Translate this page into:
Is minimally invasive evacuation a future option in the management of spontaneous supratentorial intracerebral hemorrhage?
*Corresponding author: Edgar G. Ordóñez-Rubiano, Department of Neurosurgery, Fundación Universitaria de Ciencias de la Salud San José, Bogotá, Bogota, Colombia. egordonez@fucsalud.edu.co
-
Received: ,
Accepted: ,
How to cite this article: Ramos-Márquez A, Ramón JF, Gomez D, Hakim F, Ordonez-Rubiano EG. Is minimally invasive evacuation a future option in the management of spontaneous supratentorial intracerebral hemorrhage? J Neurosci Rural Pract. 2024;15:615-7. doi: 10.25259/JNRP_220_2024
Abstract
Intracerebral hemorrhage (ICH) carries a high morbidity and mortality. Historically, it has been treated medically, with specific indications for surgical management as a last resort in critical patients. Recently published literature has shown improved functional outcomes in spontaneous ICH patients managed with minimally invasive surgery (MIS) for hematoma evacuation along with medical management. Previously, surgery was believed to be a lifesaving measure; nonetheless, the doors have been opened for future implementation of MIS as a treatment option for spontaneous ICH. This raises questions on how MIS techniques may be implemented in alternative settings, including those where ICH has the highest clinical burden including lower-and middle-income countries.
Keywords
Intracerebral hemorrhage
Minimally invasive surgery
Around 10–20% of strokes are caused by spontaneous intracerebral hemorrhage (ICH) understood as brain injury caused by acute hemorrhage into the brain parenchyma.[1] It has been frequently associated with malignant hypertension in combination with neurovascular risk factors including chronic conditions such as diabetes, alcohol abuse, longstanding uncontrolled hypertension, and several others.[1,2] Locations of ICH include lobar and putaminal (25– 40%), posterior fossa (14–20%), and thalamic hemorrhages.[2] Patients usually present clinically with neurological deficits related to the hematoma location, with larger volumes of ICH generating risk for intracranial hypertension and brain herniation if not promptly managed.[2] Nonetheless, the clinical burden of spontaneous ICH is disproportionately higher in lower- and middle-income countries (LMICs) in comparison to higher income countries (HICs).[1]
ICH incidence is variable across regions; with twice the incidence in LMICs compared to HICs (22 vs. 10/100,000 population/year), in LMICs, ICH represents up to 32% of all strokes, and in HICs, ICH represents 10%.[2,3] Population-based studies have described the highest incidence in Asians (51.8/100,000), followed by the white population (24.2), black population (22.9), and Hispanic population (19).[3,4] In Latin America, there are scarce studies available; in Colombia’s System of Integrated Information of Social Protection, which collects official nationwide data provided by the Colombian Ministry of Health, and using the International Classification of Diseases, Tenth Revision codes for ICH, between 2017 and 2023, there are 58,673 cases in patients ≥18-year old found. We illustrate a clinical case managed in one of our institutions of a patient with perirolandic right frontoparietal ICH treated with minimally invasive ICH evacuation through tubular retractor systems as seen in Figure 1.
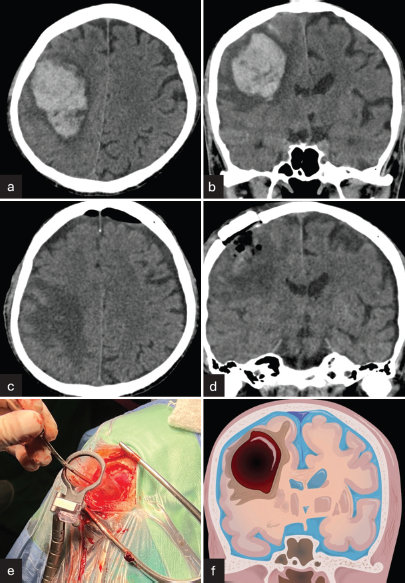
- Perirolandic right frontoparietal intracerebral hemorrhage (ICH) treated with minimally invasive intracranial hemorrhage evacuation with tubular retractor systems. (a and b) Pre-operative cranial computed tomography (CT) showing axial and coronal views of perirolandic right frontoparietal ICH, respectively. (c and d) Post-operative CT showing complete drainage of the ICH in axial and coronal views, respectively. (e) Intraoperative 3 cm craniotomy using tubular retractor system for drainage. (f) Right frontoparietal ICH illustration.
