Translate this page into:
Crescent-shaped intracranial hemorrhage in cerebral venous sinus thrombosis: A case report and review of literature
*Corresponding author: Muhammad Yunus Amran, Division of Interventional Neurology and Neuroendovascular Therapy, Department of Neurology, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia. muhyunusamran@med.unhas.ac.id, yunusamran10@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Amran MY, Fitrah YA. Crescent-shaped intracranial hemorrhage in cerebral venous sinus thrombosis: A case report and review of literature. J Neurosci Rural Pract. 2025;16:118-24. doi: 10.25259/JNRP_430_2024
Abstract
Cerebral venous sinus thrombosis (CVST) is a rare but serious condition involving blood clots in the cerebral venous system often linked to prothrombotic states. It can result in complications such as intracranial hemorrhage and neurological deficits. We present the case of a 16-year-old female with CVST affecting the superior sagittal sinus, who experienced severe headaches and seizures. Initial computed tomography imaging showed a hematoma in the right frontal lobe, suggesting sinus and cortical vein thrombosis. Magnetic resonance imaging, magnetic resonance angiography, and magnetic resonance venography confirmed subacute hemorrhage with perifocal edema, and cerebral angiography validated the diagnosis. Elevated D-dimer levels supported the findings. The patient was treated with fondaparinux and later transitioned to oral warfarin, leading to clinical improvement and reduced D-dimer levels within a week. This case highlights the importance of early diagnosis and anticoagulation therapy, even in hemorrhagic cases, to prevent long-term complications and emphasizes the need for awareness of CVST in similar scenarios.
Keywords
Cerebral venous sinus thrombosis
Crescent-shaped intracranial hemorrhage
Superior sagittal sinus thrombosis
Cortical veins thrombosis
Anticoagulation therapy
INTRODUCTION
Cerebral venous sinus thrombosis (CVST) is a rare but potentially life-threatening condition characterized by the formation of blood clots in the cerebral veins and sinus. This condition can lead to significant disruption of venous blood flow and increased intracranial pressure (ICP), causing a variety of neurological symptoms.[1,2] CVST can involve different venous sinuses within the brain, with the superior sagittal sinus (SSS) being the most commonly affected. The clinical presentation of CVST is highly variable, making diagnosis challenging and necessitating a high index of suspicion, especially in young patients presenting with unexplained neurological symptoms such as headaches, seizures, or focal neurological deficits. Given its rarity and diverse presentation, CVST requires prompt recognition and treatment to prevent long-term complications or mortality.[1,3] This case report discusses a 16-year-old female who presented with acute neurological symptoms secondary to CVST, highlighting the diagnostic approach, management, and outcomes in this rare but serious condition.
CASE REPORT
A 16-year-old female had been referred to our hospital after experiencing a 12-day history of persistent headaches. The headache had been described as intense, stabbing, and sharp, occasionally spreading from the eyes to the back of the head, and had been accompanied by dizziness. Eleven days before admission, the patient had suffered a generalized tonic-clonic seizure lasting approximately 2 min, followed by unconsciousness. During this period, she had experienced ten episodes of generalized seizures, each lasting several minutes. After the seizures had subsided, she had felt lethargic and fallen asleep. Upon regaining consciousness, she had exhibited motor aphasia, which was characterized by difficulty expressing words despite understanding instructions, as well as numbness and weakness on the right side of her body. She had initially been treated at a local hospital, where she had been diagnosed with status epilepticus and had received phenytoin 100 mg twice daily and piracetam 700 mg three times daily to control the seizures. Although the seizures had been managed effectively, the headache and neurological symptoms had persisted, prompting her referral to our facility for further evaluation. The patient had reported a history of fever two weeks before admission, which had resolved on its own. She had denied any prior use of oral contraceptives or a history of trauma, hypertension, diabetes, cardiovascular disease, or tuberculosis. On initial evaluation, she had been fully conscious (Glasgow Coma Scale E4M6V5) with motor aphasia, moderate right-sided weakness (muscle strength scale 4), and hyperreflexia in the right lower limb. Babinski and other pathological reflexes had been absent. Laboratory investigations had revealed elevated D-dimer levels (4.96 ng/mL) and raised liver transaminases: Serum glutamic oxaloacetic transaminase (132 U/L) and serum glutamic pyruvic transaminase (162 U/L), while coagulation studies, including prothrombin time, activated partial thromboplastin time, and international normalized ratio, had been normal.
