Translate this page into:
Clinical Profile, Outcome, and Prognostic Factors of Cortical Venous Thrombosis in a Tertiary Care Hospital, India
Address for correspondence: Dr. Basavaraj Fakkirappa Banakar, Department of Neurology, SDM Medical College and Hospital, Sattur, Dharwad, Karnataka, India. E-mail: drbanakar2006@yahoo.co.in
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Cortical venous thrombosis (CVT) is a rare condition, compared to arterial stroke and often occurs in young individuals presenting with varying clinical features.
Aim:
The aim is to study clinical profile and assess the outcome and prognostic factors of CVT patients.
Methodology:
A case series study was done for 2 years. CVT cases confirmed by magnetic resonance imaging were included in this study. Clinical presentation and risk factors were noted then patients were assessed at the time of discharge for their physical and mental status. Modified Rankin scale was used to group patients, accordingly scores 0–2 were considered as good and 3–6 as poor outcome, respectively. Data were analyzed using Chi-square test to know the association between prognostic factors and outcome.
Results:
Out of 81 patients, more than half of the patients were in the age group of <35 years (55.6%), and majority of patients were females (79%). Most common symptom was headache (82.7%) and least was fever (14.8%). Superior sagittal sinus was most commonly involved (74.1%). Nearly half of the patients were in puerperal period (44.1%). Patients aged more than 35 years (odds ratio [OR]: 9.1, confidence interval [CI]: 4.463–19.750) presenting with symptoms such as fever (OR: 3.442, CI: 1.088–12.140), impaired consciousness (OR: 5.467, CI: 2.064–15.330) and having clinical signs such as coma (OR: 23.99, CI, 3.844–544.1), papilledema (OR: 25.15, CI: 7.565–101.5), and with focal neurological deficit (OR: 9.366, CI: 2.693–3.41) had statistically significant poor outcome.
Conclusion:
Females formed a major bulk of patients. Higher number patients showed poor outcome. Study showed association between age, headache, impaired consciousness, coma, papilledema, and neurological deficit to poor outcome.
Keywords
Cortical venous thrombosis
modified Rankin scale
stroke
INTRODUCTION
Cortical venous thrombosis (CVT) is any thrombosis that occurs in intracranial veins or sinuses.[1] Cerebral vein and sinus thrombosis is rare compared to arterial stroke and often occurs in young individuals.[2] Worldwide estimated annual incidence is 3–4 cases/1 million population, about 75% of the adult patients are women.[3] With reference to India, there are no definitive data as there are no multicenter hospital-based studies.
The spectrum of clinical manifestation varies; headache is the most common symptom.[4] Seizures occur in about 7%–15% of cases during presentation and in about 40% during the course of illness, and they may be focal or generalized in almost equal proportion.[5] Patients may also present with long-lasting focal neurological deficits or transient focal neurological deficits mimicking transient ischemic attacks.[6] Other common symptom is altered sensorium.
Etiological factors vary depending on geographical area and also according to anatomical site involved. Primary or idiopathic CVT is mainly caused by hypercoagulable state. Secondary thrombosis results from a variety of causes that include injury, infection, hematological disturbances, and dehydration. In India, CVT is very common in the early puerperal period (postpartum period till 6 weeks), 10–12 times higher than in the west and as a whole puerperal CVT may account for about 15%–20% of stroke victims of younger age.[78]
A meta-analysis of the most recent prospectively collected series, in which the weight of the International Study on Cerebral Veins and Dural Sinus Thrombosis cohort is very important, showed an overall 15% case-fatality or dependency rate.[6] With the advent of imaging modalities such as computed tomography (CT) scan and magnetic resonance imaging (MRI) and MR venography (MRV), the diagnosis and respective management has improved significantly. Hence, we started our study with following objectives to study clinical profile and assess the outcome and prognostic factors of CVT patients.
METHODOLOGY
A case series study was done for 2 years in a tertiary care hospital in North India. During study period, patients aged more than 18 years which are confirmed as CVT from clinical features and investigations such as CT scan of the brain with contrast or MRI with MRV were considered. Cases where CT scan of the brain showing hemorrhage or infarct in the distribution of arterial territory, neoplastic and granulomatous disease of the brain, and eclampsia or preeclampsia cases were excluded from the study.
