Translate this page into:
Assessment of verbal (conventional) training versus models training for head frame fixation in neurosurgery
*Corresponding author: Deepak Kumar Jha, Department of Neurosurgery, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. jhadeepak2@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal M, Katiyar V, Sharma RK, Janu V, TotalaP, Jha A, et al. Assessment of verbal (conventional) training versus models training for head frame fixation in neurosurgery. J Neurosci Rural Pract. doi: 10.25259/JNRP_536_2023
Abstract
Cranial immobilization is an essential first step in cranial surgeries. Complications related to head fixation frames are under-reported and given less importance during training. Authors report their experience of using verbal (Conventional) training and training by models of “head fixation frame” and “wooden head” for head frame application for cranial surgeries. Models of the “Head Fixation Frame” (Mayfield clamp) and “wooden human head” were made using metal (iron) and wood, respectively. Major craniometric landmarks and dural venous sinuses were marked on the head model. A total of 15 trainee residents of >18 months (Group A, n = 4), < 18 months (Group B, n = 5), and without neurosurgical training (Group C, n = 6) were assessed for head frame application on human cadaver heads after verbal (conventional) training (n = 8) and training on models (n = 7). Various parameters, such as time taken for pin application, selection of pin site, and quadrants, were evaluated for adequacy of pin placements and position of head. Both methods were compared for assessment of better training method. Model training for head frame fixation was found better with regard to all aspects out of which time for positioning the head and for pin application, selection of quadrants of the head, site for pin insertions, and need of intervention by faculty were significant. Training on models of “head fixation frame” and “head” is better than conventional training. It is simple and safe and will prevent pin-related complications.
Keywords
Head fixation
Model
Mayfield head frame
Skull clamp
Head immobilization devices
INTRODUCTION
Pin-type head frame systems are commonly used in neurosurgical procedures for the optimal and rigid positioning of the head.[1] They hold the patient’s head in a suitable and stable position (e.g., supine, lateral, or prone) during intracranial and spinal surgeries. The use of a head frame to provide rigid fixation also facilitates accurate neuronavigation and has become universally accepted for safety considerations during surgical procedures.[2] The two most commonly used cranial fixation devices are the Mayfield and Sugita head frames.[3] The three-pin Mayfield head frame is the most popular pin-type head frame and is equipped with a force gauge integrated into the torque screw on the side with one pin.[4] Although fixation devices are very useful, they have been associated with adverse effects.[5,6] Despite them being under-reported due to medicolegal reasons, several complications related to the pin-type head frame are reported in the literature, including venous air embolism, skull fracture with or without intracranial hematoma, traumatic pseudoaneurysm of the superficial temporal artery, alopecia, pin-site infections, scalp lacerations, and head slippage.[7,8]
There is very limited literature regarding head frame fixation in neurosurgery and training aspects for the same is relatively a neglected area.[9-11] Authors used handmade models of “head fixation frame” and “head” for training purposes and compared their effectiveness in learning in comparison to the verbal (conventional) method.
MATERIALS AND METHODS
A total of 15 trainees were involved in the assessment study. These were divided into:
Group A: Trainee residents of neurosurgery with >18 months of experience
Group B: Trainee residents of neurosurgery with <18 months of experience
Group C: Trainee residents with no experience of neurosurgery. These were on rotation postings in the department of neurosurgery from other surgical departments.
At the institute, where the study was done, trainee residents join after a minimum of three years of general surgery training and each resident gets both clinical and operative exposures in outdoor clinics, inpatient wards and operation rooms (ORs) as observers/assistants. Eighteen months’ cutoff was chosen, as the total tenure for neurosurgical training is for three years (36 months). After 18 months, the trainees perform selected surgeries under supervision. However, head fixation training is given in the OR right from the beginning of the neurosurgical training, and they are involved in the head fixation in the OR under the supervision of the faculty of Neurosurgery. Faculty members (7 in number) follow the verbal training of head fixation during pre-operative planning sessions and in the OR are based primarily on the article by Fung.[9] Although there were no objective criteria to assess the pre-training knowledge of the trainees, overall concepts of head fixation in each group of trainees before (Group A) and after 18 months (Group B) of training in neurosurgery grossly are similar. Group C was third year trainees of general surgery, who had no knowledge of head fixation for neurosurgical procedures.
