Translate this page into:
Intraoperative Squash Smear in Central Nervous System Tumors and Its Correlation with Histopathology: 1 Year Study at a Tertiary Care Centre
Address for correspondence: Dr. Arpita Jindal, 400 Vasundhara Colony, Tonk Road, Jaipur - 302 018, Rajasthan, India. E-mail: drarpitajindal@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Intraoperative squash smear cytology is a simple and reliable technique for rapid intraoperative diagnosis of neurosurgical specimens. The study was designed to assess the accuracy of intraoperative squash smear in the diagnosis of central nervous system (CNS) space-occupying lesions.
Materials and Methods:
One hundred and fifty cases of CNS space-occupying lesion were studied in a period of 15 months. Smears were prepared from the biopsy sample obtained at the time of operation and were stained with rapid hematoxylin and eosin method.
Results:
One hundred and forty-one cases showed complete correlation with histopathology, two cases showed partial correlation, and seven cases were discrepant. The overall diagnostic accuracy was found to be 94%.
Conclusion:
Intraoperative squash smear thus provides diagnosis with fair accuracy in brain tumors and is of great value in intraoperative consultation.
Keywords
Central nervous system tumors
cytopathology
intraoperative
squash cytology
INTRODUCTION
Central nervous system (CNS) tumors are the tenth most common tumors in adults constituting 1.3% of all cancers and are the seventh leading cause of mortality in the developed countries.[1] Intraoperative cytology preparation was first introduced by Eisenhardt and Cushing in the early 1930 and Badt in 1937. CNS tumors are very soft and gel-like in consistency. This feature is exploited in squash smear as cytological details are easily seen in smears. Intraoperative squash smear technique is a very simple and rapid tool for diagnosis of brain tumors. The present study was undertaken to assess the accuracy of intraoperative squash smear technique for CNS tumors.
MATERIALS AND METHODS
The study was undertaken in the Department of Neurosurgery and Pathology. One hundred and fifty cases of CNS space-occupying lesions were studied over a period of 15 months, from September 2013 to November 2014. The tissue obtained at the time of operation was crushed between the two clean glass slides with a pressure sufficient to spread the tissue into a film by the resident pathologist. The smears were then fixed in 95% alcohol for 2 min and then stained with rapid hematoxylin and eosin staining method. The smears were reported by the consultant pathologist taking into consideration the clinical and radiological findings, and the diagnosis was intimated to the neurosurgeon. Remaining tissue submitted for histopathology was later correlated with intraoperative cytology diagnosis by the same pathologist.
RESULTS
The study was a prospective study of 150 CNS space-occupying lesions, which included 76 males and 74 females. The age ranged from 4 months to 73 years. The prevalence of CNS tumors in the study is depicted in Figure 1. Cytological and final diagnoses on paraffin sections are summarized in Table 1. Out of 150 cases studied, histopathological diagnosis was compatible with the cytological diagnosis in 141 cases. Remaining seven cases showed discrepancy and two cases showed partial correlation as depicted in Tables 2 and 3. The cases with the same diagnosis and grade on cytology and histopathology were considered as complete correlation. The cases where intraoperative cytological diagnosis did not correlate with the histological examination were categorized as discrepant cases. Deviations of grade of tumor with lesser grade on squash smear cytology were included in partially correlated cases.
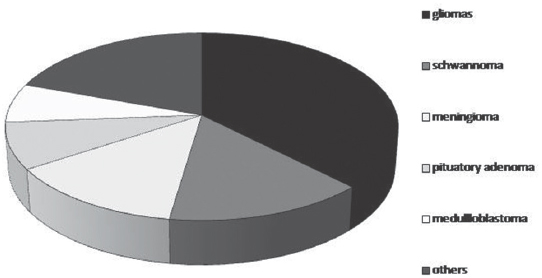
- Pie chart - incidence of central nervous system tumors in our series
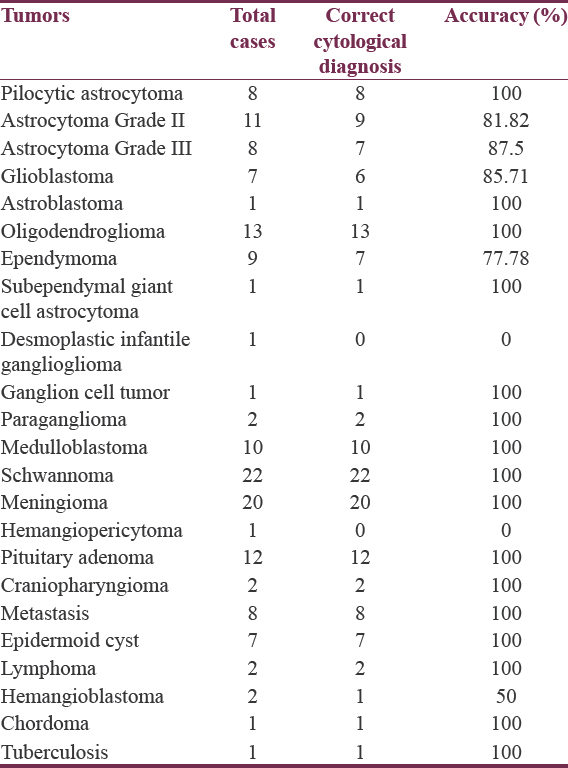

In our series, astrocytomas (incidence = 23.34%) were the most common tumors, followed by schwannoma (14.67%), meningioma (13.33%), oligodendroglioma (8.67%), and pituitary adenoma (8%). Metastatic lesions were diagnosed in eight patients on squash smear which included metastasis from the breast, lung, and kidney. The representative microphotographs are shown in [Figures 2–4].
