Translate this page into:
Lateral sacral artery aneurysm
*Corresponding author: Anurag Srivastava, Department of Neurosurgery, Mahatma Gandhi University of Medical Sciences and Technology, Jaipur, Rajasthan, India. ramboanurag92@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Srivastava A, Kaushik Y, Randhawa AS, Sharma BS, Goyal G, Sherpa TD. Lateral sacral artery aneurysm. J Neurosci Rural Pract. 2024;15:373-6. doi: 10.25259/JNRP_335_2023
Abstract
A rare case of aneurysm of the lateral sacral artery is reported. This 46-year-old female presented with complaints of bowel and bladder incontinence and decreased perianal sensation for the past 15 months. She underwent laminectomy and diskectomy for the diagnosis of a prolapsed disk at peripheral hospital where the surgeon was confronted with a severe and unexpected hemorrhage, and surgery was aborted without effective treatment. Prior medical history includes hypertensive kidney disease with a renal transplant eight years ago. Magnetic resonance imaging and angiographic findings were suggestive of a lateral sacral artery aneurysm. Patient with a history of renal transplant and presenting with cauda equina require a more thorough assessment, and a differential of lateral sacral artery aneurysm should always be kept in mind. Our purpose is to report the pre-operative features of the lateral sacral artery aneurysm and its treatment modalities.
Keywords
Lateral sacral artery aneurysm
Cauda equina syndrome
Post-renal transplant
Endovascular therapy
Surgical excision
INTRODUCTION
Lateral sacral artery aneurysms are very rare and usually originate as a result of post-renal transplant high-flow trans-pelvic shunts between internal iliac arteries (IIAs).[1,2] These aneurysms may cause neurological effects due to the mass effect or as ruptured epidural hematoma.[1,2] These aneurysms are misdiagnosed and may cause severe arterial hemorrhage during surgery. We describe such a case presenting as cauda equina syndrome.
CASE REPORT
A 46-year-old female presented to our hospital with a complaint of low backache, decreased perianal area sensation, and bowel and bladder incontinence for 15 months for which she had undergone an L-S spine magnetic resonance imaging (MRI) [Figure 1a], which was suggestive of L5-S1 disk herniation and was operated (L5 laminectomy and diskectomy) for the same in an outside hospital a year ago. Prior medical history includes a renal transplant eight years back due to hypertensive kidney disease and on dialysis for a year due to graft rejection. Her low backache resolved, but she did not regain her bowel or bladder function or perianal sensations. On detailed neurological examination, her higher mental function was normal, cranial nerves were intact, tone and power were normal in all limbs, deep tendon reflexes were also normal, and sensory examination revealed loss of perianal and perineal sensations.
A repeat MRI of the L-S spine [Figure 1b and c] was done, which was suggestive of an intraspinal bilobed extradural lesion at the L5-S1 disk and S1 vertebral body level with epicenter left anterolaterally causing central canal and left lateral recess narrowing. Lesions measured about 15 × 16 × 24 mm and about 5.3 × 7.6 × 8.51 mm appeared predominately hypointense on T2-weighted images with central hyperintensity. The lesion was moderately compressing the thecal sac and left traversing S1 nerve roots. These lesions likely represent aneurysms.