Each group was further subdivided into two subgroups: verbal training subgroup and model training subgroup. Principles and techniques of head fixation were explained for pterional craniotomy, retromastoid suboccipital craniotomy (RMSOC), and Midline sub-occipital craniotomy (MLSOC) verbally to the “verbal subgroup” and by demonstrating it on the models of Mayfield clamp and wooded head (made by senior author DKJ) to the “model subgroup” as described by Fung[9] and Thijs and Menovsky.[11] After verbal or model training, trainees of both the subgroups of Groups A, B, and C used actual Mayfield clamp for cadaver head fixation for each of the three craniotomies.
Group A had two residents in each subgroup (n = 4), Group B had three in verbal training and two in model training subgroup (n = 5), and Group C had three residents in each verbal and model training subgroup (n = 6).
The model of the Mayfield clamp [Figure 1a] was made using iron metal with functional pin application systems. The head model [Figures 1a and b] was made of wood on which the zygoma, superior nuchal line, superior temporal line, and coronal sutures were marked for training purposes. The Cadaver head and actual Mayfield clamp were used for the evaluation of the trainees [Figure 1c]. The following seven aspects of the cadaver head fixation technique by Mayfield clamp were evaluated for Pterional craniotomy, RMSOC, and MLSOC, and all the observations were recorded on an excel work-sheet:
Time taken for pin placement
Time taken in positioning the head
Number of attempts for pin placement
Whether the pins (two pins swivel and single pin) were applied on opposite quadrants [Figure 2]
Whether the pins were applied on the sweatband line[9] or Linea Temporalis Latitude:[11] Pin application on a virtual band formed by frontal eminences, parietal eminences, the highest point of superior temporal lines, and opisthocranium was observed
Pin placement: The pin should not be over the midline, and temporalis muscles were observed
Need for intervention: Intervention by faculty to rectify the error was observed.
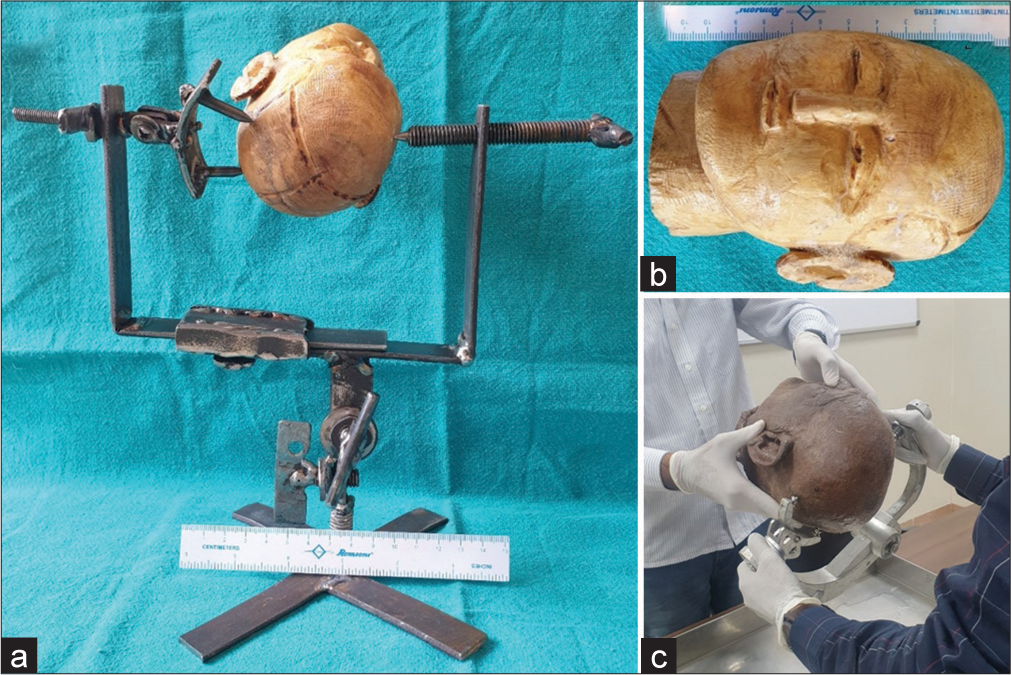
- (a) Handmade model of Mayfield head frame made up of iron metal with functional pin application system with a wooded head fixed in it for left pterional craniotomy. (b) A wooden head and neck model with surface landmarks (left coronal suture and superior temporal lines are visible partially). (c) Cadaver head being fixed by a trainee for left pterional craniotomy for assessment study.
