Translate this page into:
A Comparative Study to Evaluate the Efficacy of Virtual Versus Direct Airway Assessment in the Preoperative Period in Patients Presenting for Neurosurgery: A Quest for Safer Preoperative Practice in Neuroanesthesia in the Backdrop of the COVID-19 Pandemic!
Unnikrishnan Prathapadas, MD, PDCC Division of Neuroanesthesia, Department of Anesthesiology 1st Floor, C Block, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum 695011 India drunnikrishnanp@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Objectives Neurosurgical patients with cervical spine pathologies, craniofacial and craniovertebral junction anomalies, recurrent cervical spine, and posterior fossa surgeries frequently present with an airway that is anticipated to be difficult. Although the routine physical evaluation is nonaerosol-generating, Mallampati scoring, mouth opening, and assessment of lower cranial nerve function could potentially generate aerosols, imposing a greater risk of acquiring severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection. Moreover, airway evaluation requires the patient to remove the mask, thereby posing a greater risk to the assessing anesthesiologist. Thus, we designed this study to evaluate the efficacy of virtual airway assessment (VAA) done via telemedicine in comparison to direct airway assessment (DAA), and assess the feasibility of VAA as a part of the preanesthetic evaluation (PAE) of patients presenting for neurosurgery in the backdrop of the COVID-19 pandemic.
Materials and Methods A total of 55 patients presenting for elective neurosurgical procedures were recruited in this prospective, observational study. The preoperative assessment of the airway was first done by a remote anesthetist via an encrypted video call, using a smartphone which served the purpose of telemedicine equipment, followed by a direct assessment by the attending anesthetist. The following parameters were assessed: mouth opening (MO), presence of any anomalies of tongue and palate, Mallampati classification (MPC) grading, thyromental distance (TMD), upper lip bite test (ULBT), neck movements, and Look-Evaluate-Mallampati-Obstruction-Neck mobility (LEMON) scoring system.
Statistical Analysis Demographic parameters were expressed as mean ± SD. Agreement between the values obtained by VAA and DAA parameters were analyzed with the Kappa test.
Results We observed a “perfect agreement” between the DAA and VAA with regard to MO. Assessment of ULBT, neck movements, and the LEMON score had an overall “almost perfect agreement” between the DAA and VAA. We also observed a “substantial agreement” between VAA and DAA during the assessment of MPC grading and TMD.
Conclusion Our study shows that PAE and VAA via telemedicine can reliably be used as an alternative to direct physical preanesthetic consultation in the COVID-19 scenario. This could reduce unnecessary exposure of anesthesiologists to potential asymptomatic COVID-positive patients, thereby protecting the available skilled workforce, without any significant compromise to patient care.
Keywords
virtual airway assessment
COVID19
telemedicine
neurosurgery
Introduction
Preoperative airway assessment of patients undergoing anesthesia is an integral part of safe anesthesia practice.1 The purpose of which is to evaluate the patient's airway, in order to plan an appropriate and safe technique to secure the airway. Multiple factors contribute to a difficult airway, especially in patients presenting for neurosurgery. Patients with cervical spine pathologies, craniofacial and craniovertebral junction (CVJ) anomalies, as well as patients coming for recurrent cervical spine and posterior fossa surgeries frequently present with an airway that is anticipated to be difficult.1 2 Moreover, a difficult airway when poorly managed predisposes to hypoxemia and hypercarbia, attributing to secondary neurological injury. Preoperative airway assessment necessitates the employment of various airway grading systems such as Mallampati classification (MPC), thyromental distance (TMD), inter incisor distance, upper lip bite test (ULBT), and evaluation of the range of neck movements.2 3 4 5
Anesthesiology has embraced the use of telemedicine as a means to perform preoperative evaluations for the last two decades.6 7 8 9 10 11 However, this has been restricted to appraising the medical and surgical history, reviewing medications, and focusing on the need for optimization of comorbid conditions. In the context of the COVID-19 pandemic caused by severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2), a safe practice during the preoperative airway assessment is essential to prevent disease transmission. Many institutions have developed safety protocols for health care workers, especially for those involved in aerosol-generating procedures (AGP) such as anesthesiologists. Although the routine physical evaluation is a non-AGP, the evaluation of airway principally, the Mallampati scoring, and assessment of lower cranial nerve function could generate aerosols, thus imposing a greater risk of acquiring the deadly virus. Moreover, airway evaluation requires the patient to remove the mask, posing a greater risk to the assessing anesthesiologist.
