Translate this page into:
Multilocular peripheral neuropathy with delayed symptom progression and neuropathic pain after lightning strike
-
Received: ,
Accepted: ,
How to cite this article: Gdynia H, Bauer A, Schimpf N, Wagner DM. Multilocular peripheral neuropathy with delayed symptom progression and neuropathic pain after lightning strike. J Neurosci Rural Pract. doi: 10.25259/JNRP_92_2024
Dear Editor,
Lightning injuries can cause multiple neurological consequences, and a variety of cerebral and cerebellar syndromes have been described.[1] Furthermore, cranial nerve syndromes,[2] autonomic syndromes,[3] spinal cord disorders,[4] and peripheral nerve disorders[5] are known. Unique to lightning injury is keraunoparalysis. It means a transient syndrome lasting only a few hours, which can occur in different forms.[1,6,7]
Our 59-year-old Caucasian male patient incurred a lightning strike during his job as a shepherd in the German Alps. After a primary brief loss of consciousness and a night in the forest, he was able to reach a location with cell phone reception and get help. In the emergency room, he presented with mild holocephalic headache, and slowing of speech and psychomotor functions. Neurologically, he showed a slight diffuse sensorimotor palsy of the distal left lower extremity with prominent paralysis of the foot elevation. No further deficits emerged. Somatosensory evoked potentials of the left tibial nerve were pathological. Motor nerve conduction studies demonstrated a slight axonal lesion of the left peroneal nerve, and sensory nerve study of the left sural nerve was unremarkable. There were no signs of denervation in electromyography (EMG). Spinal and cerebral magnetic resonance imaging (MRI) was unremarkable. Overall, the deficits were slight.
After one year, he showed aggravation of the leg palsy and developed a slowly progressive hypaesthesia of the fingers 4–5 of the right hand. Furthermore, moderate new distal motor ulnar nerve palsy of the right hand with aspects of ulnar claw phenomenon and mild spasticity occurred. At this time, motor nerve measurements of the right ulnar nerve were unremarkable, but no sensory ulnar nerve action potential could be detected.
The patient suffered from distinct allodynia and hyperalgesia of the right upper extremity, and the left lower leg was hypaesthesic. After an emergency admission on New Year’s Eve due to pain, the patient was referred to a specialized pain clinic where chronic neuropathic pain syndrome was diagnosed. Based on the bio-psycho-social model, a multimodal pain therapy was carried out. In addition to intensive physiotherapy and occupational therapy, this also included psychoeducation on understanding chronic pain, acceptance, and learning coping strategies. Furthermore, relaxation methods were taught, and strategies for activating resources and improving the mental state were developed.
After two years, the palsy of the right hand has aggravated severely with medical research council (MRC) grade 0 in fingers 4 and 5 and the aspect of ulnar claw phenomenon with extended metacarpophalangeal joints of the 4th and 5th fingers and flexed interphalangeal joints of the same fingers [Figure 1]. Fingers 1–3 demonstrated MRC strength grades 4–5, again mild spasticity. The palsy of the left lower extremity was severe with flaccid foot drop. He showed hypaesthesia, allodynia, and hyperalgesia of the complete left lower and right upper extremities.