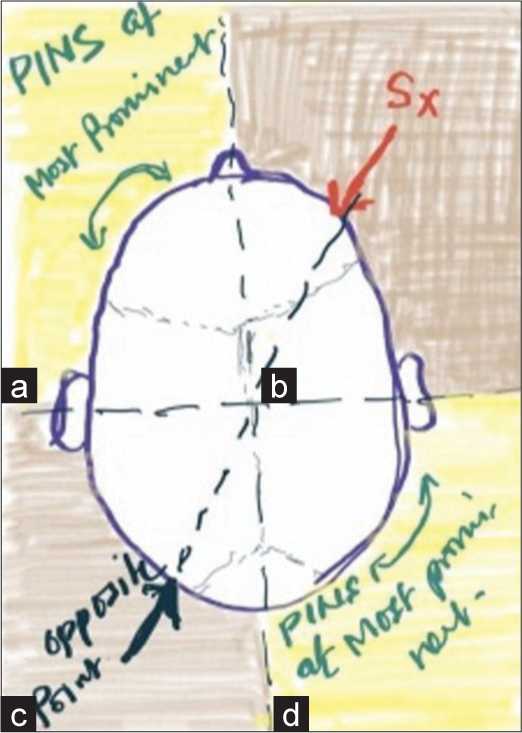
- Line diagram showing four quadrants of head with example of planning right pterional craniotomy. Pin applications should be done in adjacent quadrant to the area of interest (Sx). (a) Left anterior quadrant – site of application of single, non-dependent pin. (b) Right anterior quadrant – surgical area. (c) Left posterior quadrant (opposite quadrant) – no pins should be applied on the opposite quadrant. (d) Right posterior quadrant – site of application of two dependent pins. PINS: Pins of head frame, Sx: Surgical site.
Trainees in the model training subgroup used the model of the Mayfield clamp to fix the model head for Pterional craniotomy, RMSOC, and MLSOC after explaining the technique as per the literature.[9,11] Pin sites and head positions on the models were checked by the faculty. Any error in the application of the pins was explained. Verbal (conventional) method of training was given to the verbal training subgroup as described by Fung[9] and Thijs and Menovsky.[11]
Pin quadrants
While selecting sites for pin application, the head was divided into four imaginary quadrants, and pins were applied in adjacent quadrants to the surgical field [Figure 2]. No pin was applied on the surgical quadrant and quadrant opposite to the surgical field [Figure 2]. Two pins swivel were placed first on the dependent part of the head followed by the single pin, which was applied on the non-dependent part of the head. An imaginary line was considered for pin application, which joins both frontal eminences, highest points of superior temporal lines, parietal eminences, and opistho-cranion as described by Fung.[9] The insertion sites of the head pins were avoided in areas with thin bone, such as the frontal sinus and temporal squama, and just above the arteries of the scalp and venous sinuses as mentioned by Thijs and Menovsky.[11]
The cost of making the models was miniscule, and it was approximately less than a dollar (USD) for one set of both head-neck and head frame models; however, it may vary in other countries.
“The R Foundation for Statistical Computing,” (R Version 4.2.2, Vienna, Austria) was used for statistical analysis. The “Kruskal–Wallis rank sum test” and “McNemar’s Chi-squared test” were used for sub-group analysis and comparison between groups. P < 0.05 was considered as significant.