The axial magnetic resonance imaging images of the brain findings [Figure 1] in this case provided clear evidence of CVST involving the SSS. On the axial T1-weighted (T1W), T2-weighted (T2W), T2-fluid-attenuated inversion recovery (T2-FLAIR), and diffusion-weighted imaging (DWI) sequences [Figure 1a], hyperintense signals were present in both parietal regions, particularly near the midline, indicating areas of venous congestion or ischemia due to impaired venous outflow. These changes were consistent with the involvement of the SSS, one of the brain’s major venous structures. There was also a distinct hyperintense lesion in the right frontal lobe [Figure 1b], likely representing a subacute hemorrhage, which is a common complication of CVST resulting from elevated venous pressure and vessel rupture. Additional bilateral hyperintense signals visible on the FLAIR images further suggested ischemic or congestive changes related to CVST.
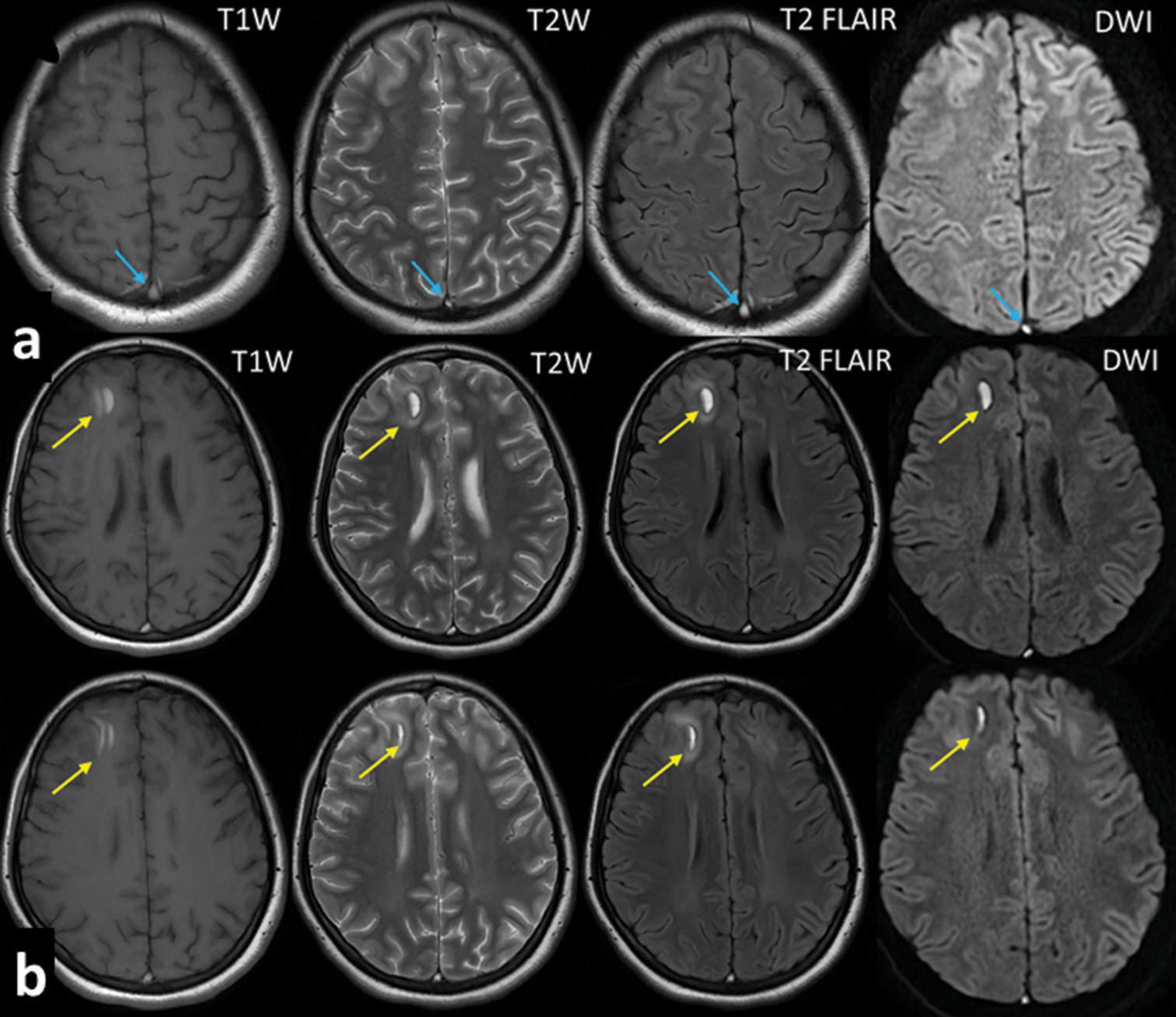
- Axial MRI images of the brain: T1-weighted (T1W), T2-weighted (T2W), T2-FLAIR, and diffusion-weighted imaging (DWI) sequences in a patient with CVST. (a) The axial T1W, T2W, T2-FLAIR, and DWI sequences reveal hyperintense signals in the bilateral parietal regions (blue arrow), indicative of venous ischemia or infarction. These lesions are localized near the midline, suggesting involvement of the superior sagittal sinus, the most common site for CVST. The distribution and pattern of these hyperintensities are consistent with venous congestion or edema, resulting from impaired venous drainage due to thrombosis; (b) The axial T1W, T2W, T2-FLAIR, and DWI images also demonstrate a hyperintense region in the right frontal lobe (yellow arrow), likely representing a subacute hemorrhagic lesion secondary to CVST, characterized by crescent-shaped intracranial hemorrhage. In addition, the presence of bilateral hyperintense areas on the FLAIR sequence in the parietal regions further supports the diagnosis of venous congestion or ischemic changes, common complications associated with superior sagittal sinus thrombosis. MRI: Magnetic resonance imaging, CVST: Cerebral venous sinus thrombosis, FLAIR: Fluid-attenuated inversion recovery.