Clinical examination was done to note focal neurological deficits and mental status. A cerebrospinal fluid analysis was considered in cases with no contraindications to lumbar puncture. All patients were assessed at the time of discharge for physical and mental status to look for outcome.
Data were collected using pretested semi-structured questionnaire. Demographic data, clinical features, and risk factors were noted. Data were entered in Excel sheet, and appropriate descriptive statistics were done to describe demographic and clinical features. Chi-square test was applied to find association between prognostic factors and outcome. Accordingly, modified Rankin scale was used to assess outcome, scores between 0 and 2 were considered as good and 3–6 as poor outcome, respectively. To analyze data, SPSS version 20 (SPSS version 20, IBM, New York, USA) was used. A P < 0.05 was fixed as significant and P < 0.01 as highly significant.
RESULTS
A total of 81 patients formed as our study participants, more than half of the patients were in the age group of <35 years (55.6%), and majority of patients were females (79%). The most common symptom of presentation of patients was with headache (82.7%), seizure (63%), and focal neurological deficit (63%) and least common symptom was fever (14.8%) [Table 1].
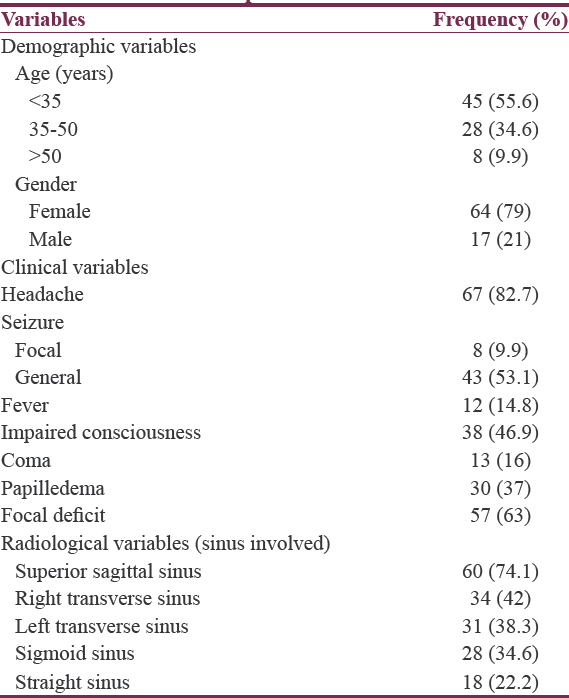
According to radiological findings, the most common involved sinus was superior sagittal sinus (74.1%) and then right transverse sinus (42%).
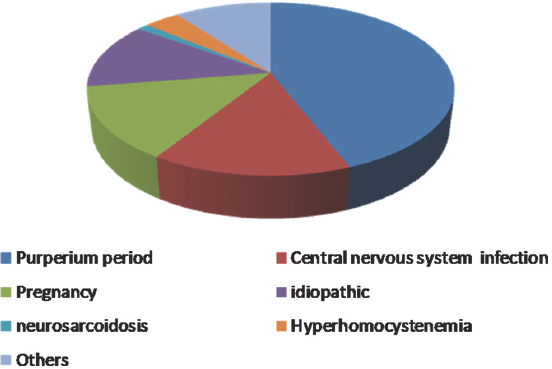
Nearly half of the patients were in puerperal period (44.1%) followed by other risk factors such as central nervous system infection (14.8%), pregnancy (13.6%), and idiopathic (12.4%). The least common risk factor was neurosarcoidosis (1.2%) [Figure 1].
- Pie chart showing distribution of patients according to risk factors
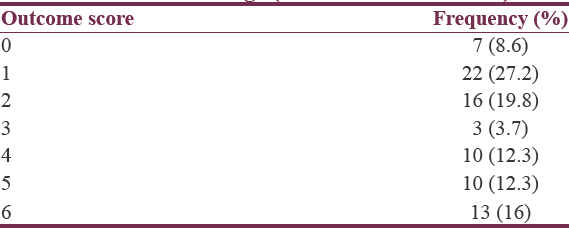
More than half of them had good scores, 45 (55.6%) with score 0 (8.6%), score 1 (27.2%), score 2 (19.8%), whereas 36 (44.4%) had poor outcome [Table 2].