RESULTS
The overall assessment of head frame application after verbal and model training is summarized in Table 1. Almost all seven parameters in the model training group showed improvements in the application of the head frame. Improvements were significant in all aspects except attempts for pin placement and pin equator selection. Overall, the time taken for both pin placements and head positioning was nearly half in the model training group in comparison to the verbal training group. The number of attempts of pin applications was nearly 55% less in the model training group when compared to the verbal training group, though it was not significant. Similarly, overall model training scored better in the selection of equator, site of pin application, and needed lesser intervention by faculty to rectify the error.
| S. No. | Assessment method | Verbal training (SD) | Model training (SD) | P-value |
|---|---|---|---|---|
| 1. | Time taken for pin placement (min) | 1.7960317 (0.6971550) | 0.9388889 (0.3353826) | NS |
| Pt | 1.7571429 (0.6216657) | 0.8642857 (0.1869414) | 0.0034 | |
| MLSOC | 1.6380952 (0.7756547) | 0.7619048 (0.2652243) | 0.02 | |
| RMSOC | 1.9928571 (0.7455955) | 1.1904762 (0.3908511) | 0.023 | |
| 2. | Time in positioning (min) | 0.8285714 (0.3877694) | 0.4666667 (0.1548297) | NS |
| Pt | 0.7571429 (0.2892931) | 0.4595238 (0.1356934) | 0.017 | |
| MLSOC | 0.6119048 (0.3710239) | 0.3333333 (0.0481125) | 0.088 | |
| RMSOC | 1.1166667 (0.3497353) | 0.6071429 (0.1239239) | 0.0085 | |
| 3. | Attempts for pin placement | 53 | 29 | NS |
| 4. | Pin quadrants (C/W) | 18/3 | 21/0 | 0.0005202 |
| 5. | Pin equator (C/W) | 8/13 | 19/2 | NS |
| 6. | Pin placement (C/W) | 3/18 | 15/6 | 0.0002795 |
| 7. | Need for intervention (Yes/no) | 20/1 | 11/10 | 0.000568 |
SD: Standard deviation, Pt: Pterional, MLSOC: Midline suboccipital craniotomy, RMSOC: Retro-mastoid suboccipital craniotomy, NS: Non-significant (P>0.05), C/W: Correct/Wrong. Bold values signify p-values, which are significant (<0.05).
The subgroup analysis of trainees based on their level of seniority is summarized in Table 2. Beneficial effects of model training were observed in all three groups irrespective of their experience; however, it was significantly more effective in groups B (P = 0.0058) and C (P = 0.00011) for the time taken for pin placement, for all groups for the time taken for positioning of the head (P = 0.00071). Group C group trained by models had significantly fewer attempts for correct pin application (P < 0.05). In the remaining aspects, though model training was beneficial, the method of training had no association with the level of experience (seniority).
| S. No. | Steps Assessed | AV | AM | BV | BM | CV | CM | P-value |
|---|---|---|---|---|---|---|---|---|
| 1. | Time taken for pin placement in minutes (SD) | 1.4527778 (0.4967021) | 1.0083333 (0.2480479) | 1.2444444 (0.4075219) | 0.6416667 (0.1778732) | 2.3925926 (0.4900476) | 1.0907407 (0.3565957) | Group A/B/C: NS/0.0058/0.00011 |
| 2. | Time in Positioning in minutes (SD) | 0.3916667 (0.0735980) | 0.5555556 (0.2670137) | 0.5555556 (0.2670137) | 0.4305556 (0.1529040) | 1.1092593 (0.3377942) | 0.5407407 (0.1748235) | 0.00071 |
| 3. | Attempts of Pin placement | Group A/B/C | ||||||
| a. Pterional | 4 | 2 | 4 | 2 | 9 | 5 | NS/NS/0.03389 | |
| b. MLSOC | 3 | 3 | 4 | 2 | 9 | 4 | NS/NS/0.03389 | |
| c. RMSOC | 4 | 3 | 5 | 3 | 11 | 5 | NS/NS/0.04311 | |
| 4. | Pin Quadrants (Correct/Wrong) | |||||||
| a. Pterional | 2/0 | 2/0 | 2/0 | 2/0 | 2/1 | 3/0 | NS | |
| b. MLSOC | 2/0 | 2/0 | 2/0 | 2/0 | 2/1 | 3/0 | NS | |
| c. RMSOC | 2/0 | 2/0 | 2/0 | 2/0 | 2/1 | 3/0 | NS | |
| 5. | Pin Equator (Correct/Wrong) | |||||||
| a. Pt | 2/0 | 2/0 | 1/1 | 2/0 | 1/2 | 2/1 | NS | |
| b. MLSOC | 2/0 | 2/0 | 0/2 | 2/0 | 0/3 | 3/0 | NS | |
| c. RMSOC | 2/0 | 2/0 | 0/2 | 2/0 | 0/3 | 2/1 | NS | |
| 6. | Pin Misplacement (midline, temporalis muscle or both) | |||||||
| a. Pt | 2 | 0 | 1 | 0 | 3 | 1 | NS | |
| b. MLSOC | 1 | 1 | 1 | 0 | 3 | 1 | NS | |
| c. RMSOC | 2 | 1 | 2 | 1 | 3 | 1 | NS | |
| 7. | Need for Intervention (for Pin site, pin position or both) | |||||||
| a. Pt | 6 | 0 | 4 | 0 | 9 | 6 | NS | |
| b. MLSOC | 1 | 1 | 2 | 0 | 9 | 3 | NS | |
| c. RMSOC | 6 | 1 | 6 | 3 | 9 | 8 | NS | |
AV: Verbal training to trainee resident>18-month experience in Neurosurgery, AM: Model training to trainee resident>18-month experience in Neurosurgery, BV: Verbal training to trainee resident<18-month experience in Neurosurgery, BM: Model training to trainee resident <18-month experience in Neurosurgery, CV: Verbal training to trainee resident without experience in Neurosurgery, CM: Model training to trainee resident without experience in Neurosurgery, SD: Standard deviation, Pt: Pterional, MLSOC: Midline suboccipital craniotomy, RMSOC: Retro-mastoid suboccipital craniotomy, NS: Non-significant.