The magnetic resonance venography (MRV) and magnetic resonance angiography (MRA) brain sequences [Figure 2] confirmed the diagnosis by showing a lack of normal blood flow in the SSS and cortical veins, indicative of thrombosis. These images together demonstrated the effects on the SSS and cortical veins, including venous obstruction, elevated ICP, and secondary ischemic and hemorrhagic brain injury. The combination of T1W, T2W, T2-FLAIR, DWI, MRV, and MRA imaging provided a comprehensive understanding of the underlying pathology in this patient, underscoring the critical role of advanced imaging techniques in diagnosing and managing CVST.
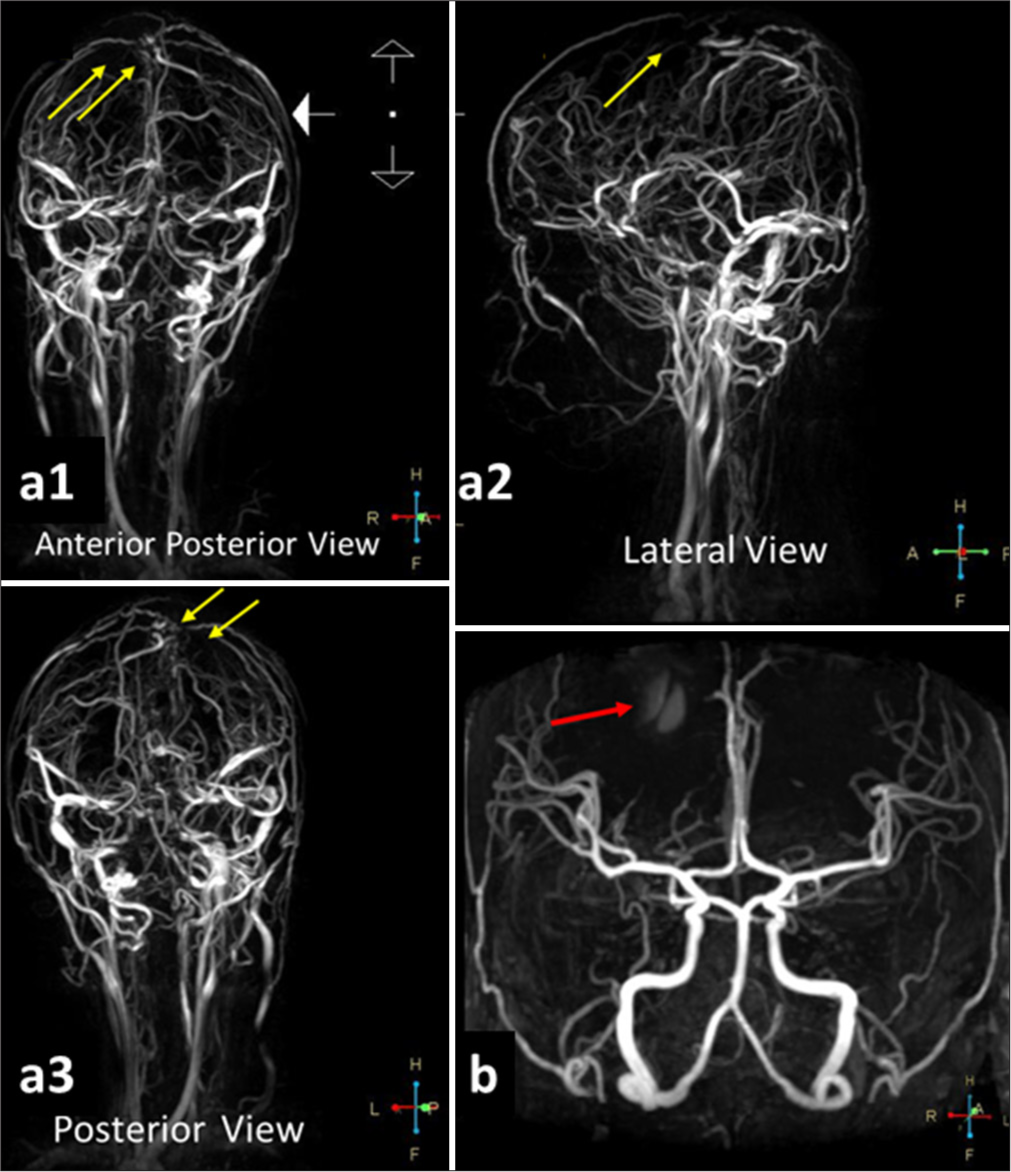
- MRV and MRA brain sequences in a patient with CVST. (a1) The anterior-posterior view of the MRV demonstrates a segmental cutoff or occlusion in the superior sagittal sinus and cortical veins (yellow arrows), confirming the diagnosis of CVST; (a2) The lateral view of the MRV similarly shows a segmental cut-off or occlusion in the superior sagittal sinus and cortical veins (yellow arrow), further supporting the diagnosis of CVST; (a3) The posterior view of the MRV reveals a segmental cut-off or occlusion in the superior sagittal sinus and cortical veins (yellow arrows), confirming the presence of CVST; (b) The anterior cranial view of the MRA indicates contrast leakage (red arrow), confirming the presence