On the other hand, ICH pathophysiology includes two mechanisms of injury.[5] The first is the mass effect due to blood collection, leading to mechanical alteration and increased intracranial pressure, which can generate hydrocephalus or herniation.[1,5] Next, mitochondrial injury is generated together with altered neurotransmitter release.[5] The release of thrombin triggers the infiltration of mesenchymal cells and microglia, leading to inflammation, and secondary perihematomal edema and toxicity.[1,5] Early removal of hematomas can lead to better outcomes by helping to reduce secondary edema.[5]
Acute stroke in supratentorial intracerebral hemorrhage has been associated with high morbidity and mortality rates, with 40% survival at 1 year and 24% survival at 10 years.[3] Among described management, medical management including blood pressure lowering and anticoagulation reversal aims at limiting hematoma expansion, while surgical management aims for the prevention of further pressure-related injury and secondary injury.[1] Minimally invasive surgery (MIS) has been widely studied to treat these issues.[5] Limited data have shown craniotomy for spontaneous ICH management as a lifesaving measure in deteriorating patients, with no improvement in functional outcomes in previous randomized trials.[1,6,7]
A recent study, the Early Minimally Invasive Removal of Intracerebral Hemorrhage (ENRICH) study, was a multicentered randomized trial with patients with acute intracerebral hemorrhage in which minimally invasive hematoma evacuation was performed within 24 h after acute spontaneous intracerebral hemorrhage.[6] Trans-sulcal parafascicular MIS was carried out with image guidance and hematoma visualization for suction evacuation through a port.[6] This study showed for the first time better functional outcomes in patients with ICH at 180 days.[6] A high posterior probability of superiority of MIS evacuation of hematoma plus guideline-based medical management compared with medical management alone was found (0.981).[6]
No difference in outcomes was found based on patient groups in regard to demographic variables such as age or sex; previous studies have not shown significant differences related to these variables.[6,8] Other studies show mixed evidence for outcomes in MIS for spontaneous ICH related to age with some finding elderly patients with increased mortality and worse prognosis, but others suggesting factors such as brain atrophy and lower intracranial pressure may make elderly patients more suitable candidates for MIS.[9]
Previous studies such as the minimally invasive catheter evacuation followed by thrombolysis phase III trial, although showing no improvement in the modified Rankin scale 365 days after ICH, were pioneers in the continuous study of ICH management beyond conservative medical measures.[6] MIS techniques described for ICH have included overtime endoscopic-assisted evacuation (1989), stereotactic aspiration (2003), craniopuncture (2009), concomitant use with mechanical or chemical thrombolysis (2008, 2016, 2019), and adjunct aspiration devices along with MIS (2020).[5,10]
Minimally invasive subcortical parafascicular access for clot evacuation (MISPACE) of ICH was initially described as a means of reducing subcortical injury, with access through a port at a sulcus with orientation at the horizontal axis of white-matter tracts.[11] MISPACE benefits have included reduction of hematoma size without compromising normal tissue at risk, visualization of the deepest clot area and control of bleeding foci, more complete clot removal, and immediate intraoperative hematoma evacuation in comparison to delayed or prolonged clot reduction through the use of catheter-based thrombolytics.[11] The ENRICH trial used MIS plus guideline-based medical management for its “surgery” patient group.[6]
The technologies used for MIS continue in development, with significant barriers for implementation in LMICs with high costs and significant learning curves.[2] MIS shows great promise for the future of spontaneous ICH management, with evidence from the ENRICH trial opening the doors for implementing MIS techniques together with medical management to be considered not only as a lifesaving measure but also as a feasible treatment option.
Regardless, the applicability and accessibility to these techniques remain uncertain for applications in LMICs where feasible alternative approaches need to be studied for broad use and using the advantage of already available equipment. Specifics such as timing for evacuation, amount of hematoma evacuation, and patient selection need to be continuously studied. Among possible low-cost alternatives, manufacturing devices using tools such as three-dimensional printers similar to commercially available tubular retractors could be a feasible temporary option. Furthermore, the use of other cylindrical devices such as syringes that have a similar structure to that of tubular retractors could be potentially beneficial when aiming to perform less possible invasive surgical procedures. In addition, factors such as lower hospitalization costs should be considered to compensate for other elevated costs associated with MIS.[12]
Recent strong evidence has shown improved clinical outcomes with a MIS technique for hematoma evacuation in spontaneous ICH. While MIS for ICH management continues to be a field with ongoing research and still requires further study before its widespread use, we believe that these techniques may represent future feasible and even among first-line treatment options for patients with ICH as an alternative with lower risk of surgical subcortical injury and improved functional outcomes. Nonetheless, for its global use and application in areas such as LMICs, issues such as costs and surgical technique learning must be thoroughly considered to plan for training and even equipment alternatives or modifications for the implementation of MIS hematoma evacuation.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: A guideline From the American heart association/American stroke association. Stroke. 2022;53:e282-361.
- [CrossRef] [Google Scholar]
- How to Manage urgent neurosurgical problems in low-and middle-income countries In: Hardy MA, Hochman BR, eds. Global surgery: How to work and teach in low-and middle-income countries. Germany: Springer International Publishing; 2023. p. :257-76.
- [CrossRef] [Google Scholar]
- Minimally invasive drainage of intracerebral hemorrhage. A South American experience with the MISTIE procedure. World Neurosurg. 2022;168:95-102.
- [CrossRef] [PubMed] [Google Scholar]
- The dawn of a new era: Early minimally invasive removal of intracerebral hemorrhage. Int J Surg Open. 2024;62:282-3.
- [Google Scholar]
- Minimally Invasive intracerebral hemorrhage evacuation techniques: A review. Diagnostics (Basel). 2021;11:576.
- [CrossRef] [PubMed] [Google Scholar]
- Trial of early minimally invasive removal of intracerebral hemorrhage. N Engl J Med. 2024;390:1277-89.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive surgery for intracerebral hemorrhage. Stroke. 2018;49:2612-20.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical management of moderate basal ganglia intracerebral hemorrhage: Comparison of safety and efficacy of endoscopic surgery, minimally invasive puncture and drainage, and craniotomy. World Neurosurg. 2019;122:e995-1001.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive intracerebral hemorrhage evacuation: A bibliometric analysis of current research trends. Clin Neurol Neurosurg. 2023;227:107672.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of minimal invasive surgery treatment in hypertensive intracerebral hemorrhage: A systematic review and meta-analysis. BMC Neurol. 2018;18:136.
- [CrossRef] [PubMed] [Google Scholar]
- The safety and feasibility of image-guided brainpath-mediated transsulcul hematoma evacuation: A multicenter study. Neurosurgery. 2017;80:515.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic surgery versus craniotomy in the treatment of spontaneous intracerebral hematoma: A systematic review and meta-analysis. Chin Neurosurg J. 2022;8:36.
- [CrossRef] [PubMed] [Google Scholar]