DISCUSSION
Head fixation is one of the most important aspects of intracranial surgery, especially skull base and posterior fossa surgeries. These procedures require an accurate understanding of the anatomy of the scalp and skull.[12] Many factors are to be considered during choosing the pinning sites for head fixation. These include the orientation of the head fixation device, the surgical approach intended, gravity forces for brain retraction, relevant craniometric points, previous craniotomy flaps if any, burr holes, shunt devices, tubings, and thin skull bones.[11] There is a learning curve for head frame application, which needs practice and supervision. Inappropriate pin application can result in multiple punctures of the scalp and the skull with subsequent potentially serious hazards for the patients.[13] Several complications are attributable to the use of the head fixation clamps. The most common complications are skull fractures with accompanying epidural hematomas, bleeding, pneumocephalus, skull fracture, and hardware breakage.[13] Rarely, these can lead to lethal complications, which mostly are related to vascular injury.[11] The under-reporting of these complications is likely due to medicolegal implications.[11] Despite under-reporting of complications of head fixation devices, the Food and Drug Administration, in February 2016, declared in a safety communication that more than 1000 incidences were reported to result in more than 700 injuries.[13] There are rare reports which provide detailed techniques to apply head frames in various surgical approaches.[9,10,14] Training of head frame application is a matter of transferred experience, which is insufficient for trainees across the globe.[13]
The selection of seven aspects of head clamp fixation was especially based on difficulties observed by the trainees during head clamp applications in the OR, which led to delay in starting surgery (time taken for pin application and head positioning, number of attempts for correct pin application), causes unnecessary pin applications with avoidable scalp invasion, which needs change in the site of pin/s (selection of quadrants and equator), awkward positioning of the head leading to difficulty in exposure and surgery (quadrants and equator), obstruction of the surgical field by the head frame itself (quadrants and equator), and scalp lacerations and rarely acute subdural hematoma in one case in our experience in a routine surgery for cerebellopontine angle epidermoid in a 68-year-old male [Figure 3]. It is important to remember that in elderly patients, dura is adherent to the cranium and there are chances of acute subdural hematoma instead of extradural hematoma, which is more likely in younger age groups, as reported in earlier studies.[15]

- Axial computed tomography scan of head showing bilateral acute subdural hematoma (left more than right) with ventricular dilatation in a post-operative patient of the right cerebellopontine angle epidermoid due to pin of head clamp (Sugita head frame)
Overall, our study included most of the aspects related to the head frame pin application including head positioning. Replicating the head position and head frame application practiced on a model during pre-operative planning session is simple and does not need the trainees to remember all points important for it. They simply need to replicate the same in the OR over the patients’ heads and over the period they also understand all the practically relevant points for safe head clamp application and head positioning. It is important to mention that during the study, we trained them only once on the model for each of the three craniotomies and all the observations are after that only. Regular practice on models before each surgery may be more effective for them for easy and safe applications of head frame and head positioning. Practice on cadavers may not be feasible at many centers and models appear an effective alternative for practicing head frame application and head positioning. Models of head fixation clamp and head-neck enable pre-hand determination of appropriate scalp and skull pinning sites. Practicing head fixation on these hand-made models is easy, safe, and helpful. This helps trainees to learn head frame application in a structured fashion by the senior neurosurgeons and ultimately will prevent most of the complications related to the pins. Selection of Pterional craniotomy, RMSOC, and MLSOC were because these are common surgical approaches and pin sites and head positions are important in these craniotomies.
