Translate this page into:
Junctional Chiasmatic Syndrome Due to Large Anterior Communicating Artery Aneurysm
Address for correspondence: Dr. Rajesh Alugolu, Department of Neurosurgery, Nizam's Institute of Medical Sciences, Hyderabad, Telangana, India. E-mail: drarajesh1306@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Even though aneurysm involving the anterior communicating artery (A Com A) was common in clinical practice, producing compressive symptoms such as visual loss was rare. We report a case, in which patient had gradually progressive visual loss with features of the junctional chiasmatic syndrome, imaging revealed partially thrombosed large A Com A aneurysm. Intraoperatively, aneurysm was found compressing the optic chiasm and right optic nerve, following clipping and decompression of the optic nerve and chiasm there was gradually improvement in the vision over 2 weeks postoperatively.
Keywords
Aneurysm
anterior communicating
junctional chiasmatic syndrome
INTRODUCTION
Optic nerve compression by aneurysms are usuallyby internal carotid artery aneurysms. However, in about 1%–3% of cases, anterior communicating artery (A Com A) aneurysms can present with visual impairment.[12] A Com A aneurysms are one of the most common causes of subarachnoid hemorrhage (SAH), but they rarely cause visual disturbances. Most aneurysms presenting with visual impairment are usually either large or giant aneurysms. The mechanism of visual loss and field defect is either compression of the optic nerve or chiasm by the aneurysm itself, or it could also be by an associated hematoma or vasospasm. We present a case of an unruptured large partially thrombosed A Com A aneurysm presenting with visual impairment.
CASE REPORT
A 48-year-old male presented with throbbing headache, waxing and waning for 6 months with impairment of vision for 2 months. He was fully conscious. His best corrected visual acuity was finger counting close to face and 6/24 in the right and left eyes, respectively. He had impaired direct pupillary reaction in the right eye. Fundi were normal. Visual field assessment showed temporal hemianopsia in the left eye [Figure 1], and right eye could not be tested due to poor vision.
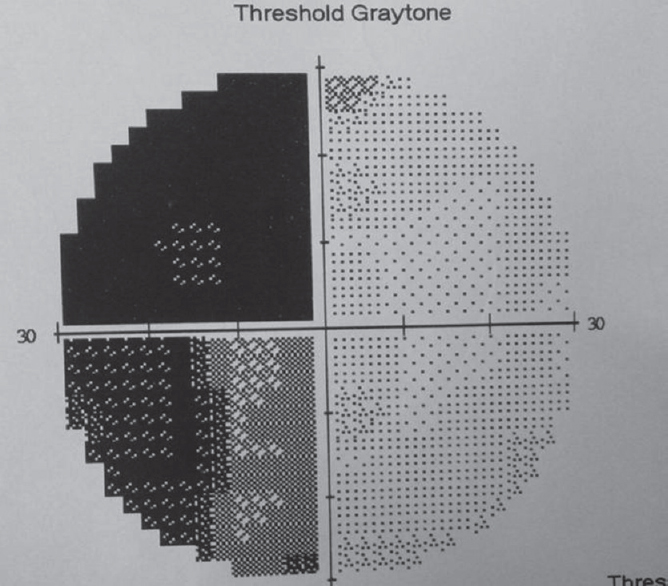
- Visual field chart in the left eye showing left temporal hemianopsia
Noncontrast computed tomography of the brain showed a hyperdense suprasellar mass of 2 cm [Figure 2]. The magnetic resonance imaging (MRI) of brain plain and contrast showed a well-defined rounded suprasellar lesion which was composed of concentric rings of differing intensities, suggestive of partially thrombosed A Com A aneurysm [Figure 3]. Digital subtraction angiography confirmed MRI findings of A Com A aneurysm measuring 8.3 mm × 8.13 mm × 9.65 mm projecting anteroinferiorly [Figure 4].