of late subacute hemorrhage in the right frontal lobe accompanied by perifocal edema. This phenomenon is attributed to venous occlusion, which disrupts normal blood flow, leading to venous hypertension, edema, and ischemic changes in the affected cortical regions. MRI: Magnetic resonance imaging, CVST: Cerebral venous sinus thrombosis, MRA: Magnetic resonance angiography, MRV: Magnetic resonance venography.
To further assess the patient’s condition, cerebral digital subtraction angiography [Figure 3] was performed, which revealed reduced blood flow to the SSS and bilateral cortical veins, particularly on the right side.
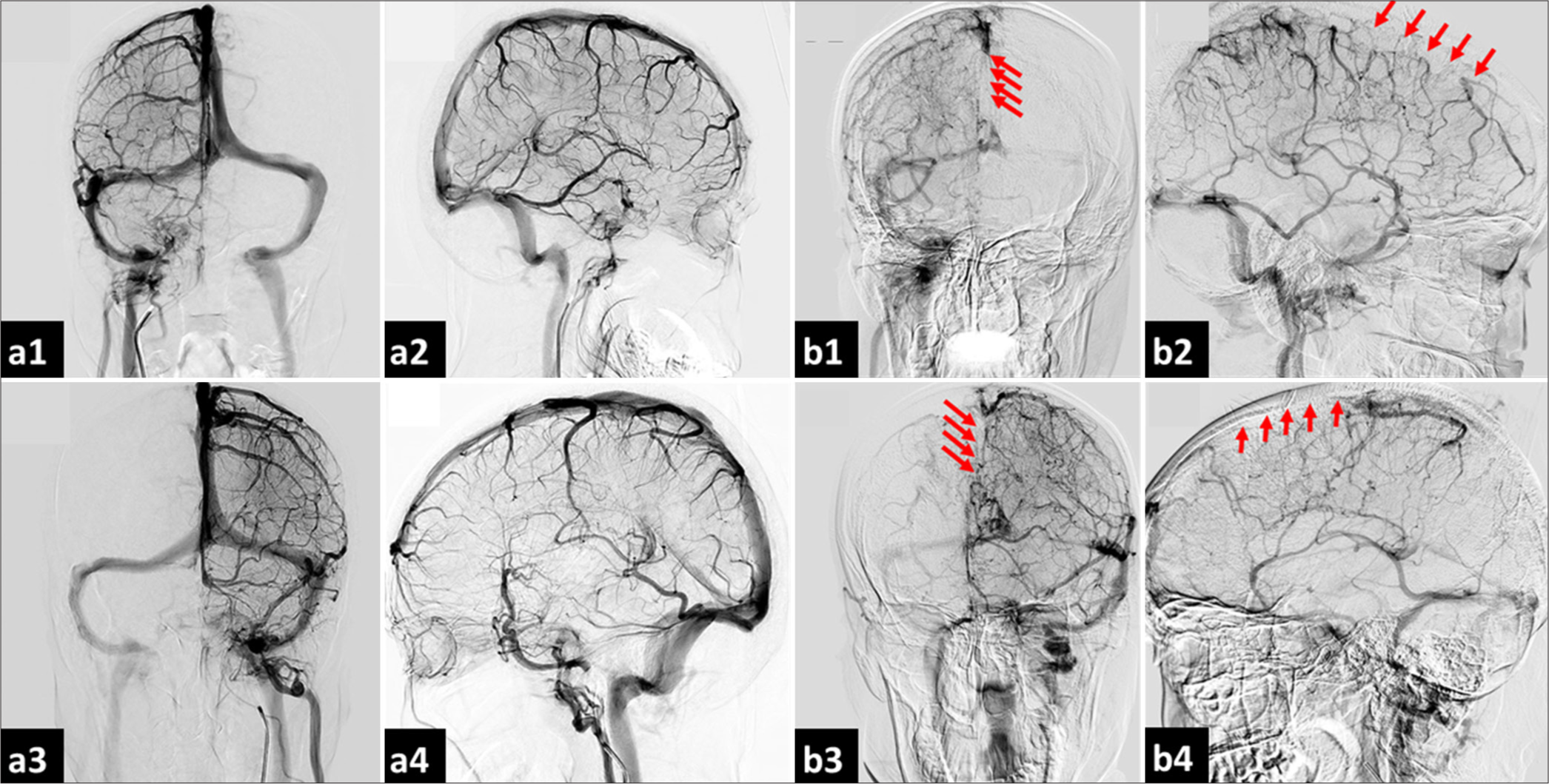
- Cerebral digital subtraction angiography: Venous phase in a patient with CVST. (a1) Contrast injection from the right internal carotid artery (Rt-ICA) in the anterior-posterior view reveals a normal pattern of the cerebral venous sinus; (a2) The lateral view of contrast injection from the Rt-ICA also displays a normal pattern of the cerebral venous sinus; (a3) Contrast injection from the left internal carotid artery (LtICA) in the anterior-posterior view shows a normal pattern of the cerebral venous sinus; (a4) The lateral view of contrast injection from the Lt-ICA similarly demonstrates a normal pattern of the cerebral venous sinus; (b1) Contrast injection from the Rt-ICA in the anterior-posterior view indicates reduced flow to the superior sagittal sinus and bilateral cortical veins, particularly on the right side, raising the suspicion of thrombosis in both the superior sagittal sinus and cortical veins (red arrows); (b2) The lateral view of contrast injection from the Rt-ICA corroborates the finding of reduced flow to the superior sagittal sinus and bilateral cortical veins, especially on the right side, suggesting possible thrombosis (red arrows); (b3) Contrast injection from the Lt-ICA in the anterior-posterior view reveals diminished flow to the superior sagittal sinus and bilateral cortical veins, predominantly on the right side, further indicating potential thrombosis (red arrows); and (b4) The lateral view of contrast injection from the Lt-ICA also shows reduced flow to the superior sagittal sinus and bilateral cortical veins, particularly on the right side, reinforcing the possibility of thrombosis in these regions (red arrows). CVST: Cerebral venous sinus thrombosis.
Based on the clinical, radiological, and angiographic findings, a diagnosis of CVST had been made. Treatment had included a subcutaneous injection of 2.5 mg of fondaparinux (anti-factor Xa) once daily, which was later transitioned to a direct anticoagulant on day 7. Additional supportive care had included analgesia with ketorolac 30 mg intravenously twice daily. The patient’s headache had fully resolved by day 9 of treatment.