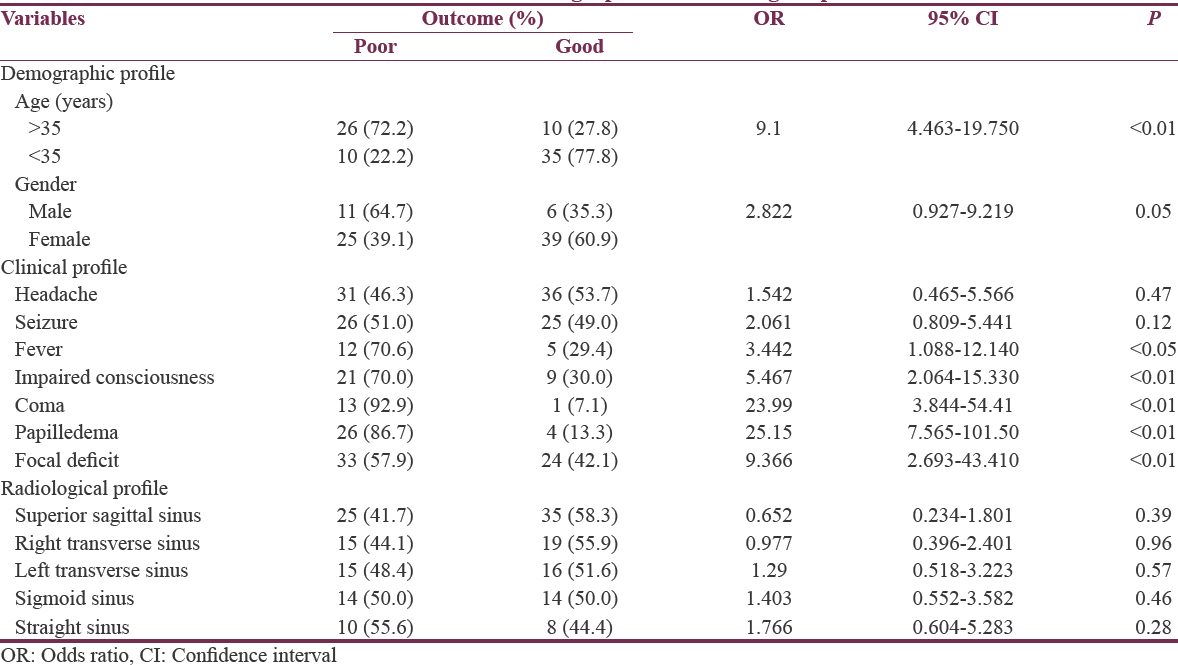
Patients aged more than 35 years had poor outcome (72.2%) compared to patients aged <35 years (22.2%) and was statistically significant (OR: 9.1, CI: 4.463–19.750). Patients who had symptoms such as fever (OR: 3.442, CI: 1.088–12.140), Impaired Conciousness (OR: 5.467, CI: 2.064–15.330), coma (OR: 23.99, CI: 3.844–544.1), papilledema (OR: 25.15, CI: 7.565–101.5), and presenting with focal neurological deficit (OR: 9.366, CI: 2.693–3.41) had statistically significant poor outcome [Table 3].
DISCUSSION
A total of 81 patients were included during study period with age range from 18 to 70 years (mean ± standard deviation: 30.2 ± 9.15).
More than half of our patients were in the age group <35 years (55.6%). This is in conformity with most of the earlier studies by Ameri and Bousser[9] (61%), Daif et al.,[10] Deschiens et al.,[11] Nagaraja et al.,[12] and Narayan et al.[13] The present study showed a female preponderance with ratio of male to female patients being 1:3.76 because of influence of pregnancy, puerperium, and oral contraceptive pills, whereas ratio was 1:1.29 in study done by Ameri and Bousser[9] and 1:1 by Daif et al.,[10] and studies done in India showed higher number of female patients such as 1:1.38 by Patil et al.[14] and 1:1.4 by Mehta et al.[15]
CVT presents with a wide spectrum of symptoms and signs. Patients presented with headache, foal deficit, seizure, papilledema, impaired consciousness, and coma in the order of decreasing frequency.
