Translate this page into:
Headache Patterns in Cerebral Venous Sinus Thrombosis
Address for correspondence: Dr. Ravi Yadav, Department of Neurology, National Institute of Mental Health and Neurosciences, Bengaluru - 560 029, Karnataka, India. E-mail: docravi20@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
The objective of this study was to assess the clinical characteristics, patterns, and factors associated with headache in patients with cerebral venous sinus thrombosis (CVT).
Methods:
In this prospective cohort study, we recruited conscious CVT patients who were able to give reliable history after consent. Institutional ethics approval was obtained. The diagnosis of CVT was based on the clinical and imaging parameters. Data regarding headache characteristic, severity (visual analog scale [VAS]), imaging findings and outcome was recorded.
Results:
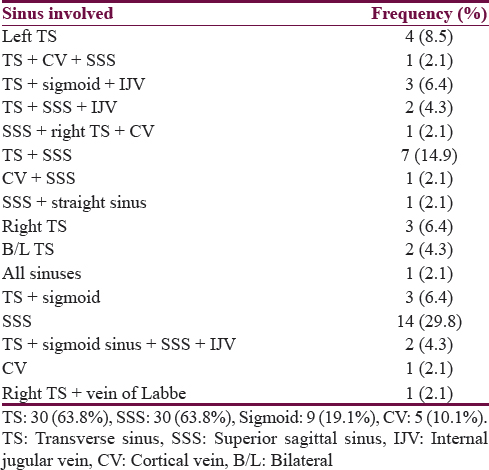
Forty-seven patients (19 males and 28 females) with mean age 29.7 ± 8.7 years were recruited. The mean duration of headache was 12.6 ± 26.8 days, and VAS was 79.38 ± 13.41. Headache onset was acute in 51.1%, subacute in 42.6%, thunderclap in 4.3%, and chronic in 2.1%; location was holocranial in 36.2%, frontal in 27.7% patients; description was throbbing in 44.7% and aching in 25.5% patients. Superior sagittal sinus and transverse sinus were involved in 63.8% cases each. The prothrombotic factors were anemia in 55.3%, puerperal in 38.3%, hyperhomocysteinemia in 29.8%, and polycythemia in 19.1%.
Conclusion:
Holocranial and bifrontal headache of increasing severity may be a marker of CVT. This may be useful in clinical judgment in identifying conscious patients with CVT.
Keywords
Acute
headache
holocranial
thrombosis
venous
INTRODUCTION
Cerebral venous sinus thrombosis (CVT) is a form of stroke resulting from the thrombosis of the venous sinuses of the brain with protean clinical presentations. In more than 85% of the CVT patients, headache is the presenting clinical symptom.[1] The most common presenting symptom in CVT is a headache which is frequently associated with other symptoms and signs, namely seizures, focal neurological deficits, papilledema, and impaired consciousness.[23] The type of headaches that have been reported in CVT range from cluster headache such as onset, worst headache of life, migraine-like headache, exploding headache, chronic tension headache, chronic daily headache, and thunderclap headache.[45] In CVT, the pattern of headache is not uniform and is highly variable.[36] Most common pattern is subacute onset that with rapid worsening and variable severity. The headache in CVT can mimic subarachnoid hemorrhage, migraine, and idiopathic intracranial hypertension.[789] Difficulty to select patients for neuroimaging may occur due to lack of definite clinical criteria for the diagnosis of CVT and increased prevalence of primary headaches such as migraine, tension-type, and chronic daily headache.
Clinical characterization based on study of patients with acute and chronic CVT can help to develop a set of features that could be used for clinical evaluation and investigation of patients. Studies that have looked into the type of headache in CVT are few.[101112] Most of the literature that was available was in the form of case reports which describe the unusual presentation of CVT with various types of headaches. The main aim of the current study was to characterize the type of headache in CVT, pattern of venous sinus involved, factors affecting headache, and response to standard therapeutic interventions.
METHODS
This was a prospective descriptive observational study on a cohort of CVT patients who were recruited after informed consent and consecutively from the emergency and outpatient department of department of neurology at a tertiary care center in south India. We recruited the CVT patients between August 2010 and April 2014. The study was approved by Institute Ethics Committee.