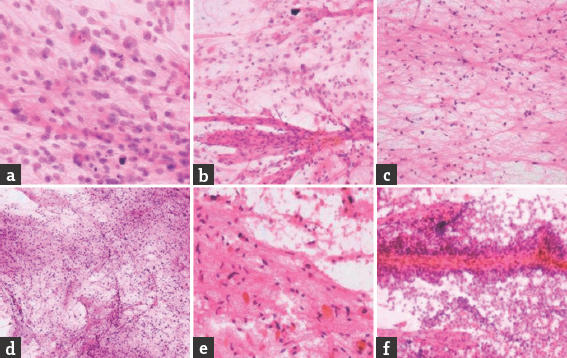
- (a) High-grade astrocytoma: sheets of cells having large irregular pleomorphic nuclei; mitotic figure ares seen; (H and E, ×400). (b) Glioblastoma: thick-walled blood vessels; (H and E, ×400). (c) Low-grade astrocytoma – increase in cellularity with mild nuclear pleomorphism; (H and E, ×400). (d) Pilocytic astrocytoma with loose and cellular area; (H and E, ×100). (e) Pilocytic astrocytoma demonstrating Eosinophilic granular bodies; (H and E, ×400). (f) Ependymoma: cells are arranged in small papillae around blood vessel. More loosely adherent cells are smeared away from vessels; (H and E, ×400)
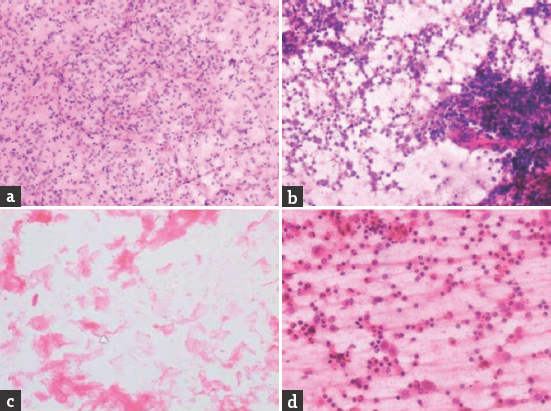
- (a) Oligodendroglioma showing finely branching capillary network; (H and E, ×400). (b) Cellular smears of lymphoma showing isolated large round cells with scanty cytoplasm. Nucleoli are prominent; (H and E, ×400). (c) Epidermoid cyst showing flakes of keratinous material; (H and E, ×400). (d) Smears showing inflammatory cell infiltrate and macrophages; (H and E, ×400)
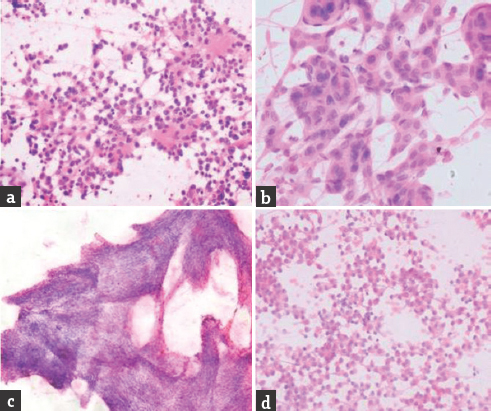
- (a) Medulloblastoma showing neoplastic cells in sheets and rosettes are present; (H and E, ×400). (b) Meningioma showing whorled pattern of meningothelial cells; (H and E, ×400). (c) Schwannoma showing interlacing fascicles of smeared Antoni A tissue consisting of tightly packed, elongated spindle-shaped tumor cells; (H and E, ×100). (d) Pituitary adenoma showing sheets of round cells having moderate amount of cytoplasm and at places arranged in the glandular pattern; (H and E, ×400)
DISCUSSION
The intraoperative diagnosis of CNS tumors by smearing the tissue can provide guidance in modifying the surgical approach by the neurosurgeons. The exact location, radiological findings, and clinical presentation of the patient help the pathologist in making the cytological diagnosis with reasonable accuracy. Accuracy of cytological diagnosis depends on the good cytological preparation and staining of the smear. Smearing of the tissue with ease depends on the consistency of the tumor. The soft and friable tissues in the CNS tumors are easy to smear and thus provide good cellular details. This is especially exhibited in gliomas, medulloblastomas, pituitary adenomas, most of the meningiomas, and metastatic tumors. Many tumors such as nerve sheath tumors, epidermoid cysts, and some meningiomas, especially the fibroblastic type, are relatively tough to smear.