In the present study, most of the patients (82.7%) presented with headache. Similar results were observed in studies done by Daif et al.[10] (82%), Einhäupl et al.[16] (91%), Ameri and Bousser[9] (74%), Nagaraja et al.[12] (71%), Narayan et al.[13] (94.4%), Vishwanath et al.[17] (94%), and Halesh et al.[18] (95%).
Around (63%) of patients presented with focal deficit such as hemiparesis, monoparesis, and paraparesis with cranial nerve palsy (18.5% with 7th nerve, 4.9% with 3rd nerve, and 2.5% with 4th nerve palsy). A similar results were observed by Stolz et al.[19] (56.9%), whereas in a study done by Halesh et al.,[18] only 48% presented with focal deficits, this may be due difference in number of patients.
Seizure was seen in 62% of cases. It is a common symptom of CVT next to headache. It may be generalized, focal, or with secondary generalization. In Einhäupl et al.[16] (48%) and in Barinagarrementeria et al. (60%),[20] patients presented with seizures which were comparable to our study. Papilledema was seen in 37% of patients. Accordingly, it varied from (27%) Einhäupl et al.[16] to (45%) by Bousser et al.[2]
In the present study, 54% of patients presented with altered sensorium, out of which 38% were having Glasgow coma scale (GCS) between 9%, 13% and 16% were having GCS <9, i.e., comatose. In a study conducted by Barinagarrementeria et al.,[20] altered sensorium was present in 63%, which was comparable to our study. Other symptom was fever seen in 16% of cases which may be secondary to infection such as otitis media, meningitis, and septic thrombotic process.
Female patient contributed majority, among females, more than half were in puerperal period, i.e., 36 (56.25%) and only 6 (9.37%) were on oral contraceptive pills. A very low proportion of <15% postpartum cases was noted from studies done by Ferro et al.,[21] De Bruijn et al.,[5] and Deschiens et al.[11] The reasons may be because of postpartum hypercoagulable state combined with culturally practiced water restriction and high fatty diet.
Infection was found in 14.8% of patients. All patients were suffering from meningitis secondary to otitis media which was comparable to Bousser et al.[2] Other risk factors for CVT in decreasing order of frequency were pregnancy (13.6%), hyperhomocysteinemia (3.7%), dehydration (2.5%), and neurosarcoidosis (1.2%). In remaining 12.4% of cases, causes could not identify and named as idiopathic.
The superior sagittal sinus was most common sinus involved in 74.1% of the cases, either alone or with other sinuses. In studies by Ameri and Bousser[9] (72%) and Daif et al.[10] (85%), superior sagittal sinus was involved which was comparable to our study. Other sinuses involved in decreasing order of frequency were right transverse sinus (42%), left transverse sinus (38.3%), sigmoid sinus (34.6%), and straight sinus (22.2%), respectively.
At the time of discharge, 44.3% of patients had poor outcome with 27.3% of patients having dependent morbidity and 16% of mortality. Patients aged more than 35 years had poor outcome compared to younger age group (OR: 9.1, CI: 4.463–19.750). Similar results were observed in studies done by Stolz et al.,[19] Ferro et al.,[21] and De Bruijn et al.[5]
The present study showed that males had a poor outcome compared to females but was statistically not significant (OR: 2.822, CI: 0.927–9.219). Many of the previous studies such as Halesh et al.[18] and Ferro et al.[21] also showed poor outcome for males. However, there was not much difference in outcome in a study done by Narayan et al.[13]
Patients who had history of fever (OR: 3.442, CI: 1.088–12.140) and impaired consciousness (OR: 5.467, CI: 2.064–15.330) were associated with poor outcome.