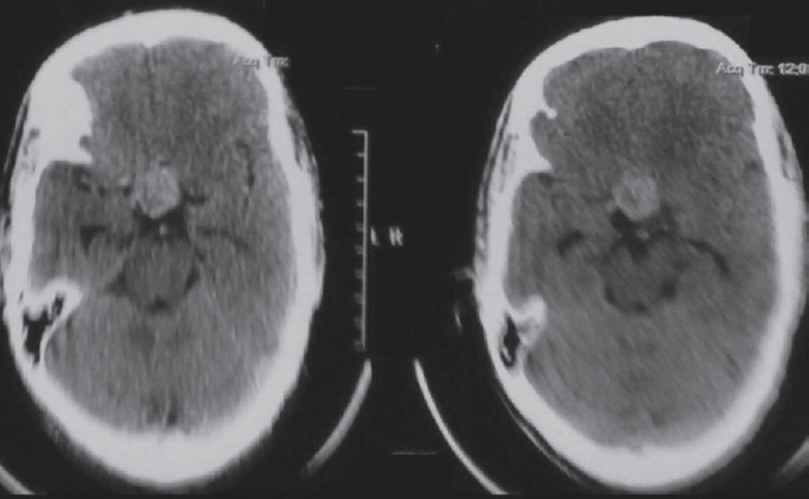
- Hyperdense lesion in suprasellar region suggestive of thrombosed anterior com artery aneurysm

- T1-weighted image showing a well-defined rounded suprasellar lesion which was composed of concentric rings of differing intensities (black arrow), suggestive of partially thrombosed anterior com artery aneurysm
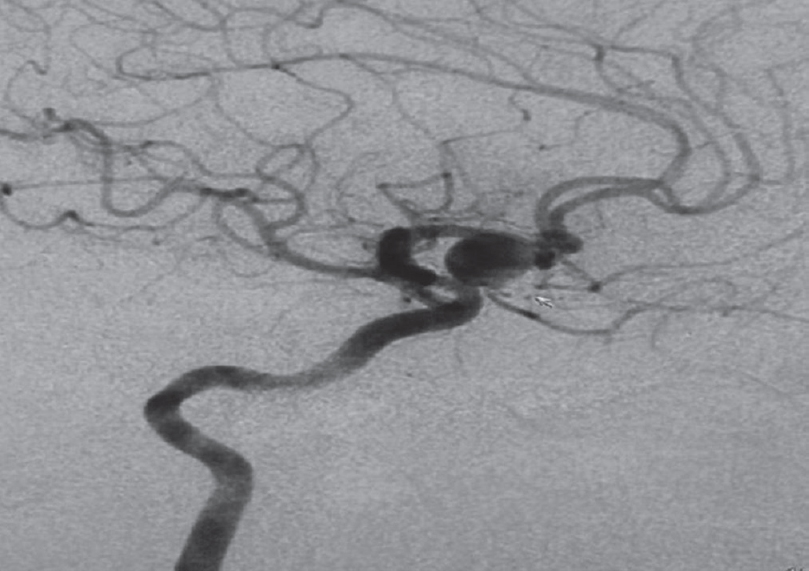
- Digital subtraction angiography, right internal carotid artery injection showing partially thrombosed anterior com artery aneurysm (white arrow)
Intraoperatively, there was mild xanthochromia of the surrounding brain tissue on the right side. There was an aneurysm extending into interoptic region, compressing the right opticochiasmatic junction. It was clipped and partially excised [Figure 5]. Postoperatively after 1 week, the patient has not reported any improvement in vision, but his headache has subsided. Two weeks after surgery, patient's vision improved to counting fingers at 2 meters.
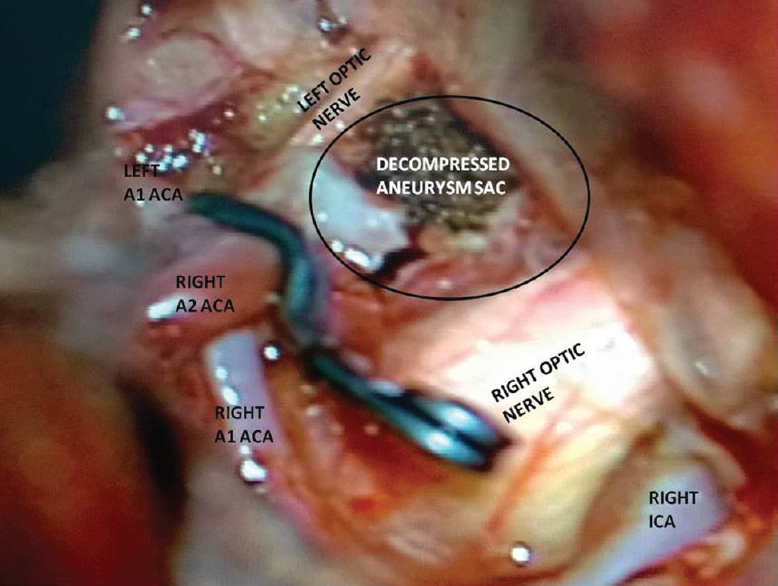
- Intraoperative image showing clipped aneurysm and decompressed sac of the aneurysm
DISCUSSION
The A Com A is the most common site of intracranial aneurysm, accounting for 26%–38% of all cerebral aneurysms.[25] Patients with a ruptured intracranial aneurysm causing SAH present with symptoms of a sudden thunderclap headache and disturbances in the level of consciousness (transient to permanent). Although A Com A aneurysms can be located close to the visual pathways, they rarely induce visual disturbances[3] ranging from 1% to 3%.[12] However, there are few reported instances in the literature where incidence of visual disturbances has been reported as high as 25%, and giant or large aneurysms were the majority accounting up to 86%.[467] However, small aneurysms of the A Com A rarely produce visual disturbance. In our case, the aneurysm was large (8.3 mm × 8.13 mm × 9.65 mm) and partially thrombosed. We hypothesize that the mechanism of visual disturbance to be direct compression of the visual pathways by the aneurysm itself. A Com A aneurysms typically compress the superior chiasmatic surface and produce macular loss and bilateral inferior field defects.[78] Alternatively, when an aneurysm ruptures, the pressure from arterial blood flow can damage the optic chiasm and nerves as much as the presence of a hematoma.[29] In our case, a large A Com A aneurysm was projecting backward and downward onto right opticochiasmatic junction.