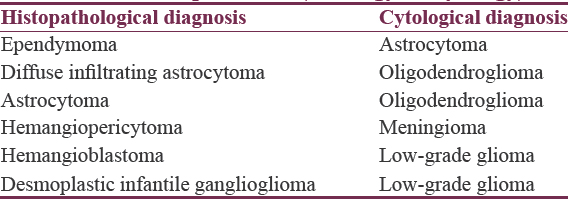
Although smears provide good cytological details, a few diagnostic difficulties were encountered due to misrepresentation of the tumor tissue. There were seven discrepant cases in our study. Tissue from unrepresentative areas led to erroneous diagnosis in discrepant cases. Two astrocytomas were misinterpreted as oligodendroglioma due to the presence of cortical tissue in the smears. The absence of any rosette pattern with diffuse fibrillary background led to misinterpretation of two cases of ependymoma as astrocytoma. In these cases of ependymoma, discussion with the operating surgeon could have helped in knowing the plane of cleavage of the tumor and thereby keeping ependymoma as a differential diagnosis, thereby eliminating the error.
Hemangiopericytoma was misinterpreted as fibroblastic meningioma although no whorling pattern was identified. Our little experience with the hemangiopericytoma led to error. In case of hemangioblastoma, representative tissue was not submitted and gliotic tissue was misinterpreted as pilocytic astrocytoma. In cases when the tissue is not representative or the cytology findings are not consistent with the radiology, at times, we can ask for more tissue to be submitted intraoperatively which would reduce the discrepancy.
Desmoplastic infantile ganglioglioma was reported as low-grade glioma due to absence of ganglion cells in the tissue submitted.
In the present study, there were two partially correlated cases which varied in the grade on cytology and histopathology. They were under graded on squash smear cytology. The grade of astrocytomas varies within a single tumor, and hence, grading of astrocytoma on cytology occasionally poses problem. One case of glioblastoma was under graded as anaplastic astrocytoma due to the absence of necrosis and no thick-walled vessels could be appreciated. Another case of anaplastic astrocytoma was misgraded as low-grade astrocytoma due to only occasional mitoses in the smear sampled.
In our study, the overall diagnostic accuracy was found to be 94.0%. The overall diagnostic accuracy studied by various authors varied from 76% to 96%.[2345678910111213141516]
CONCLUSION
Cytology provides good cellular details in easily smearable tumors. It permits reliable intraoperative guidance. With clinicoradiological correlation, squash smear cytology could be the preferred method for intraoperative diagnosis of CNS tumors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- National Cancer Institute. SEER Stat Fact Sheets: Brain and other Nervous System Cancers. Available from: https://seer.cancer.gov/statfacts/html/brain.html
- [Google Scholar]
- High diagnostic accuracy of cytologic smears of central nervous system tumors. A 15-year experience based on 4,172 patients. Acta Cytol. 2002;46:667-74.
- [Google Scholar]
- Cytopathology of the central nervous system. Part I. Utility of crush smear cytology in intraoperative diagnosis of central nervous system lesions. Acta Cytol. 2006;50:608-16.
- [Google Scholar]
- Utility of intra-operative consultations for the diagnosis of central nervous system lesions. Ann Clin Lab Sci. 2001;31:133-9.
- [Google Scholar]
- Intraoperative cytologic diagnosis of lesions of the central nervous system. Am J Clin Pathol. 1997;108(4 Suppl 1):S56-66.
- [Google Scholar]
- Accuracy of cytological diagnosis of central nervous system tumours in crush preparation. Indian J Pathol Microbiol. 2006;49:483-6.
- [Google Scholar]
- Crush preparations of lesions of the central nervous system. A useful adjunct to the frozen section. Acta Cytol. 1985;29:279-85.
- [Google Scholar]
- Smear technique for intraoperative examination of nervous system lesions. Acta Cytol. 1993;37:34-9.
- [Google Scholar]
- Intraoperative consultation, cytologic preparations, and frozen section in the central nervous system. Arch Pathol Lab Med. 2005;129:1635-52.
- [Google Scholar]
- Use of cytologic preparations for the intraoperative diagnosis of stereotactically obtained brain biopsies: A 19 year experience and survey of neuropathologists. J Neurosurg. 1999;91:454-8.
- [Google Scholar]
- Smears and frozen sections in the intraoperative diagnosis of central nervous system lesions. Neurosurg Clin N Am. 1994;5:1-18.
- [Google Scholar]
- Cytologic results of fine-needle aspiration biopsies of the central nervous system. Cancer. 1986;58:1117-21.
- [Google Scholar]
- Intraoperative consultation and smear cytology in the diagnosis of brain tumours. Kathmandu Univ Med J (KUMJ). 2008;6:453-7.
- [Google Scholar]
- Intraoperative squash cytology of central nervous system lesions: A single center study of 326 cases. Diagn Cytopathol. 2010;40:104-12.
- [Google Scholar]
- Accuracy and diagnostic yield of intraoperative squash smear technique in rapid diagnosis of CNS lesions. Bombay Hosp J. 2010;52:153-60.
- [Google Scholar]
- Role of squash smear technique in intraoperative diagnosis of CNS tumours. Int J Med Sci Public Health. 2013;4:889-92.
- [Google Scholar]