Although there are isolated reports wherein real-time video was used for preoperative airway assessment, no studies have been done comparing the predictability of airway assessment parameters by direct physical assessment to the virtual airway assessment (VAA) done via telemedicine.6 7 8 9 10 11 12 13 Thus, we designed this study to evaluate the efficacy of VAA in comparison to direct airway assessment (DAA), and assess the feasibility of VAA as a part of the preanesthetic evaluation of patients presenting for neurosurgery in the backdrop of the COVID-19 pandemic.
Materials and Methods
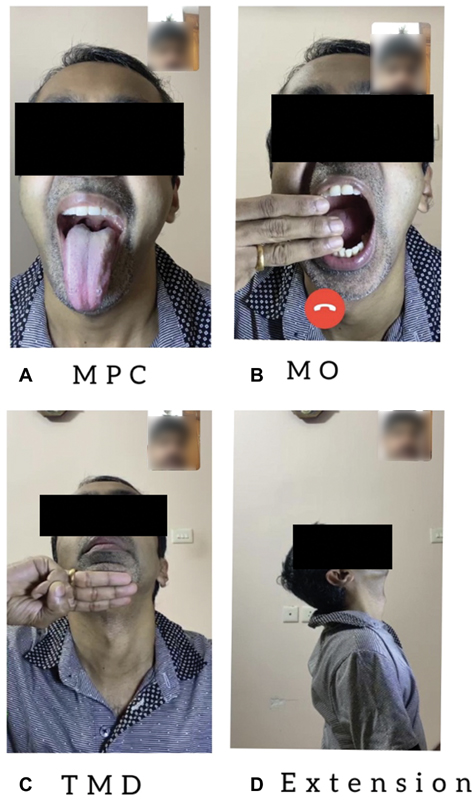
After obtaining approval from the Institutional Ethics Committee, 55 consenting patients in the age group of 18 to 65 years, presenting for elective neurosurgical procedures were recruited in this prospective, observational, pilot study. Patients presenting for surgical management of supratentorial lesions, cervical spine pathologies, posterior fossa lesions, and skull base endoscopic surgeries were included in this study. Patients with altered sensorium and psychological abnormalities were excluded from the study. An anesthesiologist, who was not assigned to the case, performed the VAA component of the study via a video call averaging approximately 5 to 10 minutes in duration with the help of a smartphone. The video call was facilitated at the patient end with the help of a mobile smartphone (M2001C3K31, Xiaomi Inc, Haidian, Beijing, China) with a high-definition camera (8MP front camera. f/2.0 aperture,1.12 mm pixel size, video recording 1920 × 1080 @ 30 fps) capable of real-time both-way video and audio communications, which was held by an adjustable holder fixed on the bedside infusion stand (Fig. 1). The patient was seated in the neutral position, with the camera positioned at the same level of the patient's face and was asked to look straight into the camera for the entire duration of the evaluation. The snapshots of different evaluation techniques during the video call using the WhatsApp (WhatsApp LLC, California, United States) application are hypothetically represented in Fig. 2. The patient (represented by one of the authors) shown in the foreground in each picture is being examined by the anesthesiologist whose image appears on the right upper corner. The real-time video call was performed, and data transmission was within the institutional firewall and AES-128 encrypted (certified by the US Department of Defense). Staff at the neurosurgical ward received training in the setting up and use of the telemedicine equipment, along with patient positioning needed for the airway examination, to facilitate completion of the VAA.

-
Fig. 1 Figure showing the patient being evaluated through a video call with a smartphone held by an adjustable holder fixed on the bedside infusion stand.
Fig. 1 Figure showing the patient being evaluated through a video call with a smartphone held by an adjustable holder fixed on the bedside infusion stand.
-
Fig. 2 Figure showing the hypothetical snapshots of different airway evaluation techniques during the video call: (A) Mallampati classification (MPC) (B) mouth opening (MO) (C) thyromental distance (TMD) (D) Neck extension.
Fig. 2 Figure showing the hypothetical snapshots of different airway evaluation techniques during the video call: (A) Mallampati classification (MPC) (B) mouth opening (MO) (C) thyromental distance (TMD) (D) Neck extension.