DISCUSSION
This case of a 16-year-old female with CVST highlights key clinical features and the complexity of managing the condition. Headache was the initial and dominant symptom, which is consistent with studies reporting that headaches occur in 60–90% of CVST cases. The character of the headache, often throbbing or pressure-like, can progress gradually over days and is typically linked to increased ICP. In this case, the persistence of headaches despite adequate seizure management aligns with findings from studies in Pakistan, India, and Turkey, where headache is frequently reported as the most prevalent symptom among CVST patients. Globally, the incidence of CVST is significantly higher in females, with studies consistently demonstrating a marked predominance among women, particularly those of reproductive age, with an average age commonly reported as between 36 and 39 years. Headache continues to be the most commonly reported clinical manifestation. On a global scale, CVST has an incidence rate of 2.62 cases/100,000 individuals, with hormonal influences such as pregnancy and contraceptive use serving as significant risk factors. These findings strengthen the understanding that headache is the predominant clinical feature of CVST, especially among female patients.[1,3,4] Seizures, a common symptom of CVST, were also observed in this patient. Seizures often arise in patients with supratentorial hemorrhagic lesions or cortical vein thrombosis and are particularly common in the acute phase of CVST. In this case, the patient’s imaging studies showed thrombosis in the SSS and cortical veins, supporting the pathophysiology linking seizures to this anatomical involvement. Early seizure activity is common, with reports showing early seizures in 44.3% of CVST patients and status epilepticus in up to 12.8%. The use of anticonvulsants, such as phenytoin in this case, is crucial for managing recurrent seizures.[1,5] Aphasia, a focal neurological deficit, was another significant finding in this patient, emerging after the CVST diagnosis. Aphasia is often associated with thrombosis in the dominant hemisphere’s cortical veins, particularly in the left lateral sinus, as was the case in this patient. Literature suggests that aphasia occurs in 19–24% of CVST cases, and its presence in this patient further underscores the multifaceted neurological impact of CVST.[1,6]
In addition, intracerebral hemorrhage (ICH) developed in this patient, a complication known to affect 30–40% of CVST cases. ICH in the setting of CVST is associated with a worse prognosis and is linked to increased venous pressure and compromised neurovascular integrity. The rupture of dilated veins due to CVST can result in hemorrhagic transformation, as occurred in this case, where imaging showed a right frontal hematoma. This complication raises concerns for long-term morbidity and mortality.[4,7] Previous studies indicate that D-dimer serves as a sensitive diagnostic tool for excluding CVST in low-risk patients. Notably, a meta-analysis revealed a high negative predictive value for D-dimer levels in patients presenting with isolated headaches suspected of having CVST.[8,9]
In our case, the initial D-dimer level of 4.96 ng/mL, followed by a decrease to 2.78 ng/mL after treatment, underscores the utility of this biomarker not only in confirming the diagnosis but also in monitoring the effectiveness of anticoagulation therapy in a patient without traditional risk factors for CVST. This highlights the importance of D-dimer testing in assessing patients with unexplained headache symptoms, reinforcing its role in clinical decision-making.[10,11]
The management of CVST in this patient followed established guidelines. Anticoagulation therapy is a mainstay of CVST treatment, even in the presence of ICH. In this case, fondaparinux, a factor Xa inhibitor, was administered subcutaneously, followed by oral anticoagulation. According to the European Stroke Organization and American Heart Association/American Stroke Association guidelines, anticoagulation should be continued for 3–6 months in provoked cases and 6–12 months in unprovoked cases. Warfarin was chosen for long-term management in this patient, as direct oral anticoagulants and factor Xa inhibitors are not the first-line choice for CVT according to current guidelines.[1,10,12] Table 1 summarizes several cases of CVST based on their clinical presentations, imaging findings, therapy, and outcomes.
| No | Author (s) | Year | Patient demographics | Clinical presentation | Imaging findings | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| 1. | Sun et al.[13] | 2018 | Female, 57-year-old | Headache, nausea, vomiting, incomplete motor aphasia, right hemihypalgesia, later developed seizures | CT: Linear high-density images in parietal, frontal, occipital lobes; MRA, MRV confirm sagittal sinus thrombosis | Dehydration therapy, no anticoagulants or thrombolytics | Patient improved with mild right-sided weakness and non-fluent aphasia; no recurrence of thrombosis |
| 2. | Katwal et al.[4] | 2024 | Male, 30-year-old | Sudden onset right-sided weakness, 5-day history of severe headache, nausea, vomiting, no prior medical history, reduced muscle strength, right-sided paresthesia, difficulty comprehending language | Non-contrast CT: hypodense lesion in left parietal lobe, hemorrhage, mass effect. MRI venography confirmed thrombosis in superior sagittal sinus, left vein of Trolard, and parietal cortical veins | Low-molecular-weight heparin for 10 days, followed by oral vitamin K antagonists | Clinical improvement, regained motor function, minimal residual symptoms, good recovery with physiotherapy. Declined follow-up MRI due to financial reasons |
