Translate this page into:
Occipital artery occlusion to facilitate transmastoid posterior fossa tumor embolization
Address for correspondence: Dr. Shakir Husain, Department of Interventional Neurology, Max Superspeciality Hospital, 1, Saket, New Delhi - 110 017, India. E-mail: drshakir@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The transmastoid branch of the occipital artery is an important supply to posterior fossa vascular malformations and tumors and is often difficult to catheterize due to tortuosity and a transforaminal course. In very difficult situations, we can try to induce spasm of the occipital artery just beyond the origin of the mastoid branch by repeated passages of the microcatheter/wire. This induces a temporary ‘ligation’ like effect so that the microcatheter can then be manipulated into the mastoid branch via the mastoid foramen. Rarely, the occipital artery has to be sacrificed if spasm cannot be induced or is short living, following which particles can be injected from a distance without entering the mastoid foramen. Occluding the occipital artery proximally has no effect on distal perfusion, as collaterals and anastomoses from superficial temporal artery, posterior auricular artery, and opposite occipital artery take over the supply.
Keywords
Artery occlusion
occipital artery
transmastoid artery
tumor embolization
Introduction
The occipital artery (OA) gives two important transforaminal branches – stylomastoid trunk and mastoid. The latter enters the cranium via the mastoid foramen to supply the dura of the posterior fossa. It also participates in anastomoses with other vessels, most important one being the vertebral artery and branches of anterior inferior cerebellar artery. The transmastoid artery is an important feeder to posterior fossa vascular malformations and tumors and can be the only prominent supply occasionally. Superselective microcatheterization of this artery, however, can be difficult due to extreme tortuosity and the difficulty in navigating through the narrow mastoid foramen.
Case Report
A 45-year-old woman presented with headache since 2 years and gradually deteriorating vision since 3 months. She had bilateral papilledema (left more than right) with decreased visual acuity; however, other neurological examinations were normal. A magnetic resonance imaging (MRI) scan showed a large left petrous-based meningioma, bright on T2W images and enhancing brilliantly on post-gadolinium scans. Considering these to be indicative of hypervascular nature of the tumor, a preoperative embolization was undertaken.
During the procedure, the tumor was found to be hypervascular and with a single feeding artery, that being the transmastoid branch of the left OA [Figure 1a]. However, this artery proved difficult to catheterize due to its tortuosity, small size, and a recurrent course of the ostial and proximal portions. Various microcatheters (including semi and true flow-guided catheters) and microguidewire systems were used without benefit. An attempt was then made to induce spasm in the parent artery distal to the feeding vessel origin by repeated passages and torquing the wire. However, this also turned futile as the spasm inductions lasted short [Figure 1b].
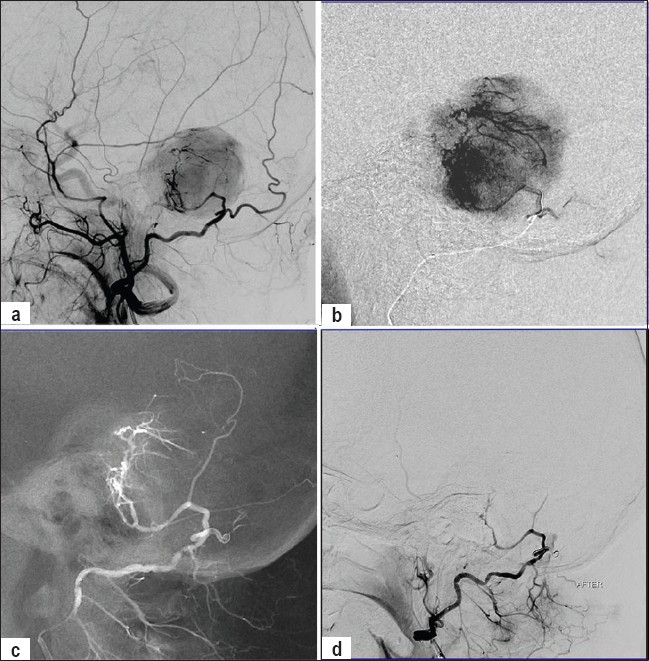
- (a) Left external carotid artery injection showing the hypervascular posterior fossa tumor fed primarily by the transmastoid foraminal branch of occipital artery. (b) Microcatheter injection of the left occipital artery near the mastoid branch showing spasm of the occipital artery with no forward flow. (c) Post coil-occlusion of the occipital artery; the contrast flow is entirely via the artery of interest now. (d) Post embolization left external carotid artery injection showing no tumor stain.