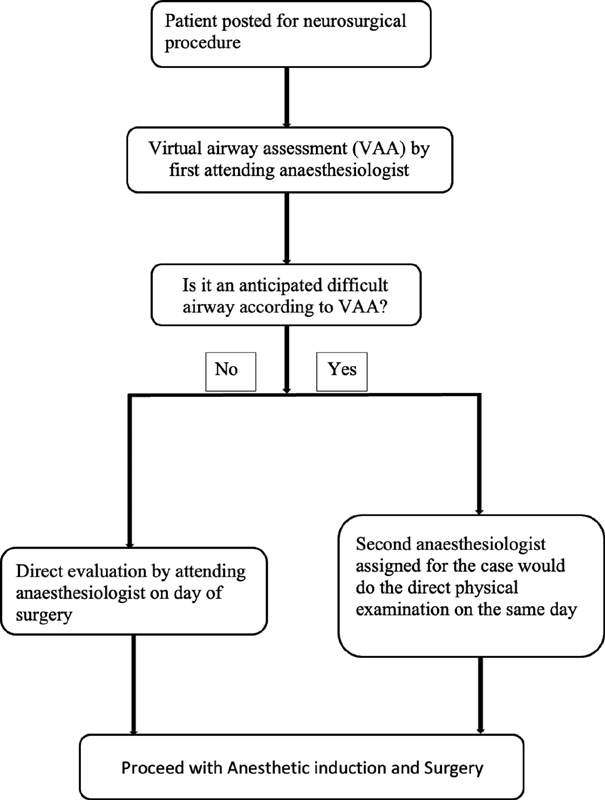
On the day of the surgery, before induction of anesthesia, the attending anesthesiologist with an appropriate level of personal protective equipment (PPE) conducted a DAA. The procedure by which the patient's VAA and DAA were done is elaborated in the preoperative airway assessment flowchart (Fig. 3). The data was collected by both the anesthesiologists who had performed the VAA and the attending anesthesiologist and comparative analysis was done.
-
Fig. 3 Algorithm used for the preoperative airway assessment of patients enrolled in this study.
Fig. 3 Algorithm used for the preoperative airway assessment of patients enrolled in this study.
Parameters Observed
The following parameters were assessed in addition to the demographic details: the history of obstructive sleep apnea, reactive airway disease, hoarseness of voice, stridor, and history of previous maxillofacial surgeries/cervical spine surgeries/head and neck surgeries. The assessment included facial features, mouth opening (MO), presence of any anomalies of tongue and palate, Mallampati scoring, TMD, ULBT, neck movements, and the Look-Evaluate-Mallampati-Obstruction-Neck mobility (LEMON) scoring system.
Statistical Analysis
SPSS 16 (IBM Corporation, 2019) software was used for analysis. Demographic parameters were expressed as mean ± SD. Results were considered to be statistically significant when p < 0.05 and p < 0.001 was considered highly significant. Agreement between the values obtained by VAA and DAA parameters were analyzed with Kappa test which, when compared with percentage agreement, is a better measure of interassessor and intra-assessor reliability.14 Kappa can range from − 1 to + 1, where 0 represents the amount of agreement that can be expected from random chance, and 1 represents perfect agreement between the assessors. Kappa is interpreted further as values ≤ 0, indicating no agreement, 0.01 to 0.20 as none to slight, 0.21 to 0.40 as fair, 0.41 to 0.60 as moderate, 0.61 to 0.80 as substantial, and 0.81 to 1.00 as almost perfect agreement.
Results
Fifty-five patients were recruited for the study with a mean age of 48.6 ± 18.5 years. The gender characteristics, neurosurgical procedures, and the incidence of comorbidities in the study population are described in Table 1. There was no statistically significant difference in the gender of the patients (54.5% males vs. 45.5% females). The mean body mass index (BMI) was 25.1 ± 5.3 kg/m2. Patients recruited in this study had a MO of either 2 or 3 fingers breadth on the VAA, which correlated well with the results of DAA (Kappa = 1, p = < 0.001, perfect agreement) Concerning MPC grading of the airway, the VAA agreed with the DAA in 78.9% of patients who had MPC grade 1, in 85.7% of patients who had MPC grade 2, and in 81.8% of patients who had MPC grade 3. In the case of MPC grade 4, the VAA agreed only in 25% (1 out of 4 patients) with DAA. In this circumstance, 3 out of 4 patients (75%), who were found to have MPC 4 using VAA, turned out to be class 3 in DAA. Additionally, 3 out of 4 patients (75%) found to have a grade of MPC 4 using DAA had been graded as MPC 3 in the VAA. However, the overall combined data of all observations (MPC 4) showed substantial agreement (Kappa = 0.68, p = < 0.001, Table 2).