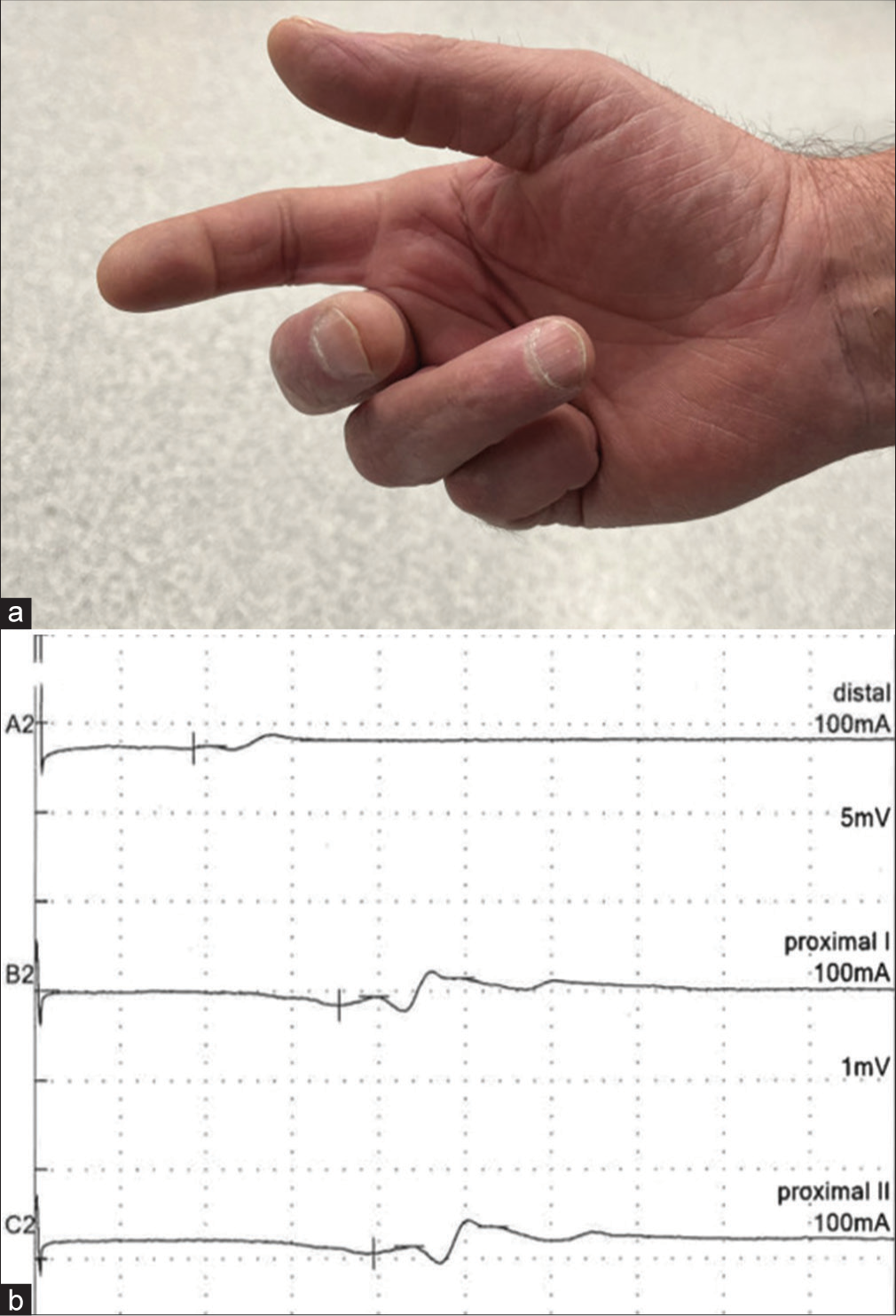
- (a) Right hand of the patient showing aspects of ulnar claw. (b) Motor nerve conduction study of left peroneal nerve with reduced compound muscle action potentials and temporal dispersion.
The results of nerve conduction studies are outlined in Table 1.
| Nerve | Stimulation site | Amplitude | Latency (ms) | NCV (m/s) |
|---|---|---|---|---|
| Motor | ||||
| Peroneal left | Ankle | 0.37 mV | 9.3 | 40.2 |
| Below fibular | 0.21 mV | 17.7 | 57.5 | |
| Above fibular | 0.23 mV | 19.75 | ||
| Tibial left | Ankle | 9.64 mV | 4.7 | |
| Popliteal fossa | 7.37 mV | 16.45 | 39.1 | |
| Ulnar right | Wrist | 15.07 mV | 3.6 | |
| Below elbow | 11.7 mV | 8.94 | 48.8 | |
| Median right | Wrist | 12.3 mV | 4.2 | |
| Elbow | 8.84 mV | 8.91 | 49.9 | |
| Sensory | ||||
| Ulnar right | Wrist | - | - | - |
| Median right | Wrist | 13.19 µv | 3.72 | 44.4 |
| Sural left | Calf | - | - | - |
mV: Millivolts, µV: Microvolts, ms: Meter/second, NCV: Nerve conduction velocity. Pathological findings are in bold letters
An EMG of the left tibialis anterior and right abductor digiti minimi muscle detected moderate spontaneous activity.