We then decided to sacrifice the parent artery and used a Guglielmi Detachable coil (GDC) for the same. The artery was sacrificed just distal to the origin of the mastoid branch [Figure 1c].
After occlusion, embolization was done with polyvinyl alcohol (PVA) particles, injections being made from the OA trunk but still outside the cranium. Care was taken to inject slowly, allowing the pulsations carry forward the contrast-mixed particles, and not allow any reflux. Post procedure angiogram showed near complete occlusion of the tumor bed [Figure 1d]. The patient was operated on after 2 days, with complete excision of the tumor and minimal blood loss. The tumor turned was an angioblastic variety of meningioma. The patient had an uneventful recovery and is presently asymptomatic.
Discussion
The transmastoid artery (1-3 in number) is a major and important branch of the OA (with the stylomastoid branch) passing through the mastoid emissary foramen and supplying the dura of the posterior fossa.[1–3] It is a prominent supply to vascular malformations and tumors of the posterior fossa. It enters the mastoid foramen soon after origin and may have a recurrent proximal course. The mastoid foramen is often small and often does not allow the passage of microcatheter of the available sizes. The narrow-caliber (mean diameter 0.6 mm) and the tortuosity of the artery does not make things any easier.
The OA provides arterial supply to most of the muscles of the posterior and lateral upper portion of the neck, occipital muscles, posterior half of the scalp, and multiple neuronal branches to facial, spinal accessory, hypoglossal, occipital nerve of Arnold and greater occipital nerve. Its terminal branches form an anastomotic rete with branches of the contralateral OA, posterior auricular artery, and superficial temporal artery.[1–3] Hence, knocking off the main trunk does not have any major side effects.[34] In fact, for the same reason, it is a favored artery for bypass surgeries and can be ligated/occluded during surgeries or for treating aneurysms/pseudoaneurysms.[34]
However, unwanted embolization into the distal vascular bed can lead to scalp necrosis and neuronal ischemia, and hence we must prevent the same.
In our case, we occluded the arterial trunk just after the mastoid branch had originated, so as to enable injection of PVA particles without entering the mastoid foramen.
Another important point to be remembered is the common occurrence of occipital to vertebral artery anastomosis.[1] Any inadvertent embolization can be devastating. Hence, mixing of contrast agent with the PVA is compulsory and so is a slow injection, with the surgeon and assistants on an active lookout for any reflux.
Summary
Here we describe a case of petrous meningioma with a single feeder from the mastoid branch of the OA, which could not be superselectively catheterized; hence, the occipital trunk was sacrificed and PVA particles injected without entering the cranial cavity.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- The occipital artery: Anatomy- normal angiographic aspects – embryological significance. Neuroradiology. 1978;15:31-7.
- [Google Scholar]
- The occipital artery: A microanatomical study. Neurosurgery. 2006;58(Suppl 1):ONS114-22.
- [Google Scholar]
- Microsurgical anatomy of cerebral revascularization. Part II: Posterior circulation. J Neurosurg. 2005;102:132-47.
- [Google Scholar]
- Endovascular treatment of traumatic aneurysm of the occipital artery. Cardiovasc Intervent Radiol. 2006;29:486-7.
- [Google Scholar]