|
Parameters |
Number (n) |
Percentage (%) |
|
|---|---|---|---|
|
Gender |
Male |
30 |
54.5 |
|
Female |
25 |
45.5 |
|
|
Type of neurosurgery |
Supratentorial |
21 |
38.2 |
|
Cervical spine |
16 |
29.1 |
|
|
Posterior fossa |
13 |
23.6 |
|
|
Endoscopic |
5 |
9.1 |
|
|
Comorbidities |
Diabetes |
9 |
16.3 |
|
Hypertension |
7 |
12.7 |
|
|
Endocrine disorders |
5 |
9.1 |
|
|
Coronary artery disease |
2 |
3.63 |
|
|
VAA (MPC) |
DAA (MPC) |
Total as per VAA in each MPC category |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
MPC 1 |
MPC 2 |
MPC3 |
MPC4 |
|||||||
|
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
|
|
MPC 1 |
15 |
78.9 |
3 |
14.3 |
0 |
0.0 |
0 |
0.0 |
18 |
32.7 |
|
MPC 2 |
4 |
21.1 |
18 |
85.7 |
0 |
0.0 |
0 |
0.0 |
22 |
40.0 |
|
MPC 3 |
0 |
0.0 |
0 |
0.0 |
9 |
81.8 |
3 |
75.0 |
12 |
21.8 |
|
MPC 4 |
0 |
0.0 |
0 |
0.0 |
2 |
18.2 |
1 |
25.0 |
3 |
5.5 |
|
Total as per DAA in each MPC category |
19 |
100.0 |
21 |
100.0 |
11 |
100.0 |
4 |
100.0 |
55 |
100.0 |
Abbreviations: DAA, direct airway assessment; MPC, Mallampati classification; VAA, virtual airway assessment.
In the assessment of TMD, for patients having TMD of 2 fingers breadth, DAA agreed with the VAA in 100% of the study population. Moreover, in 86.7% of the patients with TMD of 3 fingers breadth and 87.5% of patients with TMD of > 3 fingers breadth, DAA agreed well with the VAA. Overall, it showed substantial agreement for TMD in our study population (Kappa = 0.66, p = < 0.001, Table 3). In the ULBT, the VAA agreed with the DAA in 97.1% of the subjects with class 1 and 100% of the subjects with class 2. Overall, it showed almost perfect agreement (Kappa = 0.96, p = < 0.001). Evaluation of the neck movements showed an almost perfect agreement (Kappa = 0.84, p = < 0.001, Table 4). Finally, for LEMON scores of 0 to 3, the VAA agreed with the DAA in all the patients and 60% of the subjects with a LEMON score of 4. Overall, there was an almost perfect agreement with regard to the LEMON score (Kappa = 0.94, p = < 0.001, Table 5).
|
VAA (TMD) |
DAA (TMD) |
Total as per VAA in each TMD category |
||||||
|---|---|---|---|---|---|---|---|---|
|
2 fingers breadth |
3 fingers breadth |
> 3 fingers breadth |
||||||
|
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
|
|
2 fingers breadth |
2 |
100.0 |
0 |
0.0 |
0 |
0.0 |
2 |
3.6 |
|
3 fingers breadth |
0 |
0.0 |
39 |
86.7 |
1 |
12.5 |
40 |
72.7 |
|
> 3 fingers breadth |
0 |
0.0 |
6 |
13.3 |
7 |
87.5 |
13 |
23.6 |
|
Total as per DAA in each TMD category |
2 |
100.0 |
45 |
100.0 |
8 |
100.0 |
55 |
100.0 |
Abbreviations: DAA, direct airway assessment; TMD, thyromental distance; VAA, virtual airway assessment.
|
VAA (neck extension) |
DAA (neck extension) |
Total as per VAA in each category of neck movement |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
20 degrees |
25 degrees |
30 degrees |
35 degrees |
|||||||
|
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
|
|
20 degrees |
2 |
100.0 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
2 |
3.6 |
|
25 degrees |
0 |
0.0 |
15 |
100.0 |
2 |
9.1 |
0 |
0.0 |
17 |
30.9 |
|
30 degrees |
0 |
0.0 |
0 |
0.0 |
16 |
72.7 |
0 |
0.0 |
16 |
29.1 |
|
35 degrees |
0 |
0.0 |
0 |
0.0 |
4 |
18.2 |
16 |
100.0 |
20 |
36.4 |
|
Total as per DAA in each category of neck movement |
2 |
100.0 |
15 |
100.0 |
22 |
100.0 |
16 |
100.0 |
55 |
100.0 |
Abbreviations: DAA, direct airway assessment; VAA, virtual airway assessment.
