Translate this page into:
Stroke due to Percheron Artery Occlusion: Description of a Consecutive Case Series from Southern Portugal
Hipólito Nzwalo, MD, MSc, PhD Department of Biomedical Sciences and Medicine, University of the Algarve Estr. da Penha, 8005-139 Faro Portugal nzwalo@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
The artery of Percheron (AOP) is an abnormal variant of the arterial supply of the thalamus. Stroke caused by AOP occlusion is seldom reported. AOP leads to bilateral thalamic and rostral midbrain infarct presenting with unspecific manifestations. There are few descriptions of case series of stroke caused by AOP. We sought to review the clinicoradiological characteristics of AOP infarction from Algarve, Southern Portugal. Eight consecutive cases were retrospectively identified by searching the electronic clinical charts, as well as the stroke Unit database (2015–2020). Sociodemographic (age and gender) and clinicoradiological characteristics (etiological classification, admission severity, manifestations, and short- and long-term prognoses) were retrieved. The corresponding frequency of AOP infarction was 0.17% (95% confidence interval: 0.05–0.28). The mean age was 67.1 (range: 60–80) years. The range of stroke severity evaluated assessed by the National Institute of Health Stroke Scale ranged from 5 to 23 (median = 7.5). None of the patients receive acute ischemic stroke reperfusion treatment. AOP patterns were isolated bilateral paramedian thalamic (n = 2), bilateral paramedian and anterior thalamic (n = 2), and bilateral paramedian thalamic with rostral midbrain (n = 4). Two patients (20%) died on the short term (30 days). At hospital discharge, six patients had functional disability of ≤2 on the modified Rankin scale. In the follow-up at 6 months, half (n = 3) of the survivors had persistent hypersomnia and two had vascular dementia. Stroke from AOP presents with variable clinical and radiological presentations and patients do not receive alteplase. The short-term survivor and the long-term functional independency can be compromised after AOS infarct.
Keywords
bithalamic infarct
the artery of Percheron
ischemic stroke
paramedian thalamic infarct
Introduction
The artery of Percheron (AOP) is an uncommon variant of the thalamoperforating arteries characterized by a single dominant perforating artery originating in the proximal segment of the posterior cerebral artery (PCA) and supplying bilateral paramedian thalamus and rostral midbrain.1 Because of the thalamus complex functional anatomy, occlusion of the AOP causes variable and unspecific clinical manifestations.2 Most of knowledge about the characteristics and outcomes of stroke secondary to AOP comes from single case reports poses problems of publication bias. In addition, the number of consecutive case series of stroke as a result of AOP infarction in literature is sparse, reflecting the rarity of the syndrome and complicating appropriate prognostication in routine practice. Therefore, we sought to review the clinicoradiological characteristics of AOP infarction from stroke patients consecutively admitted to a single community representative center from Algarve, the southernmost region of Portugal.
Methods
Among the 4,705 consecutive acute ischemic stroke (AIS) cases (January 2015–November 2020), eight cases were retrospectively identified by searching the electronic clinical charts, as well as the Stroke Unit database from January 2015 to November 2020. Patients with documented first ever bilateral simultaneous ischemic lesions affecting the medial thalamus on brain magnetic resonance imaging (MRI) or cranial tomography were included. The individual electronic charts were reviewed to extract the sociodemographic (age and gender) and clinicoradiological (etiological classification, admission severity and manifestations, and short-term and long-term prognoses) characteristics. The Trial of Org 10172 in Acute Stroke Treatment (TOAST) was used for etiological classification.3 Radiological patterns of AOP infarction were classified as follows: bilateral paramedian thalamic with midbrain, bilateral paramedian thalamic without midbrain, bilateral paramedian thalamic with anterior thalamus and midbrain, and bilateral paramedian thalamic with anterior thalamus without midbrain.1 This study was approved by institutional ethics committee. Informed consent was waved due to its retrospective nature.
