Translate this page into:
Cloud-like pattern of mineralization in skull base osteosarcoma
Address for correspondence: Dr. Lakshmi Narayan Garg, Department of ENT, MM Institute of Medical Sciences & Research Maharishi Markandeshwar University, Mullana- Ambala, 133-203 (Haryana), India. E-mail: dr.lngarg@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Osteosarcoma derives from primitive bone-forming mesenchymal cells, although it is the most common primary bone malignancy,[1–2] osteosarcoma of the skull base is very rare.[13–6] A 40-year-old woman, a known case of left temporal bone osteosarcoma operated 3 years back, now presented with progressively increasing swelling over the previously operated site for the previous 6 months and foul smelling discharge for 3 days. Not able to take food, breathing difficulty, and was in altered sensorium. At the time of initial presentation (3 years back) there was pinkish, firm to hard, moderately vascular, nonsuckable tumor, infiltrating into the temporal muscle and fascia with ill-defined plane of cleavage. The tumor was adherent to the dura but there was no dural invasion. Histologically the tumor comprised highly pleomorphic tumor cells, findings suggestive of anaplastic variant of osteosarcoma and a poor prognosis was predicted. The patient received a course of chemotherapy but did not receive radiotherapy. Plain axial CT images of the head soft tissue and bone showed an aggressive, densely ossified bone-forming tumor with extensive involvement of the soft tissue and bony destruction of the anterior, middle, and part of the posterior cranial fossa on left side [Figure 1]. The patient was managed conservatively but did not do well and expired after 3 days of admission.
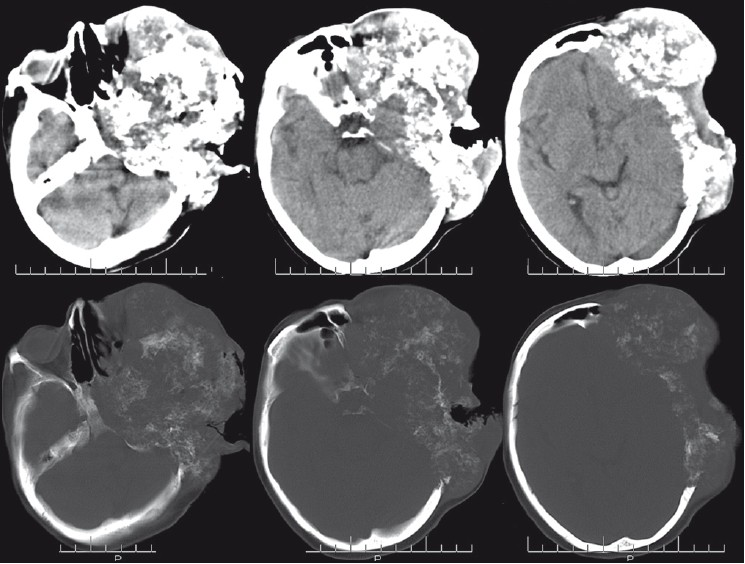
- Plain axial CT images of the head soft tissue and bone showing an aggressive, densely ossifi ed bone-forming tumor with extensive involvement of the soft tissue and bony destruction of the anterior, middle, and part of the posterior cranial fossa on left side producing cloud-like pattern of mineralization
Fibro-osseous lesions are characteristically centered within bone and surface fibro-osseous lesions prompt consideration of parosteal osteosarcoma, which is rare but well documented in the skull.[7] Because of the superimposed bony structures, conventional radiographs are of limited worth in evaluating head and neck osteosarcomas.[8] However, CT and plain films are superior to MR in detecting the matrix calcifications and bone destruction or reaction.[8] CT provides excellent detection of tumor calcification, cortical involvement, and, in most instances, soft tissue as well as intramedullary extension[8] as in the present case, on axial CT poorly defined destructive osteosarcoma that neoplasm extends into the soft tissues produces cloud-like pattern of mineralization.[2] The key to disease-free survival in treating primary osteosarcoma of the calvarium is complete surgical resection with immediate reconstruction followed by adjuvant chemotherapy.[4] In skull base osteosarcoma, prognosis is poor even in patients who have received adequate therapy.[6]
Source of Support: Nil
Conflict of Interest: None declared.
References
- Update on bone forming tumors of the head and neck. Head Neck Pathol. 2007;1:87-93.
- [Google Scholar]
- Osteosarcoma of the skull base: Case report and review of literature. Int J Pediatr Otorhinolaryngol. 2008;72:115-9.
- [Google Scholar]
- Long-term management of craniofacial osteosarcoma. J Craniofac Surg. 2009;20:406-9.
- [Google Scholar]
- Craniofacial reconstruction of primary osteogenic sarcoma of the skull. J Plast Reconstr Aesthet Surg. 2010;63:1265-8.
- [Google Scholar]
- Protuberant fibro-osseous lesion of the temporal bone: “Bullough lesion”. Am J Surg Pathol. 2010;34:1217-23.
- [Google Scholar]
- Craniofacial osteosarcomas: Plain film, CT, and MR findings in 46 cases. AJR Am J Roentgenol. 1988;150:1397-402.
- [Google Scholar]





