Translate this page into:
Utilization patterns of central nervous system drugs: A cross-sectional study among the critically ill patients
Address for correspondence: Dr. Lisha Jenny John, Department of Pharmacology and Research Division, Gulf Medical University, Ajman, UAE 4184. E-mail: drlishaj@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Critically ill patients often receive central nervous system drugs due to primary disorder or complications secondary to multiorgan failure. The aim of the study was to evaluate the current utilization pattern of central nervous system drugs among patients in the medical intensive care unit.
Materials and Methods:
A prospective observational study carried out over a period of 1 year. The relevant data on drug prescription of each patient was collected from the inpatient case record. Drugs were classified into different groups based on WHO–ATC classification. The demographic data, clinical data, and utilization of different classes of drugs as well as individual drugs were analyzed.
Results:
A total of 325 consecutive patients were included for the analysis; 211 (65%) patients were males; 146 patients (45%) were above 55 years of age. Encephalopathy [63(19.38%)] and stroke [62(19%)] were the common central nervous system diagnoses. In a total of 1237 drugs, 68% of the drugs were prescribed by trade name. Midazolam (N05CD08) 142 (43.69%), morphine (N02AA01) 201 (61.84%), and atracurium (M03AC04) 82 (25.23%) were the most commonly used sedative, analgesic, and neuromuscular blocker, respectively. Phenytoin (N03AB02) 151 (46.46%) had maximum representation among antiepileptic agents.
Conclusions:
Utilization of drugs from multiple central nervous system drug classes was noticed. Rational use of drugs can be encouraged by prescription by brand name.
Keywords
Central nervous system
critically ill
drug utilization
Introduction
Neurologic disorders are prevalent among the critically ill patients in the intensive care unit (ICU), both as a primary disease as or as a complication of multiple organ dysfunction. Critically ill patients are at a high risk of developing neurologic disorders due to multiple organ failure, advancing age, prescription of psychoactive agents, and malnutrition.[1] Altered sensorium, raised intracranial pressure, cerebrovascular thrombosis, seizures, and bacterial meningitis are the common central nervous system (CNS) disorders noted among the critically ill.[1]
Critically ill patients, especially those with respiratory failure may require mechanical ventilation, which is uncomfortable because of pain and anxiety. Sedation and analgesia are essential components in the management of these intensive care patients in order to relieve the discomfort and anxiety caused by procedures, such as tracheal intubation, ventilation, suction, and also to minimize agitation and to provide appropriate sleep.[23] In addition, CNS drugs are also used to control seizures and treat delirium, depression, and psychotic symptoms among these critically ill patients.[4]
Drug therapy, in critically ill patients, is often complicated by the altered physiology, presence of multiorgan system failure, and multiple medications. Frequently changing disease processes and organ dysfunction result in changes in pharmacokinetic parameters of drugs used in them. Critical illnesses have shown to affect the absorption, distribution, protein binding, metabolism, elimination, and serum concentration of commonly used drugs. The alteration in the pharmacokinetic parameters leads to changes in the pharmacodynamic effects of these agents, resulting in either subtherapeutic, supratherapeutic, or toxic effects.[14] The use of multiple medications may further increase the risk of drug-related problems, such as adverse drug reactions, interactions, patient noncompliance with treatment, and medication errors. Hence, the appropriate management of these patients is a challenge for the treating physician.
The study of drug prescribing patterns helps to evaluate and suggest modifications in prescribing practices of physicians.[5] This practice ensures rational pharmacotherapy and assures quality medical care to the patients. In the developing countries, drug cost is a major concern for both health care providers and the beneficiaries, and therefore the rational use of drugs plays a pivotal role in cost minimization and optimal utilization of the available funds. The objective of the present study was to evaluate the utilization patterns of CNS drugs among the patients admitted to the medical ICU.
Materials and Methods
The study was carried out at a tertiary care superspecialty teaching hospital in southern part of the Indian subcontinent. The data were collected over a period of 12 months (October 2006 to September 2007). During the study period, all patients admitted to the medical ICU for more than 24 h and who received CNS drugs, were included as study sample. Patients who stayed in the ICU for less than 24 h and those admitted more than once in the ICU during the study period were not included in the study. The study was approved by the institutional ethics committee. The data were collected from the medication orders sheets filled by the physician. All the prescriptions were reviewed prospectively from patients admitted to ICU during the study period. The demographic data [age, gender, and outcome of the patient (improved, died)], clinical data (clinical diagnosis and associated comorbid conditions, length of ICU stay), and all drug prescription details (generic/trade name, route of administration, dose, frequency) were recorded. The data were collected by the first author.
