Translate this page into:
Cerebellar ataxia in a young patient: A rare path to lupus
Address for correspondence: Dr. Kaushik Ghosh, Flat 3b, Padma Apartment, 110 DR M N Saha Road, Kolkata - 700 074, West Bengal, India. E-mail: drkaushikghosh@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cerebellar ataxia is a rare manifestation of neuropsychiatric systemic lupus erythematosus (SLE). Development of vasculitic infarcts in the cerebellum is the most plausible reason of this manifestation. We report the case of a patient who presented with characteristic skin rashes of lupus along with cerebellar signs. Imaging of brain in this patient revealed prominent cerebellar atrophy. She was treated with mycophenolate mofetil and oral corticosteroid, and there was no further progression of her neurological signs after the initiation of therapy. In the clinical context of varied presentations of neurolupus, this is one of the rare sightings and our treatment protocol holds promise as first-line therapy in future.
Keywords
Ataxia
immunosuppression
systemic lupus erythematosus
Introduction
Cerebellar ataxia is one of the less-described neurological manifestations of systemic lupus erythematosus (SLE). The prevalence of ataxia in patients with systemic lupus is not known. Most of the patients present with acute to subacute onset cerebellar syndromes. Some of them were seen to have vasculitic infarcts in cerebellum on magnetic resonance imaging (MRI). However, the presence of cerebellar atrophy at the outset is even rarer.[1] Volume loss of cerebellum cannot be traced to the known pathogenic mechanisms of lupus. Although autoantibodies are present in such patients, there is no specific pattern attributing to the condition. Anti-Purkinje cell antibody[2] and anti-neuronal cell antibody[3] have been described in the literature without large-scale validation. On the other hand, autoimmune conditions like Sjogren's syndrome and systemic sclerosis are also associated with rare instances of cerebellar syndrome. There is an overlap of autoantibody positivity between SLE and other autoimmune conditions, e.g. high titers of antinuclear antibody in Sjogren's syndrome.[4] It may also be noted that a minority of these patients were found to have cerebellar atrophy, and such patients were less likely to respond to immunosuppression.
Case Report
A 22-year-old girl was admitted with clumsiness of movements, loss of balance while walking and generalized skin rash for last 2 months. She was asymptomatic prior to this time, without any joint pain, oral ulcers, alopecia or urinary symptoms. She first noted a difficulty in fine movements during cooking and sewing which she described as “hands going past the point she intended.” Two weeks later, she was unable to walk along a straight line and needed a support to move about indoors. Seven days prior to admission, she noted reddish eruptions over her face and the trunk. The patient was a married woman who stayed at home. She did not have history of drug use, allergies or any major illness in the past. Both of her parents had hypertension, and her siblings were reportedly healthy. On admission, the patient's pulse was 88 beats/min, blood pressure 140/94 mmHg, respiratory rate 22/min and SpO₂ 95% while inhaling room air. General examination revealed pallor (1+), edema (2+), non-scarring diffuse alopecia, malar “butterfly” rash and a generalized papular eruption. She had prominent bilateral cerebellar signs, e.g. past-pointing, dysdiadochokinesia along with truncal ataxia. Ocular movements were normal; notably, nystagmus was absent. The patient had a cerebellar dysarthria. There were no signs of papilledema on funduscopic examination. Neurological examination was otherwise normal. Initial investigations showed the presence of normochromic normocytic anemia, raised erythrocyte sedimentation rate, proteinuria (2+) and hypocomplementemia [Table 1]. Magnetic resonance imaging of the brain revealed prominent generalized cerebellar atrophy [Figure 1]. There were no evidences of any neoplasm or ischemia. Serological profile for hepatitis B, hepatitis C and human immunodeficiency virus were negative. Autoimmune profile, however, was positive for antinuclear antibody (1:320 titer, speckled pattern) and anti-dsDNA antibody (1:640 titer). Further work up was done to evaluate the renal status of the patient, which revealed lupus nephritis (International Society of Nephrology class IV, subclass A/C). The patient was diagnosed as a case of SLE with nephropathy. She was treated with mycophenolate mofetil (2 g/day), prednisolone (40 mg/day) and hydroxychloroquine (400 mg/day). After 3 months of follow-up, she has no proteinuria or active urinary sediments and her neurological features have remained static. As a corollary, her cerebellar atrophy can be attributed to SLE.

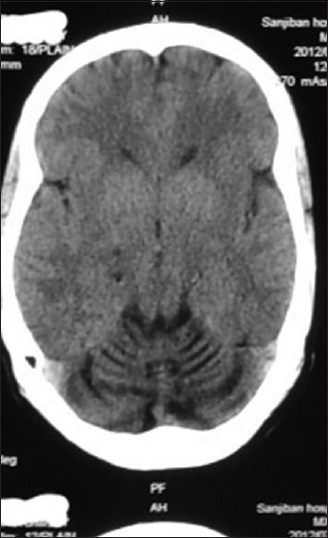
- CT scan of brain showed atrophy of the entire cerebellum. There was no evidence of ischemic change
Discussion
The patient's neurological signs suggested a disorder affecting both the hemispheres and vermis of the cerebellum. The tempo of the disease progression could be explained by a demyelinating disorder, a neoplasm or a vasculitic syndrome. The associated features of rash, hypertension and edema tilted the balance toward a multisystem disorder, possibly vasculitis. On the other hand, the absence of definitive signs of raised intracranial tension weighed against the presence of a neoplasm which otherwise affected both cerebellar hemispheres. In this patient, the possibility of a first attack of demyelinating disorders like multiple sclerosis was considered, but there were no suggestive features on brain imaging. Final diagnosis of the patient as SLE was confirmed with the help of autoimmune markers and histopathology. Reports of cerebellar ataxia in lupus demonstrated response to immunosuppression with high-dose intravenous corticosteroid.[5] In rare instances, a biopsy of cerebellum revealed dense microglial infiltration and perivascular neutrophilic invasion.[6] As specific markers of cerebellar affection in SLE have not been validated, a response to therapy can be accepted as a surrogate marker of immunopathogenesis. However, therapy with mycophenolate mofetil in such a situation has not been reported. So to conclude, we report an interesting case of cerebellar atrophy in SLE with clinical response to a combined regimen with mycophenolate mofetil and oral steroid.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Subacutepancerebellar syndrome associated with systemic lupus erythematosus. Clin Neurol Neurosurg. 1996;98:157-60.
- [Google Scholar]
- Subacute cerebellar ataxia and atrophy developed in a young woman with systemic lupus erythematosus whose cerebrospinal fluid was positive for antineuronal cell antibody. Lupus. 2012;21:324-8.
- [Google Scholar]
- Cerebellar degeneration associated with Sjögren'ssyndrome. JClinNeurol. 2012;8:155-9.
- [Google Scholar]
- Massive vasculitic cerebellar infarction in patient with systemic lupus erythematosus. Neurol India. 2012;60:106-8.
- [Google Scholar]






