Translate this page into:
Nitrum komitake: An interesting case of thunderclap headache
*Corresponding author: Akhil Sahib, Department of Neurology, Govind Ballabh Pant Institute of Post Graduate Medical Education and Research, New Delhi, India. akhilsahib03@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhury C, Sahib A. Nitrum komitake: An interesting case of thunderclap headache. J Neurosci Rural Pract. 2024;15:610-1. doi: 10.25259/JNRP_59_2024
Dear Editor,
We hereby report the case of a 67-year-old female, a well-controlled diabetic and hypertensive, with Kellgren and Lawrence Stage IV osteoarthritis of both knees, planned for sequential total knee replacement arthroplasty, right followed by the left, under combined epidural spinal anesthesia. The patient was turned to the right lateral decubitus position and injected with hyperbaric 0.5% bupivacaine at L3-L4 subarachnoid space to achieve regional block. Immediately post-procedure, the patient developed sudden-onset thunderclap headache with a visual analog scale score of 9 – 10, more prominent over the vertex with one episode of vomiting. On examination, blood pressure was 150/90 mmHg, pulse – 96/min, and saturation (Spo2) – 96% on room air. Glasgow’s coma scale score was 15, with no signs of meningeal irritation. Her motor strength was normal without any lateralizing features. There was no history of peri-procedural sneezing, coughing, or Valsalva maneuver. She was managed with injectable analgesic and anti-emetics and shifted for a non-contrast computed tomography (NCCT) head. The computed tomography head revealed a pneumocephalus involving the right frontal region without any bony fracture [Figures 1a and b] and multiple air locules along bilateral cavernous sinus, right anterior temporal bone, and posterior fossa [Figures 2a and b]. The patient was shifted to the intensive care unit for observation and managed with bed rest at Fowler’s position at 30°, high flow oxygen, analgesics, prophylactic anti-epileptics, and avoidance of Valsalva maneuver and gradually improved within three days with no residual headache or deficits.
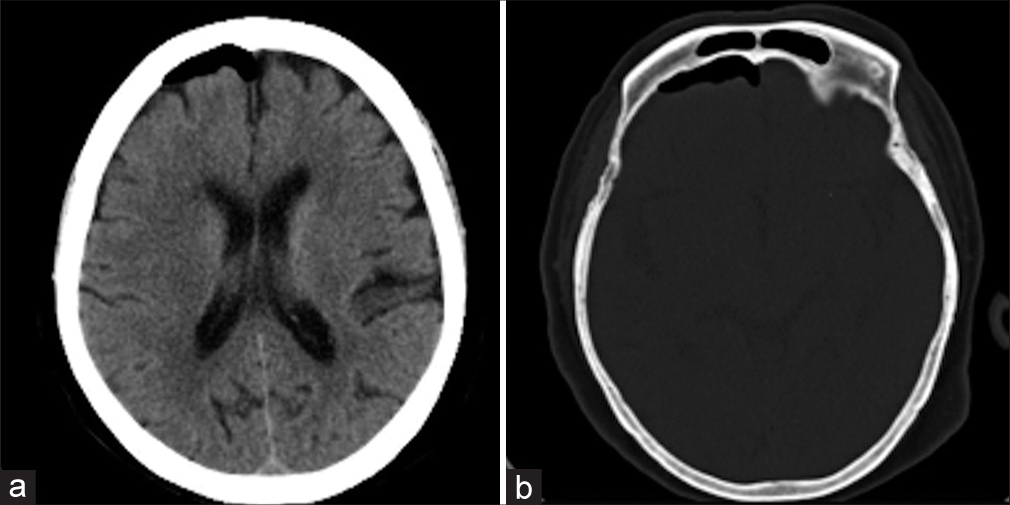
- (a) Non-contrast computed tomography head showing air collection in right anterior frontal region. (b) Bone window showing no calvarial breach.

- (a) Non-contrast computed tomography head showing multiple air locules in bilateral cavernous sinus, cerebellar folia, and right anterior temporal lobe. (b) Base of skull shows no fracture.
Pneumocephalus is common following trauma involving the skull base, cranial vault or neurosurgical procedures but is a rare complication after an epidural puncture.[1] The common differentials of thunderclap headache include subarachnoid hemorrhage, reversible cerebral vasoconstriction syndrome, cerebral venous sinus thrombosis, and interestingly pneumocephalus too.[1] The intracranial space is a pressurized closed system, and disruption to this system, as in dural puncture, causes air to penetrate through the dural defect by ball valve mechanism due to high external pressure, which overcomes the intracranial pressure. Once inside the skull, by virtue of negative intracranial pressure, the air gets sucked in by the inverted soda bottle effect to balance the pressure differential.[2] Thunderclap headache post-epidural anesthesia should be immediately assessed for pneumocephalus, which is treatable and reversible. Other symptoms of pneumocephalus may include syncope, seizures, agitation, delirium, vomiting, and decreased levels of consciousness.[2,3] On the basis of magnetic resonance imaging alone, the diagnosis of pneumocephalus may be more difficult due to the lack of objective density measurement. Gas will appear completely dark on all sequences, but depending on the location and morphology can be wrongfully diagnosed for blood product or flow voids. As less as, 0.55 mL of air within the cranial vault can be detected by NCCT head.[4] In our case, Tuohy needle of 18-gauge was used to identify the epidural space using loss of resistance to air technique, followed by dural puncture with a smaller size spinal needle. The dura could have inadvertently been punctured by the 18-gauge epidural needle itself during the procedure leading to the complications.[3]
Usually, in 85% of cases of pneumocephalus, there is resorption of air with conservative management only. In the absence of resorption, hyperbaric oxygen therapy can be useful. Surgical management is indicated in case of tension pneumocephalus, symptomatic pneumocephalus, or recurrent pneumocephalus.[5] Most of the cases of pneumocephalus reported so far resulted from accidental dural puncture due to loss of resistance technique using air.[3] To prevent pneumocephalus, identifying the epidural space with saline has been recommended.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Pneumocephalus: Case illustrations and review. Neurocrit Care. 2010;13:152-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pneumocephalus after epidural injection. J Emerg Med. 2018;54:e45-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pneumocephalus following combined spinal epidural anaesthesia for total knee arthroplasty: A case report. Malays Orthop J. 2017;11:42-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pneumocephalus in patients with orthostatic headache. J Clin Neurol. 2008;4:89-93.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of hyperbaric oxygenation therapy on symptomatic pneumocephalus. Ther Clin Risk Manag. 2014;10:769-73.
- [CrossRef] [PubMed] [Google Scholar]