Statistical analysis
The data were subjected to descriptive analysis using Microsoft Excel. The prescribed drugs were identified and placed into 6 classes using the WHO Anatomic Therapeutic Chemical classification system.[6] The total number of the different drugs administered to each patient and exposure rates for each drug class and individual drugs were analyzed and presented as number and percentage. Among the medications prescribed, those that were prescribed from the WHO essential drug list were noted.[7]
Results
The study results provide a detailed overview of the drug utilization pattern of CNS drugs among the patients admitted to medical ICU. During the study period a total of 902 patients were admitted, 325 patients (36%) received CNS drugs and were included as the study sample. The remaining 64% patients admitted to the ICU were not included because they did not receive CNS drugs. Among the 325 patients, male patients were 211 (65%) and female patients, 114 (35%). The majority of the patients were older than 55 years (146; 45%), 110 patients (34%) were between 35 and 55 years and 69 patients (21%) were younger than 35 years. The mean length of stay in the medical ICU was 6.22 ± 3.34 days. Among the 325 patients, 226 (69.53%) patients improved, of whom 30% had disabilities, such as neurologic deficits, hemiparesis, and behavioral abnormalities, 45 (13.84%) patients died, and the outcome of 54 patients was not known because 38 (11.69%) patient were discharged upon request and 16 patients (4.92%) got discharged against medical advice.
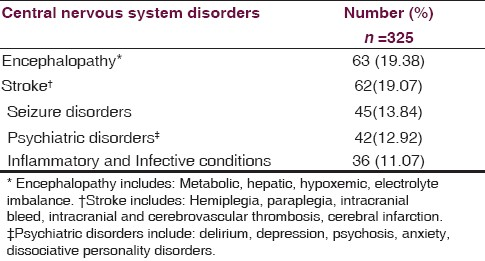
The common clinical diagnoses noticed among the patients in ICU were sepsis, acute renal failure, multiorgan dysfunction syndrome, acute respiratory distress syndrome, pneumonia, and lower respiratory tract infections. Among the clinical conditions involving the CNS, encephalopathy 63 (19.38%) and stroke 62 (19.07%) were the frequent CNS disorders observed. Patients with CNS infective conditions, degenerative disease, and structural abnormalities were fewer [Table 1].
Based on the WHO Anatomic therapeutic chemical classification, a total of 1237 drugs from ATC-N (drugs acting on nervous system) were used among 325 patients. It was observed that 68% of the CNS drugs were prescribed by trade name. Forty-two percent of drugs prescribed were from WHO essential drug list. The mean number of CNS drugs received in these patients was 5.22 ± 2.34 drugs. Various drug classes prescribed include sedatives, analgesics, neuromuscular blockers, antiepileptics, psychotropic agents, such as antipsychotic agents, antidepressants, and mood stabilizers.
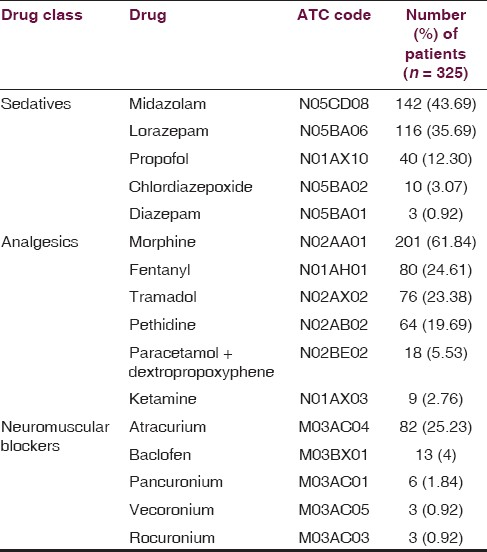
Sedative and analgesics were the frequently prescribed drug classes for patients on ventilators, and therefore they were analyzed. Midazolam (N05CD08) 142 (43.69%) and lorazepam (N05BA06) 116 (35.69%) were the most commonly used sedatives, whereas morphine (N02AA01) 201 (61.84%) was the most common analgesic prescribed. Among the neuromuscular blockers, atracurium (M03AC04) was the most common medication, being received by 82 (25.23%) out of the 325 patients [Table 2].