Inclusion criteria
Patients of CVT who were present in neurology casualty or were admitted to Neurology wards and those who were conscious, cooperative, and were able to give a reliable history.
The diagnosis of CVT was based on clinical presentation and confirmation by imaging (computed tomography [CT] with CT venogram/magnetic resonance [MR] brain with MR venography)
Anemia was considered mild when hemoglobin levels are 11–11.9 g/dl in women and 11.0–12.9 g/dl in men; moderate when hemoglobin levels are 8–10.9 g/dl (both men and women); and severe when hemoglobin levels are lower than 8 g/dl.
Exclusion criteria
The patients with the following features: (1) arterial stroke, (2) unconscious or uncooperative patient who was unable to provide a reliable history, (3) head trauma, (4) neuro infection, (5) nonavailability of reliable history (at the time of recruitment if the history is given by a person/relative who was not with the patient at the onset of symptoms and may provide inaccurate history), and (6) patients in whom the diagnosis was not confirmed by imaging studies (CT with CT venogram or magnetic resonance imaging brain with MR venogram).
The patients were interviewed by investigators in the preformed format, and details of history with particular reference to headache and CVT were recorded. Details of headache included mode of onset, location, severity, pattern, and evolution, associated symptoms, aggravating factors, relieving factors, and other comorbidities. A visual analog scale (VAS) was used to record pain severity (severe headache = VAS >70).[13] Headache severity was assessed by visual analog scale where numerical pain rating scale 0–100 was used. The absence of pain was given a score of 0 and worst pain was given a score of 100 in numerical pain rating score. The headache severity was recorded at the time of recruitment and at the time of discharge. Three modes of onset of headache were defined depending on the time between the initial pain sensation and the most severe headache.
Sudden/thunderclap like was the headache that began with catastrophic sudden onset with a VAS more than (80/100) reaching maximum intensity in <1 min, and lasting more than 1 h. Acute headache was defined by the duration from onset of <24 h. Subacute was defined as duration of more than 24 h and <14 days. Chronic headache was defined by duration of more than 14 days
The patients were treated with anticoagulation in the form of unfractionated heparin 5000–10,000 units intravenous (IV) initially, followed by 50–70 units/kg (5000–10,000 units) q4–q6 h for 10–14 days followed by oral anticoagulation. The patients were given standard antiepileptics for seizures (phenytoin; valproate; levetiracetam), antiedema measures (mannitol - 1.5–2 g/kg IV infused over 30–60 min; oral glycerol; acetazolamide), and general nursing care as per the decision of the treating physician. The patients were given inpatient care in ward or intensive care unit depending on the clinical condition. In case of worsening due to raised intracranial pressure (ICP) and midline shift, the patients were taken up for decompressive craniectomy.
The outcome was measured in terms of VAS, Barthel's index and modified Rankin Scale (mRS). The degree of independence in activities of daily living was assessed by Barthel's index. The degree of disability was assessed by mRS. Barthel's index and mRS were assessed both at admission and at discharge.
Statistical analysis
The data were collected systematically and analyzed by SPSS Version 16 (IBM SPSS, IBM Corporation Armonk, New York, USA) software using descriptive statistics, t-tests, Pearson's correlation for parametric data and Spearman's correlation for nonparametric data. We had calculated two-tailed P value and our significant cutoff value was set at 95% confidence interval and P ≤ 0.05.
RESULTS
A total of 135 patients were screened of which 73 were females and 62 were males. Of which 128 patients were eligible CVT patients (70 males and 58 females). Excluded patients were 81 (42 females and 39 males). The mean age of the excluded patients was 33.8 ± 13.6 years. Forty-seven patients who satisfied the inclusion criteria were included after screening of 128 eligible patients [Figure 1]. A total of 47 patients were recruited in the study of which 32 (68.1%) were females. The mean age of the study group was 29.7 ± 8.7 years (men 33.47 ± 8.3 years; women 28.06 ± 8.6 years) [Table 1]. The clinical characteristics of headache are shown in Table 2. The pattern of sinus involvement is shown in Table 3.