Results
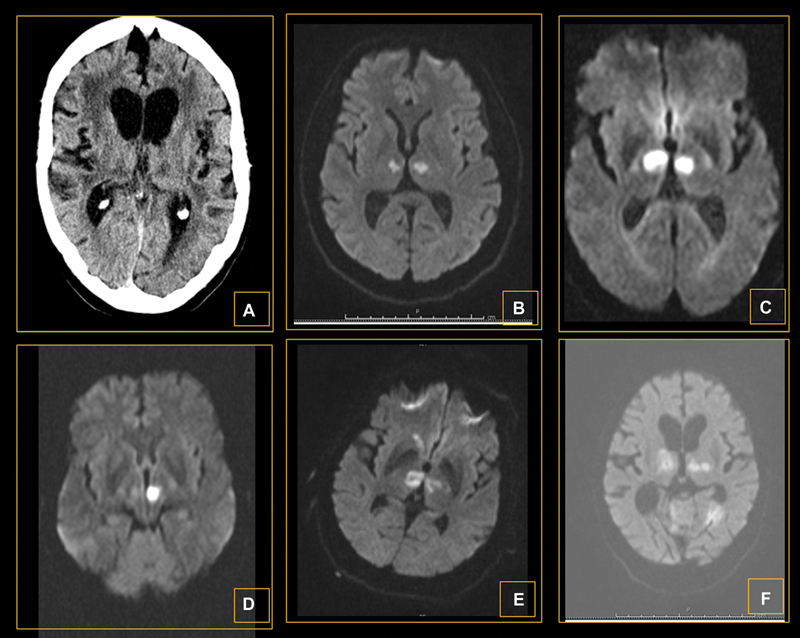
All eight cases were confirmed with magnetic resonance. The corresponding frequency of AOP infarction was 0.17% (95% confidence interval: 0.05–0.28). Table 1 resumes the sociodemographic and clinicoradiological characteristics. The mean age was 67.1 (range: 60–80) years and gender ratio was 1:1. Patients presented with varying levels of mental status disturbance, cognitive manifestations, and oculomotor nerve palsies. The range of stroke severity evaluated assessed by the National Institute of Health Stroke Scale (NIHSS) ranged from 5 to 23 (median = 7.5). None of the patients receive AIS reperfusion treatment. Three of the four stroke patterns associated with AOP occurred: isolated bilateral paramedian thalamic (n = 2), bilateral paramedian and anterior thalamic (n = 2), and bilateral paramedian thalamic with rostral midbrain (n = 4). Representative cases are illustrated in Fig. 1. Two patients (20%) died on short term (30 days). At hospital discharge, six patients had functional disability of ≤2 on the modified Rankin scale (mRS). In the follow-up, at 6 months, half (n = 3) of the survivors had persistent hypersomnia and two had vascular dementia.
-
Fig. 1 Representative radiologic appearance of the artery of Percheron infarction, bilateral paramedian lesions (A) hypodense on brain cranial tomography and (B) restriction on magnetic resonance (MR) diffusion-weighted imaging (DWI); combined bilateral thalamic lesion (C) with rostral mesencephalic on DWI MR ; combined anterior (D) with paramedian bilateral lesions on DWI MR.
Fig. 1 Representative radiologic appearance of the artery of Percheron infarction, bilateral paramedian lesions (A) hypodense on brain cranial tomography and (B) restriction on magnetic resonance (MR) diffusion-weighted imaging (DWI); combined bilateral thalamic lesion (C) with rostral mesencephalic on DWI MR ; combined anterior (D) with paramedian bilateral lesions on DWI MR.
|
Case |
Age (y) |
Gender |
Clinical manifestations |
Admission NIHSS |
Etiologic (TOAST) |
Radiological pattern |
Discharge functional status (mRS≤2) |
Long-term functional status |
|---|---|---|---|---|---|---|---|---|
|
1 |
61 |
F |
MSD |
3 |
Cardioembolic |
B |
Yes |
Hypersomnia |
|
2 |
66 |
F |
BAI |
4 |
Cardioembolic |
A |
Yes |
mRS ≤ 2 |
|
3 |
78 |
F |
OMD |
5 |
Cardioembolic |
C |
Yes |
mRS ≤ 2 |
|
4 |
60 |
M |
BAI, OMD |
16 |
Undetermined |
A |
Yes |
Hypersomnia, vascular dementia |
|
5 |
68 |
M |
MSD, BAI, OMD |
23 |
Undetermined |
C |
No (deceased) |
Not applicable |
|
6 |
80 |
F |
MSD, BAI |
24 |
Large-artery atherosclerosis |
B |
No (deceased) |
Not applicable |
|
7 |
53 |
M |
BAI, MSD |
3 |
Undetermined |
B |
Yes |
Hypersomnia, vascular dementia |
|
8 |
71 |
M |
OMD |
5 |
Undetermined |
B |
Yes |
mRS ≤ 2 |
Abbreviations: BAI, behavioral/amnesic impairment; F, female; M, male; mRS, the modified Rankin score; MSD, mental status disturbance; NIHSS, National Institute of Health Stroke Scale; OMD, ocular movement disorders; TOAST: Trial of Org 10172 in acute stroke treatment.