In addition, visual impairment can be produced by ischemic damage resulting from poor blood circulation to the anterior visual pathways secondary to vasospasm or abnormality in the vessels to the optic pathway.[10]
For giant intracranial aneurysms, visual disturbance can occur with compression of the optic pathway caused by the aneurysm itself and also, from poor blood circulation caused by pressure on the vessels around the optic pathway. Moreover, minor leaks around an unruptured intracranial aneurysm can form an adhesion to the surrounding brain tissue and might compress microvessels on or around the optic pathway, causing poor blood circulation.[11]
Usually, the preferred treatment of an intracranial aneurysm with visual disturbance is to clip the neck of the aneurysm and remove the aneurysmal sac or intrasaccular hematoma and thrombus to decompress the optic pathways. In most cases, even with poor fundoscopic findings, clip ligation of the neck has a good prognosis.[5] Some authors report that it is necessary to follow patients for up to 2 years after surgery to observe recovery from the visual disturbance.[1213]
CONCLUSION
A ruptured large A Com A aneurysm can produce visual disturbance by direct compression of the aneurysm itself, by hematoma around the optic pathways, or by ischemic injury of the optic pathway caused by poor blood circulation by vasospasm or microvessel compression. Clipping of the aneurysm with decompression of the optic pathway will likely improve the visual impairment. A Com A aneurysm should be kept in the differential diagnosis for patients presenting with progressive vision loss and prompt investigation, and early treatment leads to recovery of visual impairment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cerebral aneurysms causing visual symptoms: Their features and surgical outcome. Clin Neurol Neurosurg. 1998;100:259-67.
- [Google Scholar]
- Anterior communicating artery aneurysm related to visual symptoms. J Korean Neurosurg Soc. 2009;46:232-8.
- [Google Scholar]
- A large ruptured anterior communicating artery aneurysm presenting with bitemporal hemianopsia. J Korean Neurosurg Soc. 2015;58:291-3.
- [Google Scholar]
- Intracranial aneurysms presenting with mass effect over the anterior optic pathways: Neurosurgical management and outcomes. Neurosurg Focus. 2009;26:E3.
- [Google Scholar]
- Surgically treated anterior communicating artery aneurysm. J Korean Neurosurg Soc. 2005;37:405-9.
- [Google Scholar]
- Partially thrombosed aneurysm presenting as the sudden onset of bitemporal hemianopsia. Neurosurgery. 1988;22:564-6.
- [Google Scholar]
- Giant anterior communicating artery aneurysm with bitemporal hemianopsia: Case report. Neurosurgery. 1981;8:703-6.
- [Google Scholar]
- Further concerning compression of the optic pathways by intracranial aneurysms. Clin Neurosurg. 1953;1:55-103.
- [Google Scholar]
- Pathogenesis of acute monocular blindness from leaking anterior communicating artery aneurysms: Report of six cases. Neurology. 1997;48:680-3.
- [Google Scholar]
- Visual failure following subarachnoid haemorrhage from rupture of an anterior communicating artery aneurysm. J Neurol Neurosurg Psychiatry. 1991;54:1017-8.
- [Google Scholar]
- Ischemic optic neuropathy associated with subarachnoid hemorrhage after rupture of anterior communicating artery aneurysm. Ophthalmologica. 2003;217:79-84.
- [Google Scholar]
- Carotid-ophthalmic aneurysms: Visual abnormalities in 32 patients and the results of treatment. Surg Neurol. 1981;16:1-8.
- [Google Scholar]
- Clinical manifestations, character of aneurysms, and surgical results for unruptured cerebral aneurysms presenting with ophthalmic symptoms. Acta Neurochir Suppl. 2002;82:47-9.
- [Google Scholar]