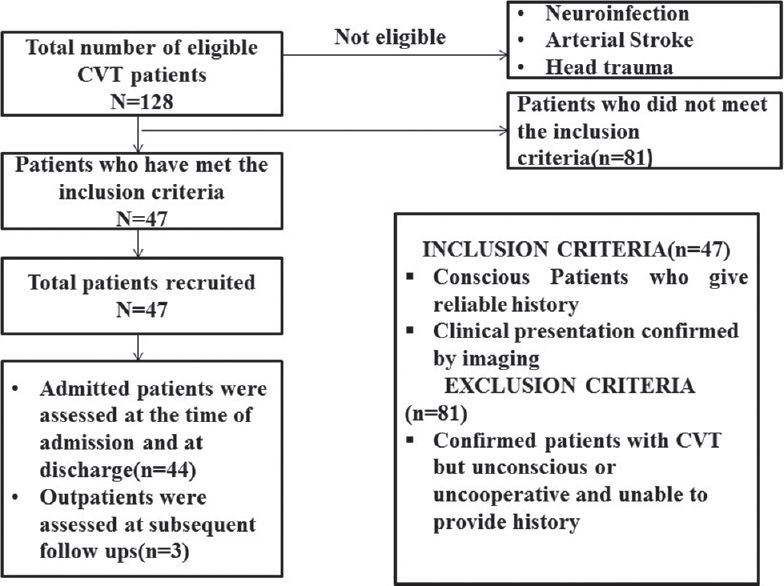
- Schema of recruitment of patients with headache and cerebral venous sinus thrombosis
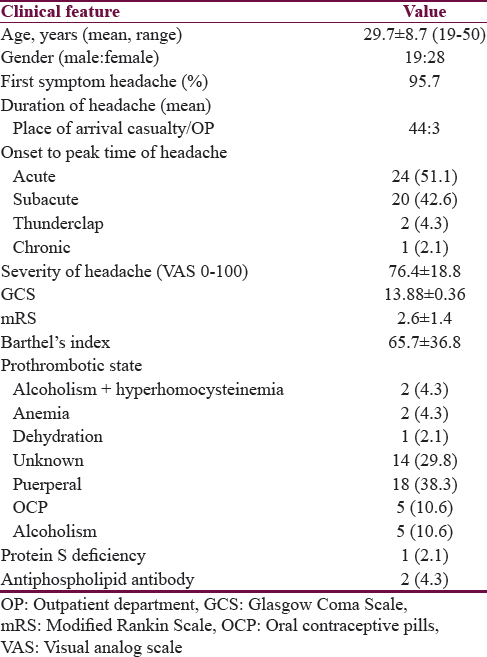
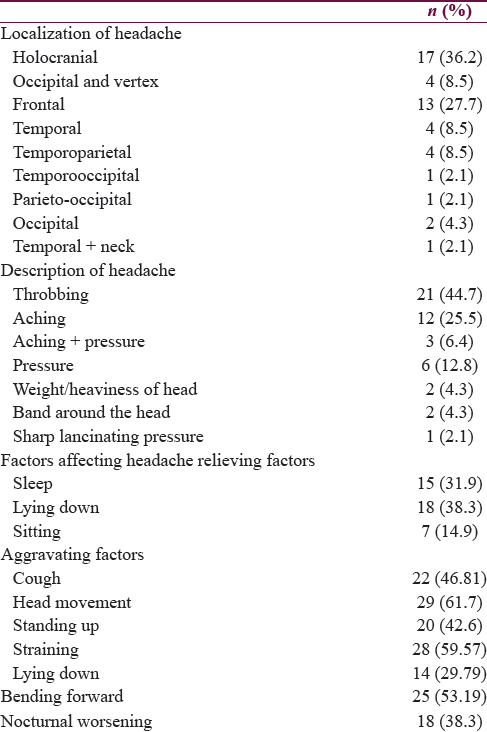
Holocranial headache was the most common type of headache in our cohort seen in 17 (36.2%) patients. The most common description of headache was throbbing type in 21 (44.6%) and aching type in 12 (25.5%) patients [Table 2].