| 3. | Casanova et al.[14] | 2023 | Female, 17-year-old | Severe left-sided headache, nausea, vomiting, confusion, somnolence, white coat hypertension, history of polyarticular joint pain, malar rash | CT: left parietotemporal intraparenchymal hemorrhage, vasogenic edema, partial collapse of the left side ventricular system. MRV: absence of filling of the left transverse sinus | Intravenous antihypertensive medication, methylprednisolone, hydroxychloroquine, calcitriol, erythropoietin, anticoagulation (heparin), cyclophosphamide, renal replacement therapy due to acute kidney failure | Extubated without complications, improvement in symptoms, discharged on day 20. Cause of CVT determined to be systemic lupus erythematosus and antiphospholipid syndrome |
| 4. | Chen and Diaz[15] | 2024 | Male, 66-year-old | Sudden severe headache, impaired consciousness, right-sided motor preference | CT: Empty delta sign, intraparenchymal hemorrhage, subarachnoid hemorrhage, venogram for AVM suspicion | Mannitol, nimodipine, high-dose atorvastatin, anticoagulation with rivaroxaban | Symptoms improved with treatment; anticoagulation continued |
| 5. | Al Zahrani et al.[16] | 2019 | Female, 24-year-old, Pregnant | Generalized tonic-clonic seizure, unclear speech, eye-rolling, salivation | CT venogram: Superior sagittal sinus thrombosis, frontal lobe hemorrhage | LMWH, levetiracetam | Full recovery, continued LMWH; levetiracetam discontinued after 2 months |
| 6. | Nie et al.[17] | 2015 | Female, 27-year-old, Pregnant | Acute severe headache, slurred speech, conscious but afebrile | CT: Temporal hemorrhage, MRV: Left transverse sinus and sigmoid sinus thrombosis, DSA confirmed | Mannitol, LMWH followed by warfarin | Hemorrhage regressed; patient transitioned to warfarin therapy |
| 7. | Delahanty and Parker[18] | 2019 | Female, 31-year-old | Decreased consciousness, nausea, vomiting, urinary incontinence | CT revealed frontal lobe hemorrhage | Managed with decompressive craniectomy, anticoagulation, and post-operative heparin infusion. | Patient improved and resumed normal activities. |
| 8. | AlQahtani et al.[19] | 2024 | Male, 33-year-old, history of IgA nephropathy, mitral valve replacement | Severe headaches, loss of consciousness, convulsions, subdural hematoma, suspected systemic vasculitis, history of mouth ulcers, family history of lupus | CT: Subdural hematoma, ischemic infarction in right frontal-parietal and temporal lobes, cerebral venous thrombosis; MRI/MRA/MRV: Bilateral acute infarcts with bleeding, SSS thrombosis | Heparin infusion (switched to fondaparinux due to HIT), plasma exchange, IV methylprednisolone, IV hydrocortisone, acetazolamide, levetiracetam, CRRT, EVD insertion for intraventricular hemorrhage | Significant clinical progress, extubated, tracheostomy, new left parieto-occipital hemorrhage, occasional sedation for anger management, responding to basic commands |
| 9. | Patil and Faruqi[20] | 2024 | Male, 23-year-old, Indian | Altered consciousness, weakness, generalized tonic-clonic seizures | CT showed superior sagittal sinus abnormalities and evidence of CVST | Treated with LMWH, levetiracetam, and additional anticonvulsants. | Outcome not specified; ongoing treatment. |
| 10. | Shabbir et al.[21] | 2023 | Male, 44-year-old with hypertension and dyslipidemia | Collapsed in the CT scanner room during duty, experienced abrupt seizure-like activity, followed by postictal confusion | Non-contrast CT showed two small left parietal foci of intraparenchymal hemorrhage without ventricular extension or midline shift | Initially treated with heparin infusion; transitioned to oral anticoagulation after 2 days of treatment, seizure prophylaxis with phenytoin, and supportive care | Discharged after a week in the ICU with a planned follow-up in the Neurology clinic; unclear etiology of CVST, further outpatient workup planned |
| 11. | Torere B E, et al.[9] | 2023 | Male, 34-year-old with a history of methamphetamine abuse, intravenous drug use, and asthma | Right chest wall pain and swelling, pancytopenia, right-sided numbness, dysarthria, headaches, seizures, neurological decline | CT: Right parietal and left frontal hematomas, cerebral venous thrombosis (SSS and bilateral cortical veins), vasogenic edema, hemorrhagic venous infarcts | IV antibiotics, incision and drainage of abscess, chemotherapy for ALL (CALGB10403), palliative care, IV heparin, argatroban, switched to enoxaparin, filgrastim, Hyper CVAD, blinatumomab | Improved with residual left-sided weakness and slurred speech, complete remission of ALL, referred for stem cell transplantation |
CT: Computed tomography, MRI: Magnetic resonance imaging, MRA: Magnetic resonance angiography, MRV: Magnetic resonance venography, CVT: Cerebral venous thrombosis, CVST: Cerebral venous sinus thrombosis, LMWH: Low-molecular-weight heparin, SSS: Sinus sagittal superior, DSA: Digital subtraction angiography, CVAD: Cyclophosphamide, vincristine, adriamycin, and dexamethasone, ALL: Acute lymphoblastic leukemia, AVM: Arteriovenous malformation
CONCLUSION
This case underscores the critical elements involved in the diagnosis and management of CVST, emphasizing the interplay between clinical evaluation, imaging diagnostics, and therapeutic interventions. The patient presented with hallmark features of CVST, including persistent headache, seizures, and focal neurological deficits, which are well-documented manifestations of this condition. The occurrence of intracerebral hemorrhage, while complicating the clinical scenario, did not preclude the initiation of anticoagulation therapy, which remains the foundation of CVST treatment. The integration of anticoagulation with adjunctive measures for symptomatic management, such as analgesics for headache and antiepileptics for seizure control, resulted in significant clinical improvement, highlighting the efficacy of current evidence-based management strategies. This case emphasizes the necessity of prompt recognition, the use of advanced imaging modalities for accurate diagnosis, and strict adherence to established treatment protocols to achieve optimal clinical outcomes in patients with CVST.