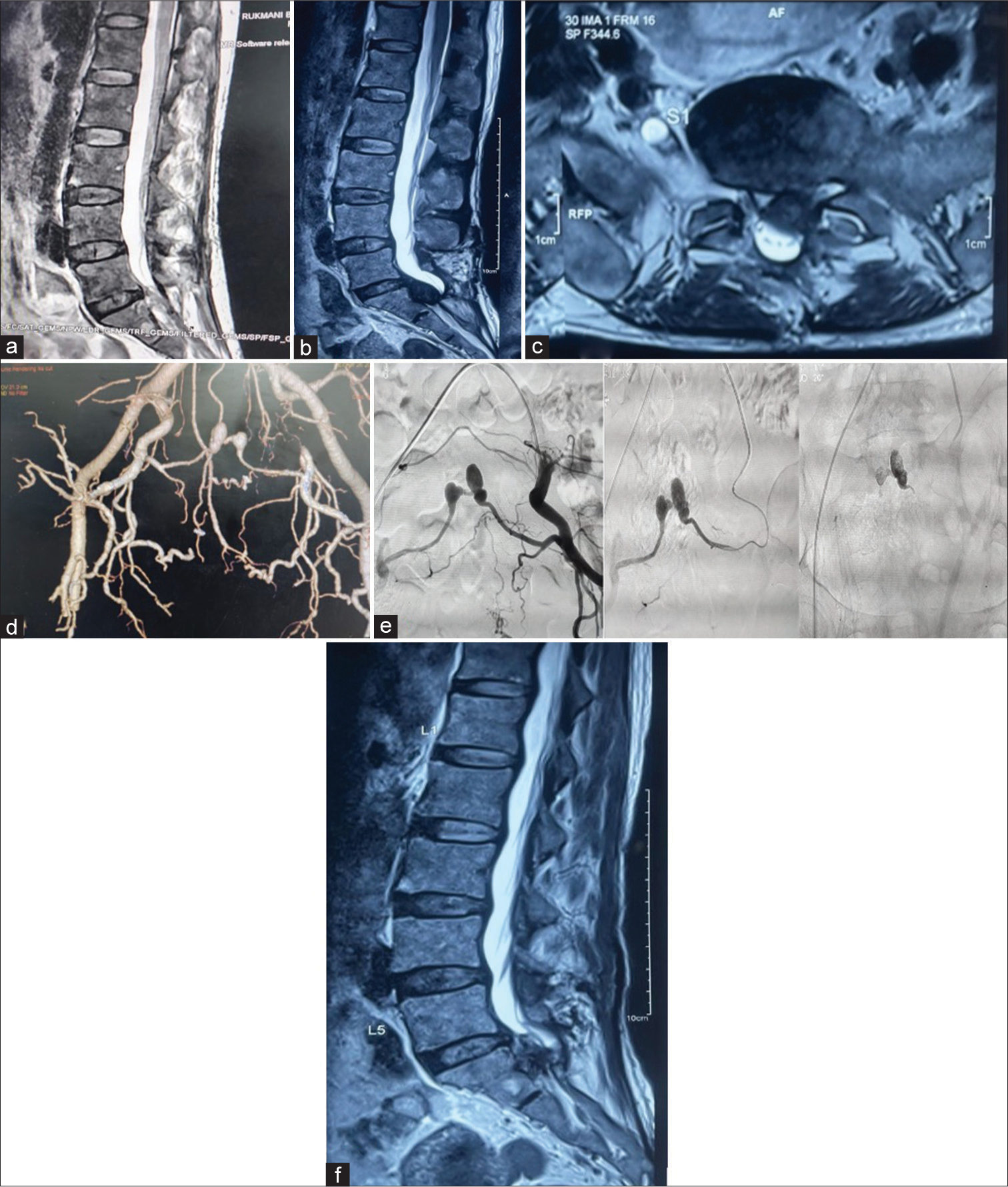
- (a) Magnetic resonance imaging (MRI) before first surgery. (b) MRI sagittal view pre-endovascular treatment. (c) MRI axial view pre-endovascular treatment. (d) 3D computed tomography angiogram showing bilobed aneurysm of the lateral sacral artery. (e) Endovascular treatment (spinal digital subtraction angiography + embolization of lateral sacral artery aneurysm). (f) MRI post-embolization.
Computed tomography angiogram of the whole spine confirmed lobulated contrast-filled outpouchings on the right and left sides communicating with each other and measuring approximately 7.9 × 8.4 × 8.7 mm and 8.2 × 7.6 × 10.6 mm, respectively [Figure 1d]. The aneurysms are seen to communicate with branches arising from the posterior division of the IIAs.
Technical notes
Endovascular (spinal angiography and embolization)
Spinal digital subtraction angiography was performed with a Cobra (5F) diagnostic catheter with Terumo guidewire through the right femoral access. Percutaneous transfemoral pelvic angiography showed complete occlusion of the right IIA after giving a branch to the transplanted kidney. The left IIA angiogram revealed an intraspinal bilobed aneurysm of the left lateral sacral artery (LSA), a branch of the IIA. Aneurysm was continued and joined the right lateral sacral artery and reconstitution of right IIA. Dimension of aneurysm was 22.2 mm (length) × 10.2 mm (width) of one lobe and 12.5 mm (length) × 11 mm (width) of another lobe. After spinal angiography, a Cobra diagnostic catheter was placed into the left IIA. The left LSA aneurysm was canulated with a Progreat microcatheter with the help of Trecess microwire. A microcatheter was placed near the origin of an aneurysm. Aneurysm was embolized with ethylene vinyl alcohol (EVHO) (Squid-12) as shown in Figure 1e. After embolization, there was complete obliteration of the aneurysm with visualization of multiple transpelvic collaterals served together to reconstitute the right IIA.