Taking anamnesis, disease course, and clinical and electrophysiological findings into account, the diagnosis of multilocular peripheral neuropathy and chronic neuropathic pain syndrome due to lightning strike was set with evidence for delayed neurological damage. Standard laboratory screening tests showed no other reasons for neuropathy such as vasculitis or diabetes. The slight aspect of spasticity of the right hand was discussed to be due to an additional affection of the central nervous system.
Therapeutically, rehabilitation treatment was established. In accordance with the chronic neuropathic pain syndrome, a medication with an anticonvulsant was started, and night-time sleep was supported with a tricyclic antidepressant.
The patient was able to walk slowly with walking sticks, but he could not use his right hand in activities of daily living. Hence, retirement proceedings have been initiated, as the patient will not be able to work as a shepherd again. The quality of life was stated by the patient to be sufficient.
Delayed neurological symptom presentation and progression is a seldom reported and poorly understood phenomenon after lightning or electrical injury.
The development of late-onset motor neuron disease (MND) after electric injury has been described.[8] The MNDs relating to electric injuries are largely referred to as delayed onset syndromes, and some authors reported years of delay before onset.[1,8] Reisner provides and reviews hypotheses to help explain this phenomenon. He concluded that in cases with delayed damage of vascular origin, there are possibly free radicals resulting from oxidative stress, which may damage spinal vascular endothelial cells, cutting off blood supply, and ending in the death of spinal neurons. Furthermore, he discusses free radicals from oxidative stress formed directly from the lipids found in abundance in myelin cells, when the delayed condition is demyelination.[9]
In addition to the multilocular peripheral neuropathy, our patient showed a mild spasticity of the right hand. An MRI showed no evidence of central nervous system affection, so spasticity might be due to keraunoparalysis where spasticity has been described.[1]
He also developed a severe neuropathic pain syndrome, which has, to our knowledge, not been described before due to lightning injury. Due to the fact that no specific treatment strategies are known, the focus of multimodal pain therapy was placed on acceptance and commitment to the chronic pain situation in addition to intensive physiotherapy to promote physical performance, altogether with good clinical effects regarding quality of life.
Andrew and Reisner suggest that the treatment should be covered with pharmacological agents and verbal neuropsychological strategies.[1] In our opinion, this is highly important due to the fact that the disease may have a lasting impact on life, like in our patient, not only with disabling symptoms but also retirement. A multidisciplinary rehabilitation team can best address this complex topic. With regard to a possible delayed symptom progression, we recommend that every patient should undergo long-term neurological surveillance.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There is no conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Neurological and neuropsychological consequences of electrical and lightning shock: Review and theories of causation. Neural Regen Res. 2017;12:677-86.
- [CrossRef] [PubMed] [Google Scholar]
- Autonomic nervous system dysfunction in lightning and electrical injuries. Neurorehabilitation. 2005;20:19-23.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed cervical spinal cord injury after high voltage electrical injury: A case report. J Burn Care Res. 2007;28:905-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pan-brachial plexus neuropraxia following lightning. A rare case report. Surg Neurol Int. 2015;6:110-2.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed reversible motor neuronopathy caused by electrical injury. J Chin Med Assoc. 2008;71:152-4.
- [CrossRef] [PubMed] [Google Scholar]
- A case of keraunoparalysis: A bolt from the blue. Indian J Crit Care Med. 2018;22:804-5.
- [CrossRef] [PubMed] [Google Scholar]
- Motor neuron disease after electric injury. J Neurol Neursurg Psychiatry. 2001;71:265-7.
- [CrossRef] [PubMed] [Google Scholar]
- Possible mechanisms for delayed neurological damage in lightning and electrical injury. Brain Inj. 2013;27:565-9.
- [CrossRef] [PubMed] [Google Scholar]