Migraine like headache was present in 12 (25.5%) and tension-type like headache was seen in 4 (8.5%) patients. Seizures were seen in 22 (46.8%) subjects out of which focal with secondary generalization were seen in 10 (21.3%) generalized seizures in 9 (19.1%) and focal seizures in 3 (6.4%) subjects. Papilledema was found in 28 (59.6%) subjects. Focal neurological deficits (diplopia, anomia, language disturbances) were present in 18 (38.3%) patients.
The mean duration of hospital stay was 17.28 ± 14.15 days. In our study, the duration of hospitalization correlated to Glasgow Coma Scale (GCS) scores at admission (P = 0.02). Duration of the hospital stay did not have any association with severity of headache (P = 0.47), Barthel's index (P = 0.88), and mRS (P = 0.99) at admission.
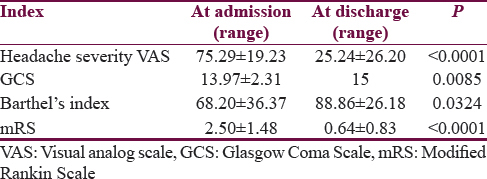
Headache severity at admission by VAS was 79.38 ± 13.41. Headache severity by faces pain rating scale at admission was 3.96 ± 0.81. The mean pain score following mannitol was 40.77 ± 22.05 following analgesic treatment was 38.97 ± 29.56. There was a significant improvement (P < 0.0001) in headache severity following mannitol and analgesic administration. There was a significant improvement in GCS (P = 0.002), Barthel's index (P < 0.0001), and mRS (P < 0.0001) at discharge [Table 4].
DISCUSSION
In this study, we studied the clinical characteristics of headache in south Indian patients with CVT. A headache characteristics were studied in detail, and we attempted to identify the discriminating features.
Mode of presentation
Acute headache was the most common presentation in our series followed by subacute type. The acute presentation was also the most common type in International Study on Cerebral Vein Thrombosis (ISCVT) study although in the series by Damak et al. study the mode of onset was predominantly subacute (72%). Another study reported similar findings as our series.[14] One reason for these differences could be the criteria used to define the acute, subacute and chronic type of a headache during recruitment in these studies. The criteria used by Damak et al. was acute <2 days, subacute 2 days to 1 month and chronic was more than 1 month.[15] Wasay et al. used 1–3 days as acute, 4–14 days as subacute and more than 14 days as chronic. A study by Cumurciuc et al. defined only acute and thunderclap headache in their series of 17 cases and found headache of progressive type as the most common type (>24 h).
We found the first symptom as headache in 95% of the patients. However, the patient presenting only with headache were 6.38%, and the most common sinus involved was transversal sinus (TS) and superior sagittal sinus (SSS) in our cohort. We could not demonstrate laterality of headache in our cohort due to coexisting involvement of other sinuses. The commonest type of headache observed in our study was holocranial or bifrontal probably due to this reason. In our cohort, 11 (23.4%) patients had headache as the sole presentation. A French study on 123 patients of CVT, found that headache was the only clinical symptom at presentation in 23% (17) of the patients. The lateral sinus was the most common sinus that was involved in these patients. Once established a headache was continuous in 15 patients and was usually ipsilateral to the occluded sinus.[11] Sparaco et al. reported headache as a sole manifestation of CVT in nearly one-third of the patients.[16] Timóteo et al. reported headache as the only presenting symptom in 40% of their patients.[17] Wasay et al. found no association between localization of headache and site of sinus thrombosis, however, they found association between the involvement of sigmoid sinus alone or in combination with transverse sinus and localization of pain to occipital area and neck. Other studies have not published any such association.[17]
In our study, prothrombotic state was seen in 68.1% cases. 5 (10.6%) cases had mild anemia, 13 (27.7%) had moderate anemia, 8 (17%) had severe anemia, and 9 (19.1%) had polycythemia.[18] The mean hemoglobin level was 11.52 ± 3.54 g/dl. Phlebotomy was opted for these patients with polycythemia. Previous studies had mentioned anemia and polycythemia as a risk factor for CVT.[19202122] Secondary causes of anemia and polycythemia were evaluated. One patient with polycythemia had dehydration. One patient with anemia had rheumatoid arthritis. There were no underlying malignancies in any of these patients. None of the cases were detected to be myeloproliferative neoplasms in hospital. The other causes of thrombotic states were puerperal in 40.4%, and oral contraceptive pill (OCP) pill usage in 10.6% in women. In ISCVT study, the most common prothrombotic state was OCP's in 54.3%, genetic in 22%, acquired in 15.7%, and puerperal in 13.8%.[1] In the series by Damak et al. the most common prothrombotic causes were OCP's and other etiologies.[15] Martinelli et al. have reported a strong association between OCP's usage and risk of CVT.[23] OCPs cause a decrease in protein S levels and hypercoagulability.[24]