|
VAA |
DAA |
Total as per VAA in each category of LEMON score |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
LEMON 0 |
LEMON 1 |
LEMON 3 |
LEMON 4 |
|||||||
|
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
Number (n) |
Percent (%) |
|
|
LEMON 0 |
32 |
100.0 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
32 |
58.2 |
|
LEMON 1 |
0 |
0.0 |
13 |
100.0 |
0 |
0.0 |
0 |
0.0 |
13 |
23.6 |
|
LEMON 2 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
|
LEMON 3 |
0 |
0.0 |
0 |
0.0 |
5 |
100.0 |
2 |
40.0 |
7 |
12.7 |
|
LEMON 4 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
3 |
60.0 |
3 |
5.5 |
|
Total as per DAA in each category of LEMON score |
32 |
100.0 |
13 |
100.0 |
5 |
100.0 |
5 |
100.0 |
55 |
100.0 |
Abbreviations: DAA, direct airway assessment; LEMON, Look-Evaluate-Mallampati-Obstruction-Neck mobility; VAA, virtual airway assessment.
Discussion
Airway assessment is a crucial part of any preanesthetic evaluation (PAE), requiring definite and unique skillsets for effective interpretation of findings. Thus, it is essential to test the concurrence of VAA with DAA. In this study designed to address this void, we observed that there is no significant difference in the quality of the airway evaluation via telemedicine (VAA) compared with direct physical consultations (DAA). We observed a “perfect agreement” between the direct examination and virtual evaluation with regard to MO. Assessment of ULBT, neck movements, and the LEMON score had an overall “almost perfect agreement” between the DAA and VAA. Although the agreement in the case of Mallampati grade 4 showed lesser levels of agreement, the combined analysis of all the classes showed “substantial agreement.” We attribute the lower level of correlation in MPC grade 4 to reduced ambient room light, which caused a “shadowing” effect, resulting in erroneously diagnosing MPC grade 3 in DAA as MPC grade 4 in VAA. The use of an external, tiltable light source fixed on the same stand, focusing light into the oral cavity, could further improve the quality of the video, especially during MPC grading. We also observed “substantial agreement” between VAA and DAA during the assessment of TMD.
Even though we have undertaken the study on the backdrop of a global pandemic, it has applications in slightly different scenarios as well. Dilisio et al assessed the technique of using a smartphone for preoperative evaluation when more advanced telemedicine equipment was not easily accessible.7 They advocated this as a valuable tool for anesthesiologists. For them, the preoperative interview frequently happens over the telephone on the evening before the planned procedure. Here, a smartphone-based evaluation will provide the ability to perform a physical examination, especially of the airway, and hence provide crucial data regarding the feasibility of office-based anesthesia. This is important in patients presenting with obesity, previous history of head and neck surgeries, and cervical spine pathologies. This modification in the interviewing technique permits the anesthesiologist to anticipate and prepare for a difficult airway, reducing surgical delays and case cancellations.
Fishman et al evaluated patient's preferences for telemedicine versus direct physical examination for PAE using a questionnaire, as they had observed that many American Society of Anesthesiologists (ASA) I and II patients had complaints about the additional cost and loss of time in travel for direct physical PAEs.15 They found that patients were divided in opinion, as some patients had a concern about privacy during telemedicine interviews. As of today, most videoconferencing software has end-to-end encryption. This fact and the additional safety layers added by the hospital (e.g., encryptions in the local data network) to protect the privacy of the patient during a telemedicine interview can be highlighted in the patient information sheet for clarification. Based on the findings of this study, we ensured data and privacy protection for all the subjects enrolled in our study and took a detailed informed consent.
Wong et al studied 10 consecutive patients via telemedicine-based anesthetic evaluation and assessed the degree of satisfaction by the patient and anesthesiologist after the procedure.13 They found that patients and attending anesthesiologists were very satisfied with the telemedicine consultation. However, they concluded by stating the need for a randomized controlled trial to prove cost-effectiveness. By using a smartphone device, our method efficiently addresses the cost-effectiveness issue. Moreover, we compared the application of virtual PAE with conventional consultation in the same patient to bring out the exact data without any confounding factors. In addition to the assessment of statistical significance, the Kappa test assessed the agreement of direct examination with the virtual evaluation in detail. In the retrospective evaluation by Rollert et al, the efficiency of PAEs of patients presenting for dentoalveolar surgeries, using a dedicated telemedicine system, confirmed that telemedicine consultations were as reliable as those conducted by traditional methods.16 But unlike our study, the telemedicine PAE was done by nonanesthesiologists, and the data collected was not compared with the data obtained from a direct evaluation by anesthesiologists.