Discussion
The frequency of AOP in our study (0.17%) are consistent with findings from the few available representative case series of AOP infarcts which have shown a frequency of 0.1 to 0.6%.2 4 5 6 7 In the absence of the classic signs of stroke, the presentation with behavior manifestations, somnolence may suggest alternative diagnosis such as inflammation, infection, metabolic, infiltrative tumor, or deep cerebral vein thrombosis. In fact, patients with AOS infarcts rarely receive thrombolysis because of delayed AIS recognition.7 8 9 None of our patients received acute reperfusion for AIS because the diagnosis was not promptly considered by the relatives or by the emergency physicians. With significant variation and overlap, the thalamus has four vascular territories: anterior, paramedian, inferolateral, and posterior. The paramedian or thalamoperforating arteries, which arise from the proximal segment of the PCA,1 supply the paramedian thalamus. The lesion patterns of AOP reflect the known variations of territorial contribution of the paramedian arteries.1 Indeed, in our case series, the bilateral paramedian thalamic with anterior thalamus and midbrain involvement subtype, which is associated with the most dominant paramedian artery variant, did not occur.4 As shown in our case series, both short-term survivor and the long-term functional independency can be compromised after AOS infarct. Thus, highly clinical and radiological suspicion is important to improve the chances of prompt treatment and favorable outcomes.10 There are important limitations worthwhile pointing out. The study was retrospective and the sample size small as in the available studies. The possibility of missing more dramatic cases with very rapid unfavorable outcomes or minor cases, with very mild symptoms cannot be ruled out. However, AOS infarct is rare and our incidence rate was within the figures from the literature. The largest case series presented so far included 37 patients from two different hospitals.1 On the other hand, given the fact of our Stoke Unit being the sole one serving the region,11 we do believe that study findings are representative of that from the community.
Conclusion
In conclusion, our case series confirms that stroke due to AOP is a rare event, with clinical and radiological variability, including an initial severity. The evolution to death is a possibility in the acute phase which is explained by lesion of strategic structures involved in maintaining wakefulness. Regardless of motor autonomy at discharge, long-term functional impairments, namely, persistent hypersomnia and dementia, do occur in a high proportion of survivors.
Conflict of Interest
None declared.
Funding None.
References
- Artery of percheron infarction: imaging patterns and clinical spectrum. AJNR Am J Neuroradiol. 2010;31(7):1283-1289.
- [Google Scholar]
- Anteromedian, central, and posterolateral infarcts of the thalamus: three variant types. Stroke. 2004;35(12):2826-2831.
- [Google Scholar]
- Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24(1):35-41.
- [Google Scholar]
- Bilateral thalamic infarction. Clinical, etiological and MRI correlates. Acta Neurol Scand. 2001;103(1):35-42.
- [Google Scholar]
- Bilateral paramedian thalamic artery infarcts: report of 10 cases. J Stroke Cerebrovasc Dis. 2010;19(4):283-289.
- [Google Scholar]
- Bilateral infarction of paramedian thalami: a report of two cases of artery of Percheron occlusion and review of the literature. BMJ Case Rep. 2011;2011:2-8.
- [Google Scholar]
- Assessment of Percheron infarction in images and clinical findings. J Neurol Sci. 2017;383:87-92.
- [Google Scholar]
- Irreversible hypersomnolence after bilateral thalamic infarction. J Neurosci Rural Pract. 2018;9(1):167-168.
- [Google Scholar]
- Artery of percheron infarct: 12 cases and their complex clinical courses. Neurohospitalist. 2018;8(3):141-145.
- [Google Scholar]
- Clinical-radiographic correlates of Artery of Percheron infarcts in a case series of 6 patients. J Clin Neurosci. 2019;61:266-268.
- [Google Scholar]
- Incidence and case-fatality from spontaneous intracerebral hemorrhage in a southern region of Portugal. J Neurol Sci. 2017;380:74-78.
- [Google Scholar]