Headache characteristics
In our study, holocranial headache was the predominant type of headache followed by frontal and most of the patients presented with bilateral headache [Table 2]. Although one previous study has reported unilateral headache as the most common type which was either localized to frontal, temporal, occipital and neck. They reported unilateral headache in 37%, localized headache (frontal, temporal, occipital, and neck) in 19% and diffuse in 20% of the patients. They also found the quality of headache as band like in 27 (20%), other (pounding, exploding, stabbing, etc.) types in 26 (20%), throbbing in 12 (9%), and thunderclap in 7 (5%). Another study also has reported headache as the most frequent symptom of CVT.[25]
In the series by Cumurciuc et al. (n = 17) throbbing headache was seen in 13 (76%) and severe in 13 (76%) of the patients (VAS ≥7). It was diffuse in 4, unilateral in 13 and associated with ipsilateral neck pain in three patients. This study also found association between the laterality of headache and the side of sinus involved.[11] We found that throbbing type of pain was the most commonly described pain in our cohort followed by aching type and pressure type.
In our study, headache mimicking migraine was present in 12 (25.5%) patients, although history of migraine was present in one of them. Tension-type headache was present in 4 (8.5%) patients In Cumurciuc et al. series four patients had a history of migraine before CVT, but they reported change in nature of headache at the time of presentation. One of their patients had headache similar to migraine.[11] This character of headache has been reported before in case reports and small studies.[8] The causative mechanism in patients with migraine like headache could be aseptic inflammatory changes in the region of trigeminal nerve innervation leading to dilatation of vessels and mimicking the migraine etiology.
The unilateral headache found in other studies ipsilateral to the sinus involved could be due to the stretching of dura which is innervated by branches of trigeminal nerve and thus is referred over the same side. On the contrary, when multiple sinuses are involved, the predominant feature is raised ICP thus leading to diffuse stretching of dura and thus resulting in holocranial headache. Similar pathogenesis is seen in cases of SSS thrombosis where the midline location of the sinus gives rise to poor localization and holocranial headache. The inability to find direct correlation between the site of sinus thrombosis and lateralization of headache was due to multiple sinus involvement in most of the patients.
In our study, there was a significant improvement in headache severity, GCS scores, Barthel's index and mRS at the time discharge after standard treatment. In Damak et al. study, death was seen in 1%, 9% were dependent with mRS scores of 3–5 at discharge, 17.4% showed partial recovery and 73% showed complete recovery. The low mortality of CVT in our group points toward the selection bias as only stable patients were recruited. This is at par with declining trends of mortality in CVT patients over time due to improvement in diagnostic and treatment modalities.[26]
The strengths of the study are prospective design, detailed characterization of headache, strict recruitment criteria of conscious patients for a description of headache and confirmation by imaging. This study further adds to the information about the headache patterns commonly seen in patients with CVT as a whole.
The weakness of the study was small sample size and cases with significant multiple venous sinus involvement. There was also probable selection and referral bias as the study was done at a tertiary neurocarecenter. Only conscious CVT patients were included as per the design of the study. Therefore, the results can only be generalized to conscious patients with CVT and not all patients with CVT.
