Translate this page into:
A Rare Case of an Extensive Multi-compartment Epidermoid Presenting with Pure Motor Trigeminal Neuropathy, Case Report and Review of Literature
Address for correspondence: Dr. Prakash Nair, Department of Neurosurgery, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum - 695 011, Kerala, India. E-mail: drprakashnair@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Epidermoid cysts are benign slow-growing tumors, clinical signs and symptoms at the time of presentation are related to the location and extent of the lesion. The motor fibers of the trigeminal nerve are fairly resistant to extraneous compression. Intracranial lesions in the vicinity of the trigeminal nerve usually present with sensory symptoms without affecting the motor component. We report a rare case of a middle cranial fossa epidermoid presenting with pure motor trigeminal neuropathy.
Keywords
Epidermoid
meckel's cave epidermoid
trigeminal motor neuropathy
INTRODUCTION
Epidermoid cyst comprises about 1.8%–2% of intracranial tumors. They commonly occur in the cerebellopontine angle (CPA) and parasellar region.[1] Trigeminal neuralgia is a common presenting complaint in these cases. Pure motor trigeminal neuropathy is an unusual condition, and the association of an intracranial epidermoid with pure trigeminal motor neuropathy is still more infrequent. We present a rare case of an extensive multicompartment epidermoid involving the CPA and the middle cranial fossa which presented with pure motor trigeminal neuropathy.
CASE REPORT
A 43-year right-handed male presented with difficulty in chewing food and progressive hollowing of the left temporalis muscle over a period of 2 years. Clinical examination was suggestive of atrophy of the left masseter and temporalis muscles, on examination, his jaw deviated to the left on opening his mouth [Figure 1]. However, he had no sensory deficits in the distribution of the trigeminal nerve.

- Clinical image: Arrow showing temporal hollowing and masseter hollowing and deviation of jaw toward the same side indicating muscle atrophy and motor weakness
Computerized tomography revealed a nonenhancing hypodense lesion in the left CPA extending into the region of the Meckel's cave. Magnetic resonance imaging revealed a well-defined extra-axial lesion measuring 3.5 cm × 4.5 cm × 6.6 cm, occupying the left CPA cistern and extending anteriorly into the region of the Meckel's cave and the suprasellar cistern. This lesion was hypointense on T1W and hyperintense on T2W sequences, with decreased apparent diffusion coefficient and restricted diffusion within the lesion in diffusion-weighted imaging. The imaging features were suggestive of an intracranial epidermoid [Figure 2].
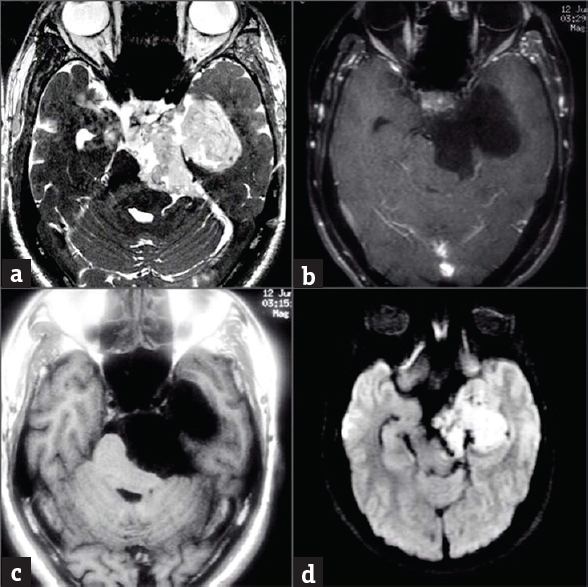
- Preoperative images: (a) T2 CISS image showing hyperintense leon in the left cerebellopontine angle cistern, left Meckel's cave and left side of basilar, (b): Contrast image showing no contrast enhancement of lesion, (c): T1-weighted image hypointense lesion in the left cerebellopontine angle (d): Diffusion-weighted imaging image showing Diffusion restriction within lesion
He underwent a surgery through a left frontotemporal craniotomy. After dissecting the Sylvian fissure, the epidermoid was seen lateral to the 3rd cranial nerve, occupying middle cranial fossa, extending posteriorly into posterior fossa till the brainstem. Laterally, the lesion was displacing the medial temporal lobe. The tumor was removed piecemeal, except for a part of the posterior capsule attached to the brainstem which was left behind. The patient had no new neurological deficits following surgery. Postoperative imaging showed residual lesion in the posterior aspect of the resection cavity [Figure 3]. The histopathological examination was consistent with an epidermoid cyst.