Acknowledgments
Not applicable.
Authors’ contributions
MYA: Conceptualization, investigation, writing-original draft, writing-review, editing, and supervision. YAF: Conceptualization, investigation, writing-review, and editing.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Diagnosis and management of cerebral venous thrombosis: A scientific statement from the American Heart Association. Stroke. 2024;55:e77-90.
- [CrossRef] [Google Scholar]
- Diagnosis and management of cerebral venous sinus thrombosis with vaccine-induced immune thrombotic thrombocytopenia. Stroke. 2021;52:2478-82.
- [CrossRef] [PubMed] [Google Scholar]
- D-dimer level associated with amount of sinus involvement using digital subtraction angiography on cerebral venous thrombosis patients. J Blood Med. 2023;14:303-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral venous sinus thrombosis with hemorrhagic infarct: A rare presentation in a risk-defying male patient. Radiol Case Rep. 2023;19:153-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral venous thrombosis. Rev Clin Esp (Barc). 2024;224:237-44.
- [CrossRef] [PubMed] [Google Scholar]
- Aphasic syndromes in cerebral venous and dural sinuses thrombosis-a review of the literature. Life (Basel). 2022;12:1684.
- [CrossRef] [Google Scholar]
- Cerebral venous thrombosis presented with symmetrical crescent-shaped intracranial hemorrhage in alcoholic liver disease: Case reports. Medicine (Baltimore). 2024;103:e37441.
- [CrossRef] [Google Scholar]
- Diagnostic and therapeutic challenges of concurrent intracranial hemorrhage and cerebral venous thrombosis in a patient with acute lymphoblastic leukemia: A case report and literature review. Cureus. 2023;15:e37482.
- [CrossRef] [Google Scholar]
- D-dimer levels in patients with suspected acute cerebral venous thrombosis. Am J Med. 2002;113:238-41.
- [CrossRef] [PubMed] [Google Scholar]
- BET 1: Does a normal D-dimer rule out cerebral venous sinus thrombosis (CVST)? Emerg Med J. 2018;35:396-7.
- [CrossRef] [PubMed] [Google Scholar]
- New oral anticoagulants versus warfarin for cerebral venous thrombosis: A multi-center, observational study. J Stroke. 2019;21:220-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral venous sinus thrombosis presenting with multifocal intracerebral hemorrhage and subarachnoid hemorrhage: A case report. Medicine (Baltimore). 2018;97:e13476.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral venous thrombosis in a 17-year-old female patient: A case report. Cureus. 2023;15:e42384.
- [CrossRef] [Google Scholar]
- Cerebral venous sinus thrombosis presenting as intracerebral hemorrhage and subarachnoid hemorrhage: A case report. J Med Univ Santo Tomas. 2024;8:1371-6.
- [CrossRef] [Google Scholar]
- Cerebral Venous sinus thrombosis with an intracranial haemorrhage: A case report. Open Access Maced J Med Sci. 2019;7:1029-31.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral venous sinus thrombosis with cerebral hemorrhage during early pregnancy. Neurosciences (Riyadh). 2015;20:48-51.
- [Google Scholar]
- A case of central venous sinus thrombosis in a young woman. Clin Pract Cases Emerg Med. 2019;3:345-8.
- [CrossRef] [PubMed] [Google Scholar]
- Multifaceted cerebral venous thrombosis with extensive intra-cerebral hemorrhage in a young man with mitral valve replacement due to thrombosis and IgA nephropathy: A challenging case report from Saudi Arabia. Cureus. 2024;16:e60016.
- [CrossRef] [Google Scholar]
- A case report of simultaneous intracranial hemorrhage and cerebral venous sinus thrombosis in a young Indian male: Diagnostic and therapeutic challenges. Cureus. 2024;16:e55642.
- [CrossRef] [Google Scholar]
- A 44-year-old male with cerebral venous sinus thrombosis. Cureus. 2023;15:e36974.
- [CrossRef] [Google Scholar]