The study showed that patients who had coma (OR: 23.99, CI, 3.844–544.1), papilledema (OR: 25.15, CI: 7.565–101.5), and presenting with focal neurological deficit (OR: 9.366, CI: 2.693–3.41) were also associated with poor outcome which were statistically significant. Similar results were observed by Ferro et al.[21] with respect to coma and hemiparesis or any deficit at the time of diagnosis.
Patients who had seizure also had a poor outcome but was statistically not significant (OR: 2.061, CI: 0.809–5.441), whereas in a study by Stolz et al.[19] who studied 79 patients, more than two seizures despite antiepileptic treatment was associated with poor outcome, and patients with history of headache had a comparatively better outcome but that was also statistically not significant (OR: 1.542, CI: 0.465–5.566).
Involvement of any of the sinuses was not associated with poor outcome. However, involvement of only straight sinus was associated with poor outcome but was statistically not significant (OR: 1.766, CI: 0.6046–5.283), and similar findings were seen in De Bruijn et al.[5]
As compared to earlier studies, the present study shows higher number of dependency and death rate. This discrepancy in the studies from Western countries and our study may be attributed to the fact that our institution being a referral center receiving patients with comparatively poor prognosis. In addition, patients in this setup seek alternative interventions leading to delay in medical intervention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: Results of the international study on cerebral vein and dural sinus thrombosis (ISCVT) Stroke. 2004;35:664-70.
- [Google Scholar]
- Headache as the only neurological sign of cerebral venous thrombosis: A series of 17 cases. J Neurol Neurosurg Psychiatry. 2005;76:1084-7.
- [Google Scholar]
- Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients. Cerebral venous sinus thrombosis study group. J Neurol Neurosurg Psychiatry. 2001;70:105-8.
- [Google Scholar]
- Cerebral venous thrombosis: Update on clinical manifestations, diagnosis and management. Ann Indian Acad Neurol. 2008;11:S79-87.
- [Google Scholar]
- Cerebral venous and arterial thrombosis in pregnancy and puerperium. A study of 135 patients. Angiology. 1983;34:731-46.
- [Google Scholar]
- Postpartum cerebral venous thrombosis study of autopsy material. Neurol India. 1973;21:19-22.
- [Google Scholar]
- Cerebral venous thrombosis in adults. A study of 40 cases from Saudi Arabia. Stroke. 1995;26:1193-5.
- [Google Scholar]
- Coagulation studies, factor V Leiden, and anticardiolipin antibodies in 40 cases of cerebral venous thrombosis. Stroke. 1996;27:1724-30.
- [Google Scholar]
- Puerperal cerebral venous thrombosis: Therapeutic benefit of low dose heparin. Neurol India. 1999;47:43-6.
- [Google Scholar]
- Risk factors, clinical profile, and long term outcome of 428 patients of cerebral sinus venous thrombosis: Insights from Nizam's Institute Venous Stroke Registry, Hyderabad, India. Neurol India. 2012;60:154-9.
- [Google Scholar]
- Clinical profile and outcome of cerebral venous sinus thrombosis at tertiary care center. J Neurosci Rural Pract. 2014;5:218-24.
- [Google Scholar]
- Cortical venous thrombosis-changing scenario. Abstracts of 59th annual conference of API 18-21 January, 2004, Hyderabad. J Assoc Physicians India. 2003;51:1196.
- [Google Scholar]
- A study of the clinical profile of cerebral venous sinus thrombosis. J Dent Med Sci. 2014;13:61-6.
- [Google Scholar]
- A study of the clinical features and the outcome of cerebral venous sinus thrombosis in a tertiary care centre in South India. J Clin Diagn Res. 2011;5:443-7.
- [Google Scholar]
- Cerebral venous thrombosis: An all or nothing disease? Prognostic factors and long-term outcome. Clin Neurol Neurosurg. 2005;107:99-107.
- [Google Scholar]
- Aseptic cerebral venous thrombosis: Proposed prognostic scale. J Stroke Cerebrovasc Dis. 1992;2:34-9.
- [Google Scholar]
- Dural sinus thrombosis mimicking “capsular warning syndrome”. J Neurol. 2000;247:802-3.
- [Google Scholar]