MRI (L-S) spine (Plain + Contrast): Post-embolization, no significant contrast uptake is seen. However, the lesion was causing a mass effect [Figure 1f].
Second surgery
The previous incision was reopened, partial S1 laminectomy was done, and non-pulsatile extradural mass was seen. Under operating microscopic guidance, the aneurysmal sac was dissected, opened, and the thrombus was evacuated piecemeal, and the wall was excised. No arterial feeding vessels were identified during the intraoperative course [Figure 2]. The post-operative course was uneventful, the patient had improved hypoesthesia and bowel control, but she still has bladder incontinence. The patient was discharged on post-operative day 3.
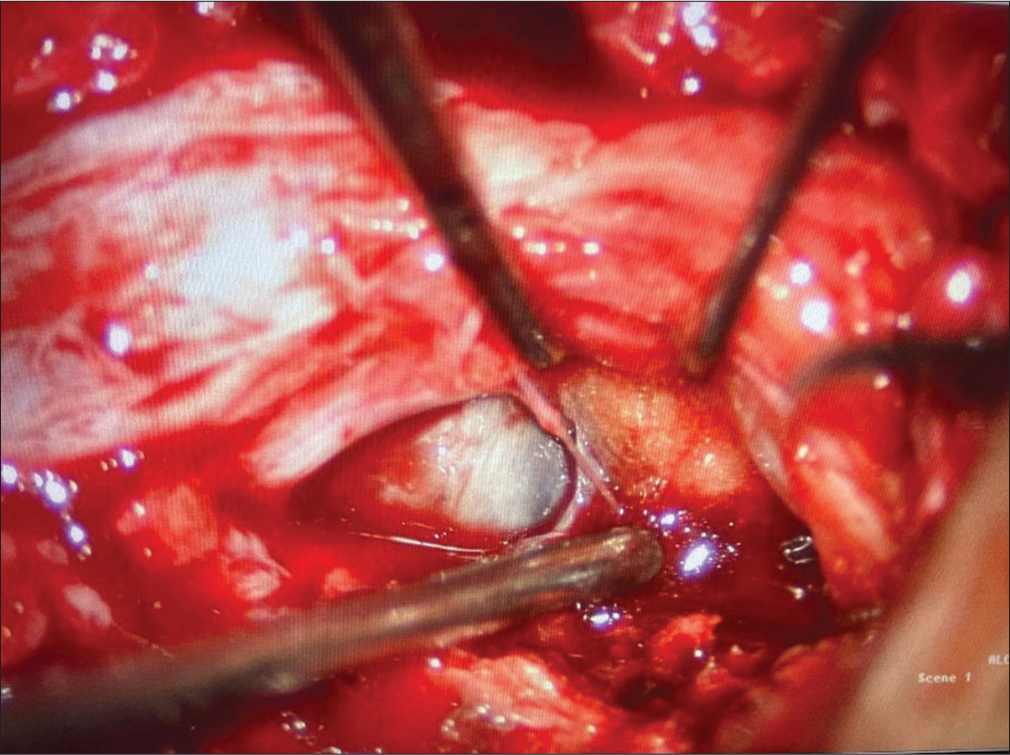
- Intraoperative surgical excision of aneurysm.
DISCUSSION
We have described an unusual lateral sacral artery aneurysm causing cauda equina syndrome in a renal transplant patient.3] There are only three such cases reported in English literature [Table 1].