Fung[9] have mentioned an imaginary line, which includes frontal eminence, superior temporal line, parietal eminence, and opisthocranion. This line is also described as a sweatband line.[10] Various locations on the head are to be avoided for pin applications, such as temporal squama, frontal sinuses, and mastoid bone, which have been mentioned in the literature, which are relevant.[7,10,16]
Application of pins in adjacent quadrants to the surgical field helps in applying pins at equidistance from the surgical area of interest. It helps in applying pins in diagonally opposite directions to each other perpendicular to the skull surface. Application of two pins on the dependent quadrant results in an even distribution of load (force of pins and gravitational force due to the weight of the head), which will reduce chances of penetration of pins inside the skull due to pressures applied during various surgical maneuvers and will decrease chances of intraoperative head slippage/dislodgement. Mayfield head frame’s arc of the two pin-swivel makes the perimeter and single pin makes the center. Mayfield head frame is used around the world, which too is a three-pin system and is considered an effective equipment for head fixation.
There are two obvious limitations of the study. The first is the total number of trainees, which were 15 and only 8 and 7 in the verbal and the model training subgroups. The reason was that the study was done at a busy neurosurgical center with a limited number of trainees. Another issue is the assumption of a similar level of knowledge, understanding, and capabilities of application of head clamp on the cadaver head before either method of training among various groups. All the trainees of groups A and B are routinely exposed to a variety of surgical approaches during their training which includes description of head clamp application on patients in OR.
Authors are aware that making handmade models require skill and artwork and may not be feasible for all except a few neurosurgeons. The senior author (DKJ) also made a simple Sugita type iron arc frame with tapped four holes and functioning screws [Figure 4a], which can be a simple three-pin practice model. Similarly, the senior author has made variety of models of head frame (both Mayfield and Sugita types) and head made up of Acrylonitrile Butadiene Styrene (ABS) plastic [Figure 4b], used in three-dimensional printers, or combinations of wood, metal and ABS plastic for training of neurosurgery residents. Authors are aware that a complicated functioning miniaturized head frame and head model [Figure 4] may not be easy to make, but the same can also be made by local artisans with little guidance and supervision of the neurosurgical team. These practicing models should also be made available in the market for training in neurosurgery, which is possible only if it is demanded by neurosurgeons.
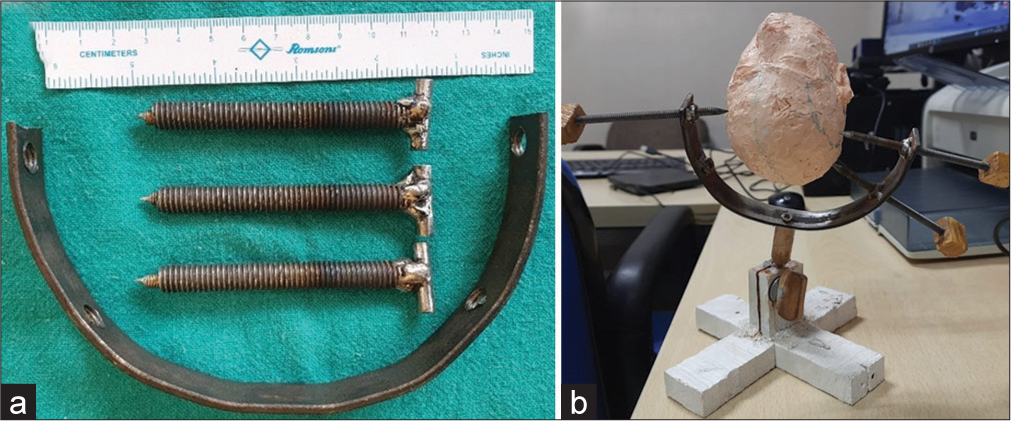
- (a) Simple iron metal model of Sugita type head frame arc with three functional pins, which may be used for training for head frame application. (b) Metal model of Sugita head frame with functional pin application system holding a head model made by three-dimensional (3D) pen using acrylonitrile butadiene styrene filament used in 3D printers.