CONCLUSION
In our study, most common headache location was holocranial followed by bifrontal. The most common headache character being throbbing and the most common sinus involved is SSS and TS. Furthermore, isolated TS thrombosis is less common and usually it co-exists with other sinus thrombosis. This pattern shows raised ICP as the primary etiology of generation of headache. Further studies with pure sinus thrombosis of internal jugular vein and SSS will help to support our observations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Prognosis of cerebral vein and dural sinus thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) Stroke. 2004;35:664-70.
- [Google Scholar]
- Headache and cerebral vein and sinus thrombosis. Front Neurol Neurosci. 2008;23:89-95.
- [Google Scholar]
- Thunderclap headache as first symptom of cerebral venous sinus thrombosis. CVST Study Group. Lancet. 1996;348:1623-5.
- [Google Scholar]
- Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients. For The Cerebral Venous Sinus Thrombosis Study Group. J Neurol Neurosurg Psychiatry. 2001;70:105-8.
- [Google Scholar]
- Subarachnoid hemorrhage: A rare presentation of cerebral venous thrombosis. Headache. 2001;41:889-92.
- [Google Scholar]
- Migraine-like headache as the presenting symptom of cerebral venous sinus thrombosis. J Neurol. 2002;249:775-6.
- [Google Scholar]
- Isolated intracranial hypertension as the only sign of cerebral venous thrombosis. Neurology. 1999;53:1537-42.
- [Google Scholar]
- Incidence and pattern of headache in cerebral venous thrombosis. J Pak Med Assoc. 2006;56:561-4.
- [Google Scholar]
- Headache as the only neurological sign of cerebral venous thrombosis: A series of 17 cases. J Neurol Neurosurg Psychiatry. 2005;76:1084-7.
- [Google Scholar]
- Clinical characteristics of cerebral venous thrombosis in a single center in Korea. J Korean Neurosurg Soc. 2014;56:289-94.
- [Google Scholar]
- Cerebral venous thrombosis associated with iron deficiency anemia. J Stroke Cerebrovasc Dis. 2008;17:426-8.
- [Google Scholar]
- Headache in cerebral venous thrombosis: Incidence, pattern and location in 200 consecutive patients. J Headache Pain. 2010;11:137-9.
- [Google Scholar]
- Isolated lateral sinus thrombosis: A series of 62 patients. Stroke. 2009;40:476-81.
- [Google Scholar]
- Headache as the sole presentation of cerebral venous thrombosis: A prospective study. J Headache Pain. 2012;13:487-90.
- [Google Scholar]
- Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. World Health Organization. Available from: http://www.who.int/vmnis/indicators/haemoglobin/en/
- Association between anemia and cerebral venous thrombosis: Case-control study. Stroke. 2015;46:2735-40.
- [Google Scholar]
- Anemia as a risk factor for cerebral venous thrombosis? An old hypothesis revisited. Results of a prospective study. J Neurol. 2007;254:29-34.
- [Google Scholar]
- A case report of cerebral venous thrombosis in polycythemia vera presenting with intracranial and spinal subdural hematoma. Case Rep Neurol. 2010;2:37-45.
- [Google Scholar]
- Cerebral venous thrombosis and venous infarction: Case report of a rare initial presentation of smoker's polycythemia. Case Rep Neurol. 2010;2:150-6.
- [Google Scholar]
- High risk of cerebral-vein thrombosis in carriers of a prothrombin-gene mutation and in users of oral contraceptives. N Engl J Med. 1998;338:1793-7.
- [Google Scholar]
- Transverse sinus thrombosis: An unusual cause of headache. Headache. 1997;37:457-9.
- [Google Scholar]
- Does headache represent a clinical marker in early diagnosis of cerebral venous thrombosis? A prospective multicentric study. Neurol Sci. 2004;25(Suppl 3):S298-9.
- [Google Scholar]
- Declining mortality in cerebral venous thrombosis: A systematic review. Stroke. 2014;45:1338-41.
- [Google Scholar]






