Translate this page into:
Holocord syringomyelia presenting as rapidly progressive foot drop
Address for correspondence: Dr. K. Saifudheen, Department of Neurology, Medical College Calicut, Calicut-8, Kerala, India. E-mail: drsaifu@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
A 14-year-old girl presented with rapidly progressive bilateral foot drop of 1-week duration with no sensory, bowel or bladder symptoms. Examination showed weak dorsiflexion of the feet, mild wasting of the left hand, dissociated sensory loss over left C4 to T8 dermatomes, diminished stretch reflexes and extensor plantar response. Nerve conduction studies showed low-amplitude compound motor action potential and normal latency and velocity for both peroneal and left ulnar nerves. The F wave was normal. Sensory nerve action potentials for median, ulnar and sural nerves were normal. Electromyographic examinations showed chronic neurogenic changes in first dorsal interossei, tibilalis anterior and medial gastrocnemius muscles on both sides. MRI revealed a Chiari I malformation with syrinx occupying almost the entire spinal cord from C2 to the conus medullaris (holocord syrinx) [Figures 1 and 2]. The patient declined any surgical intervention.
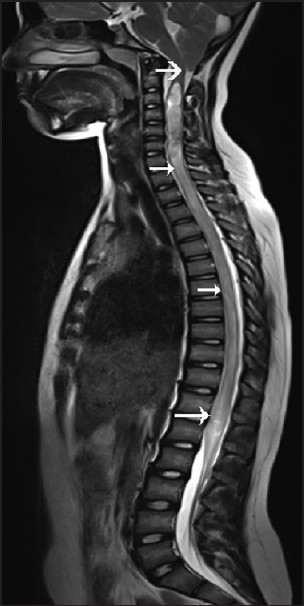
- Sagittal T2W MRI of the cervical spine shows a Chiari I malformation (thick white arrow) with syrinx extending along the entire spinal cord from C2 to the conus medullaris (white arrow)
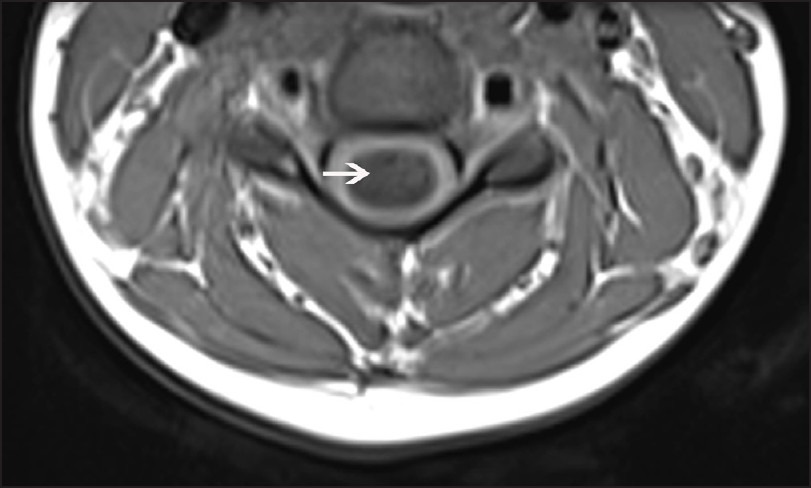
- Axial T1W MRI of cervical spine shows syrinx (white arrow)
Foot drop is a common problem that a patient can present in outpatient department. Although the most frequent cause is a common peroneal neuropathy at the neck of the fibula, other causes include anterior horn cell disease, lumbar plexopathies, L5 radiculopathy, partial sciatic neuropathy and rarely parasagital lesion. In our case, isolated foot dorsiflexion weakness without any sensory finding localize to anterior horn cell, ventral root or motor nerve involvement. In our case, it is reasonable to assume that foot drop is due to the anterior horn cell dysfunction, as shown by the imaging and electrophysiology.
Syringomyelia has variable clinical presentations which include asymmetric weakness and atrophy of hands, upper and lower limb spasticity, areflexia of upper extremity, dissociated sensory loss in the neck and arms (classic cape like distribution) and increased tone and hyperreflexia of lower limb.[1] This is the first reported case of rapidly progressive bilateral foot drop as the presenting symptom of syringomyelia and Chiari I malformation without cord tethering.
Source of Support: Nil.
Conflict of Interest: None declared.
Reference
- Syringomyelia presenting as rapidly progressive foot drop. J Clin Neuromuscul Dis. 2002;3:133-4.
- [Google Scholar]