| Case study | Year of publication | Age | Sex | Duration of presentation after renal transplant | Line of treatment |
|---|---|---|---|---|---|
| Schmidt et al.[2] | 1992 | 26 | F | 8 years | 1st surgery aborted → post-operative incomplete embolization → clipping of right LSA in its foramina |
| Alberstone et al.[1] | 2000 | 28 | F | 6 years | 1st surgery aborted → embolization of left LSA using three coils (incomplete coiling) → clipping and removal of aneurysm |
| Brunea et al.[3] | 2005 | 54 | M | 21 years | One failed attempt of endovascular treatment → 2nd successful attempt with endovascular injection of glue. |
| Present Case | 2023 | 46 | F | 8 years | Embolization with endovascular glue injection → complete excision of an aneurysm. |
In a study conducted by Rengachary et al., the presence of a critically stenosed segment in the left common iliac artery proximal to the graft led to the establishment of a right-to-left shunt between the IIAs ensuring sufficient blood flow to the graft. The study suggests that a hemodynamic state characterized by high blood flow may potentially lead to the development of spinal aneurysms, a phenomenon previously observed in connection with arteriovenous malformations or aortic coarctation.[4] In addition, instances of high-flow diversion following renal transplantation have been linked to extraspinal retroperitoneal hemorrhage. This occurs due to the rupture of a pseudoaneurysm located on the third lumbar artery with the involvement of cross-pelvic collateral vessels.[5]
The manifestation of such pathology can exhibit a progressive nature due to the compressive impact of the aneurysm or may present acutely. Acute symptoms may encompass intense lower back pain, cauda equina syndrome, radiculopathy or bowel/ bladder incontinence.[6] Achieving a pre-operative diagnosis has proven challenging; it went unnoticed in all four documented cases including the one under discussion. The differential diagnosis is primarily guided by the lesion’s location and the associated hematoma. Lesions appearing without hemorrhage may be erroneously identified as intradural extramedullary pathologies (such as neurofibroma, schwannoma or meningioma).[1] In addition, a ruptured vascular malformation might be considered in a patient presenting with a spinal hematoma. Diagnosis of an unruptured lateral sacral artery aneurysm is often overlooked. An MRI plays a crucial role in diagnosis revealing heterogeneous signal intensity within the aneurysm on both T1- and T2-weighted images indicating the presence of thrombus and turbulent flow.[2] A distinctive dark hemosiderin ring is typically observed within the lesion’s wall.[2] Furthermore, the location of the lesion is noteworthy, as in all four cases, it was situated posterior to the S1 vertebral body.
CONCLUSION
Lateral sacral artery aneurysms are rare. If this diagnosis is missed, it may result in catastrophic intraoperative hemorrhage. Aneurysms of the lateral sacral artery typically arise from elevated flow through transpelvic collaterals connecting both IIAs and have exclusively been documented in individuals post-renal transplantation. The lesion with hemosiderin ring behind the S1 vertebral body should raise suspicion in cases with high flow circulation and can be responsible for the neurological dysfunction by compression due to the aneurysm or subacute cauda equina or acute hematoma. Therefore, in patients with renal transplantation presenting with cauda equina syndrome, lateral sacral artery aneurysm should be suspected. A prompt utilization of MRI and angiogram is crucial for the accurate diagnosis. The mandatory occlusion of the malformation can be accomplished through embolization followed by surgical intervention in cases where the lesions cause a mass effect or persist despite endovascular therapy.
Acknowledgment
I would like to thank the Head of the Department of Neurosurgery, Dr. Bhawani Shankar Sharma sir, for his constant support and guidance, and my seniors Dr. Pankaj Gupta, Dr. Rohin Bhatia, Dr. Jitendra Verma, Dr. Shiteez Agrawal, Dr. Yogesh, Dr. Pawan Jain, Dr. Gourav Goyal, Dr. Arvind Ranwa, Dr. Pankaj Somani, and my collogues Dr. Yogesh Kaushik, Dr. Sen, Dr. Kapil, Dr. Anchal, and Dr. Anant.
Ethical approval
The research/study approved by the Institutional Review Board at Mahatma Gandhi University of Medical Sciences and Technology, Jaipur, number/MGMC&H/IEC/ JPR/2023/1781, dated 23/12/23.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Spinal aneurysm of the lateral sacral artery. J Neurosurg (Spine 1). 2000;92:101-4.
- [CrossRef] [PubMed] [Google Scholar]
- Acute cauda equine syndrome from a ruptured aneurysm in the sacral canal. J Neurosurg. 1992;77:945-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral sacral artery aneurysm: Case report and review of the literature. Neurosurgery. 2005;57:E197.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal arterial aneurysm: Case report. Neurosurgery. 1993;33:125-30.
- [CrossRef] [PubMed] [Google Scholar]
- Ruptured lumbar artery pseudoaneurysm: An unusual cause of retroperitoneal hemorrhage. Surgery. 1983;93:592-4.
- [Google Scholar]
- Operative treatment of spontaneous spinal epidural hematomas: A study of the factors determining postoperative outcome. Neurosurgery. 1996;39:494-509.
- [CrossRef] [Google Scholar]






