mandatory.
Conflict of Interest
None declared.
Funding None.
References
- Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J Neurosurg. 2015;123(5):1209-1215.
- [Google Scholar]
- The incidence of chronic subdural hematomas from 1990 to 2015 in a defined Finnish population. J Neurosurg. 2019;132(4):1147-1157.
- [Google Scholar]
- Postoperative course and recurrence of chronic subdural hematoma. J Korean Neurosurg Soc. 2010;48(6):518-523.
- [Google Scholar]
- Middle meningeal artery embolization treatment of nonacute subdural hematomas in the elderly: a multiinstitutional experience of 151 cases. Neurosurg Focus. 2020;49(4):E5.
- [Google Scholar]
- Middle meningeal artery embolization for chronic subdural hematoma: a series of 60 cases. Neurosurgery. 2019;85(6):801-807.
- [Google Scholar]
- Middle meningeal artery embolization for chronic subdural hematoma. Radiology. 2018;286(3):992-999.
- [Google Scholar]
- PlGF and sVEGFR-1 in chronic subdural hematoma: implications for hematoma development. J Neurosurg. 2013;118(2):353-357.
- [Google Scholar]
- Local and systemic pro-inflammatory and anti-inflammatory cytokine patterns in patients with chronic subdural hematoma: a prospective study. Inflamm Res. 2012;61(8):845-852.
- [Google Scholar]
- The “subdural” space: a new look at an outdated concept. Neurosurgery. 1993;32(1):111-120.
- [Google Scholar]
- Role of local hyperfibrinolysis in the etiology of chronic subdural hematoma. J Neurosurg. 1976;45(1):26-31.
- [Google Scholar]
- Inflammation markers and risk factors for recurrence in 35 patients with a posttraumatic chronic subdural hematoma: a prospective study. J Neurosurg. 2004;100(1):24-32.
- [Google Scholar]
- Histological study of the outer membrane of chronic subdural hematoma: possible mechanism for expansion of hematoma cavity [in Japanese] No Shinkei Geka. 1993;21(8):697-701.
- [Google Scholar]
- Histological study of vascular structure between the dura mater and the outer membrane in chronic subdural hematoma in an adult [in Japanese] No Shinkei Geka. 1999;27(5):431-436.
- [Google Scholar]
- Chronic subdural hematoma management: a systematic review and meta-analysis of 34,829 patients. Ann Surg. 2014;259(3):449-457.
- [Google Scholar]
- Recurrence of a refractory chronic subdural hematoma after middle meningeal artery embolization that required craniotomy. NMC Case Rep J. 2014;1(1):1-5.
- [Google Scholar]
- Middle meningeal artery embolization for chronic subdural hematoma: endovascular technique and radiographic findings. Interv Neuroradiol. 2018;24(4):455-462.
- [Google Scholar]
- Embolization of the middle meningeal artery in patients with chronic subdural hematoma-a systematic review and meta-analysis. Acta Neurochir (Wien). 2020;162(4):777-784.
- [Google Scholar]