CONCLUSION
Head frame application and head positioning are important in neurosurgical training to avoid difficulties in surgery due to inappropriate head positions and complications associated to application of pins. Practicing head frame fixation and head positioning on the models is safe, inexpensive and will help reduce chances of errors in head positions and reduce incidences of pin-related complications.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Respond of the different human cranial bones to pin-type head fixation device. Acta Neurochir (Wien). 2021;163:885-93.
- [CrossRef] [PubMed] [Google Scholar]
- Difference between conventional head-pin and Dispo-pin in the Sugita multipurpose head frame system. Neurol Med Chir (Tokyo). 2013;53:21-5.
- [CrossRef] [PubMed] [Google Scholar]
- Use of cranial fixation pins in pediatric neurosurgery. Neurosurgery. 2008;62:913-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pinning in pediatric neurosurgery: The modified rubber stopper technique. J Neurosurg Pediatr. 2020;26:98-103.
- [CrossRef] [PubMed] [Google Scholar]
- Depressed skull fractures in children secondary to skull clamp fixation devices. Pediatr Neurosurg. 1994;21:174-8.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of the Mayfield skull clamp. Anesthesiology. 1984;61:460-1.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic aneurysm of the superficial temporal artery as a complication of pin-type head-holder device. Case report. Surg Neurol. 1999;52:400-3.
- [CrossRef] [PubMed] [Google Scholar]
- Alopecia due to an allergic reaction to metal head-pins used in a neurosurgical operation. Surg Neurol Int. 2016;7(Suppl 1):S5-7.
- [CrossRef] [PubMed] [Google Scholar]
- Rigid head fixation In: Rabbe A, Meyer B, Schaller K, Vajkoczy P, Winkler PA, eds. The craniotomy atlas. Stuttgart: Thieme; 2019. p. :20-4.
- [Google Scholar]
- Skull clamp placement: Introduction. 2014. Available from: https://www.youtube.com/watch?v=EUevdYSc4ik [Last accessed on 2022 Oct 01]
- [Google Scholar]
- The Mayfield skull clamp: A literature review of its complications and technical nuances for application. World Neurosurg. 2021;151:102-9.
- [CrossRef] [PubMed] [Google Scholar]
- Important points for patient positioning and head fixation in cerebral aneurysm surgery. No Shinkei Geka. 2021;49:24-30.
- [Google Scholar]
- FDA urges caution with neurosurgical head holders due to slippage. Available from: https://www.raps.org/regulatory-focus%e2%84%a2/news-articles/2016/2/fda-urges-caution-with-neurosurgical-head-holders-due-to-slippage [Last accessed on 2022 Oct 11]
- [Google Scholar]
- A novel method for safe and accurate placement of the rocker pins of head immobilization devices utilizing a digital caliber phantom: Technical note. Childs Nerv Syst. 2019;35:1599-602.
- [CrossRef] [PubMed] [Google Scholar]
- Pin site bilateral epidural hematoma. A rare complication of using Mayfield clamp in Neurosurgery. Neurol India. 2011;59:649-51.
- [CrossRef] [PubMed] [Google Scholar]
- Air embolism from wounds from a pin-type head-holder as a complication of posterior fossa surgery in the sitting position. Case report. J Neurosurg. 1981;55:147-8.
- [CrossRef] [Google Scholar]