Available data in India suggests that nearly 70% of cases affected with COVID-19 either exhibit mild or very mild symptoms and can be missed in routine screening questionnaires. There have been numerous instances wherein patients tested negative on admission later turned positive in the immediate postoperative period. This resulted in the health care workers associated with the airway management undergoing testing to rule out COVID-19 and caused a lot of concerns for the medical personnel as well as the hospital management. The Ministry of Family Health and Welfare, Government of India, has recommended that even non-COVID facilities use mechanisms to minimize patient-provider encounters, including self-monitoring through apps, the use of a helpline, web applications, video calls, telemedicine, etc. Smartphone usage is rampant even in developing countries. A pandemic response needs a rapid implementation of safer practice alternatives, which makes it difficult for most high-volume centers to provide or design dedicated telemedicine equipment in the developing countries in a short period. Bearing this in mind, we evaluated the feasibility of a universally available, cost-effective, smartphone-based technology.
Skilled specialists like anesthesiologists are a major workforce during a pandemic; the application of telemedicine can provide an important path to the clinician's safety without compromising patient care, especially during PAE. VAA can ensure safe practice and boost the confidence of the anesthesia community during this COVID-19 pandemic. This would also prevent unnecessary wastage of additional PPE, which needs to be donned while performing an AGP/assessing a COVID-19 positive patient. The use of PPE just for a particular phase may not be rational, considering the short supply and the fact that it requires doffing and donning and change of the PPE to evaluate the next patient, in order to prevent cross-contamination.
Limitations of Our Study
We have not analyzed patient satisfaction scores to minimize the interactions with patients as part of the COVID-19 protocol followed in our institution. An added macro lens attached to the phone and the use of an additional light source attached to the stand could have improved the visualization of the oral cavity during Mallampati evaluation. To protect the privacy of the patient, we had not recorded the photos and videos of airway examinations for further assessment by different anesthesiologists, which would have resulted in improved accuracy of the telemedicine-based VAA. However, we have not evaluated the incidence of difficult airway encountered in terms of difficulty in mask holding or the Cormack–Lehane score. This could have shed more light into the validity of the observations of VAA. In addition, our sample population did not contain patients with high BMI; thus, we could not get a comparative data of DAA versus VAA in this subgroup of patients.
Conclusion
Our study shows that PAE and VAA via telemedicine can reliably be used as an alternative to direct physical preanesthetic consultation in the COVID-19 scenario. Although this was a pilot study, as we observed high index of correlation between VAA and DAA for Mallampati 1 and 2 patients, we suggest that VAA can be used as a surrogate for DAA in this subgroup. This could reduce unnecessary exposure of anesthesiologists to potential asymptomatic COVID-positive patients, thereby protecting the available skilled workforce, without any significant compromise to patient care. Further multicentric randomized trials can provide more supportive literature to strengthen the evidence we have obtained.
Conflict of Interest
None declared.
Funding This study is part of a project was funded by Sree Chitra Neuroanesthesia and Critical Care Society, a not-for-profit scientific society registered under the Societies Registration Act 1860, Kerala, India.
References
- Definition and incidence of difficult airway. St Louis: Mosby; 1996. p. :121-125. In: Airway Management: Principles and Practice.
- [Google Scholar]
- A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32(4):429-434.
- [Google Scholar]
- Sensitivity of palm print, modified mallampati score and 3-3-2 rule in prediction of difficult intubation. Int J Prev Med. 2013;4(9):1063-1069.
- [Google Scholar]
- To infinity and beyond: the past, present, and future of tele-anesthesia. Anesth Analg. 2020;130(2):276-284.
- [Google Scholar]
- Preoperative virtual screening examination of the airway. J Clin Anesth. 2014;26(4):315-317.
- [Google Scholar]
- Presurgical assessment using telemedicine technology: impact on efficiency, effectiveness, and patient experience of care. Telemed J E Health. 2019;25(2):137-142.
- [Google Scholar]
- Preadmission anesthesia consultation using telemedicine technology: a pilot study. Anesthesiology. 2004;100(6):1605-1607.
- [Google Scholar]
- Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276-282.
- [Google Scholar]
- Patient preferences on telemedicine for preanesthesia evaluation. Can J Anaesth. 2015;62(4):433-434.
- [Google Scholar]
- Telemedicine consultations in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1999;57(2):136-138.
- [Google Scholar]