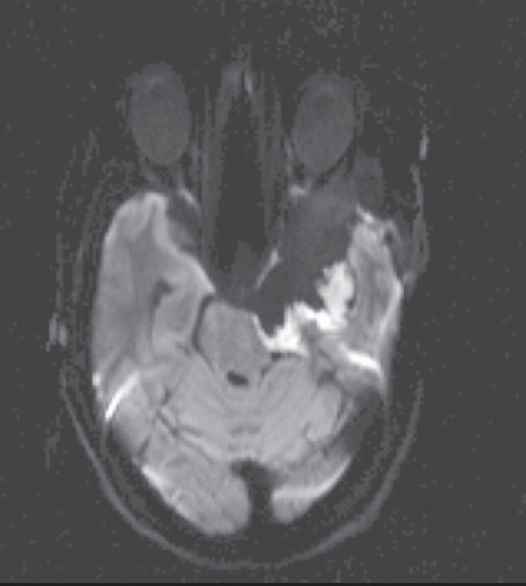
- Diffusion-weighted imaging postoperative image suggestive of small residual in posterior part of resection cavity
DISCUSSION
The most common intracranial location of epidermoid cyst is the CPA. They can also be found in the fourth ventricle, cerebellum, cerebral hemisphere, brainstem, and lateral ventricle. Epidermoid cyst of the CPA commonly present with trigeminal neuropathy, gait unsteadiness, abducens nerve palsy, facial weakness, and chemical meningitis.[1] Pure trigeminal motor neuropathy is an uncommon presentation for intracranial tumors. We have noted very few cases of pure motor trigeminal neuropathy in literature.[2]
The motor portion of trigeminal nerve begins from pontine tegmentum with motor nucleus lying medial to a large sensory nucleus. The motor fibers lie within the mandibular nerve which exits through the foramen ovale to supply the masticatory muscles. Lesions anywhere from the pontine tegmentum to the foramen ovale can present with motor weakness.
Pure motor trigeminal neuropathy is usually associated with conditions such as pontine infarction, viral infections, autoimmune conditions, head trauma or have a developmental origin.[3] Chia has reported five cases of pure trigeminal motor neuropathy, three of which were preceded by a common cold.[2] In our case, there was no associated upper respiratory infection nor any sign and symptoms of systemic infection. Li et al. reported synaptobrevin II expression to be more in motor neurons as compared to sensory neurons.[4] The difference in the specificity of this membrane protein in the motor and sensory system may account for the susceptibility of the motor neurons to specific viral infections. Mass lesion causing pure trigeminal motor neuropathy is very rare. Lee et al. reported a case of trigeminal motor neuropathy due to infarction of the pontine tegmentum.[5] Similarly, Park et al. reported a mass lesion in the foramen ovale causing pure motor neuropathy of trigeminal nerve.[6]
Kobata et al. reported 30 cases of cerebellopontine (CP) angle epidermoid, of these 29 cases presented with trigeminal neuralgia.[7] Vinchon et al. reported nine cases of CP angle epidermoid where only one patient had trigeminal neuropathy, and none had motor involvement.[8] Yamakawa et al. reported 33 cases of epidermoid among which four cases were in the CP angle. Only one among the four cases had 5th cranial nerve dysfunction with motor and sensory involvement.[9]
CONCLUSION
Numerous intracranial mass lesions cause trigeminal neuropathy; however, the rarity of motor involvement in such cases is still not convincingly explained.
To the best of our knowledge, this is the only case of a mass lesion producing pure motor neuropathy of the trigeminal nerve. We suggest that the pure motor trigeminal neuropathy is predominantly due to the sensitivity of motor fibers to the contents of the epidermoid. However, we are unable to find any specific cause for pure trigeminal motor involvement in our case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Progressive facial asymmetry due to trigeminal motor neuropathy. Eur Neurol. 2006;55:96-8.
- [Google Scholar]
- Axonal transport and distribution of synaptobrevin I and II in the rat peripheral nervous system. J Neurosci. 1996;16:137-47.
- [Google Scholar]
- Acute pontine infarction presenting with isolated unilateral masticatory muscle weakness. Korean J Clin Geriatr. 2015;16:84-7.
- [Google Scholar]
- Unilateral trigeminal mandibular motor neuropathy caused by tumor in the foramen ovale. J Clin Neurol. 2006;2:194-7.
- [Google Scholar]
- Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: Pathogenesis and long-term surgical results in 30 patients. Neurosurgery. 2002;50:276-85.
- [Google Scholar]
- Intradural epidermoid cysts of the cerebellopontine angle: Diagnosis and surgery. Neurosurgery. 1995;36:52-6.
- [Google Scholar]
- Clinical course and surgical prognosis of 33 cases of intracranial epidermoid tumors. Neurosurgery. 1989;24:568-73.
- [Google Scholar]