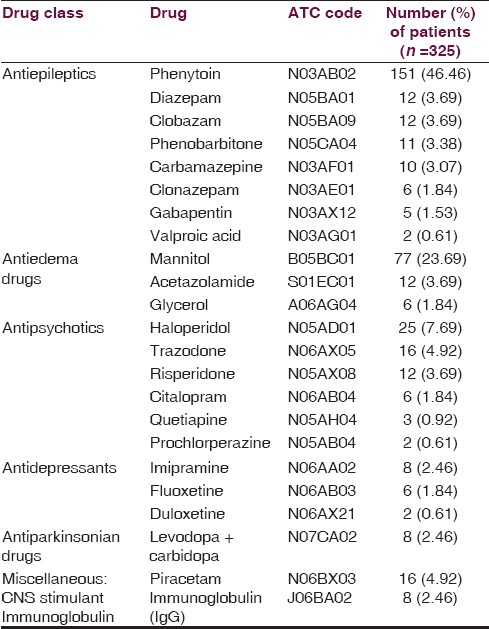
Among the other CNS drugs, phenytoin (N03AB02) 151 (46.46%) was the most commonly prescribed antiepileptic and haloperidol (haloperidol 25 (7.69%) most commonly used antipsychotic agent [Table 3].
During the ICU stay, the adverse effects associated with CNS drugs were ketamine-induced bradycardia, lithium-induced encephalopathy, and ataxia, risperidone-induced orofacial dyskinesia and seizures, sodium valproate-induced encephalopathy, and carbamazepine-induced syndrome of inappropriate antidiuretic hormone.
Discussion
The results of the present study give a detailed overview of the utilization patterns of CNS drugs among the seriously ill patients of medical ICU. It was observed that more male patients were admitted to the ICU in comparison to female patients. The common CNS conditions observed were encephalopathy (19.38%) secondary to electrolyte imbalance, hepatic cause, and metabolic and hypoxic etiologies followed by stroke. Factors associated with encephalopathy include primary cerebral disorders, such as stroke, trauma, and meningitis, or systemic derangements, including sepsis, organ failure, and exposure to pharmacologic agents and toxins. There is mounting evidence that cerebral dysfunction persists beyond the acute phase of critical illness resulting in impairments in cognitive ability, suggesting occult brain injury. Preventive and therapeutic interventions are cornerstones in the management of encephalopathy.
Of the 1237 drugs from ATC-N (drugs acting on nervous system) utilized among 325 patients, it was observed that 68% of the drugs were prescribed by brand name. Clinicians should practice generic prescription by which equally efficacious drugs could be given at a low cost and also encourage rational use of drugs.
Sedation and analgesia are important to ensure patient comfort from psychological and physical point of view, thus reducing stress which leads to profound changes in the fluid and electrolyte balance, mobilization of substrates from energy source, and neurohormonal milieu.[8] In the present study, morphine sulfate (61.84%) was the most commonly utilized analgesic followed by fentanyl (24.61%). This finding was similar to previous studies carried out by Soliman et al,[8] Biswal et al,[9] and Bobek et al.[10] Morphine is the principal sedative agent preferred in ICU due to its potency, improved patient ventilator synchrony, and availability of effective antagonist.[11]
Midazolam (43.69%), the most frequently used sedative followed by lorazepam (35.69%). Our findings were comparable with earlier reports from Europe,[8] India,[9] and United States.[10] Midazolam, due to its rapid onset of effects, faster redistribution and quicker elimination, is an appropriate choice for short-term sedation.[12] Lorazepam has an intermediate duration of action due to low lipid solubility; it is recommended for long-term maintenance of sedation in the chronically critically ill patients.[12]
Pancuronium was the most frequently utilized neuromuscular blocker in an earlier study[10] in ICU setup, while atracurium was preferred in our study; probably because atracurium follows Hofmann elimination, so can be used safely in patients with renal failure.[13]
Older intravenous antiepileptic agents, such as phenytoin (46.46%) were preferred in the present study. This finding was in concordance to an earlier study from India.[9] Phenytoin was used mainly for seizure prophylaxis and maintenance therapy. Phenytoin, due to its saturation kinetics, drug interactions, and adverse effects can be replaced by newer antiepileptic agents.[14] Studies carried out on the use of the newer agents, such as levetiracetam and lacosamide suggest that newer agents are better tolerated.[1516]
Stroke is associated with morbidity and mortality mainly due to raised intracranial pressure (ICP) and its consequences in the acute stage.[17] Osmotic agents (glycerol, mannitol) and diuretics are often used to reduce raised ICP.[1819] In the present study, 23.69% of the patients received mannitol. A previous report from India looking into the prescribing pattern of antiedema therapy in ICU showed that there was no uniformity among physicians in prescribing antiedema therapy.[20]
Delirium is one of the common psychiatric illness common in the ICU, occurring in 20%–80% of patients, with the highest proportions seen in mechanically ventilated patients.[21] Haloperidol was prescribed to 25 patients, whereas risperidone was prescribed to 12 patients. Although atypical antipsychotics are found to be equally efficacious and associated with lesser incidence of extrapyramidal effects, utilization of atypical antipsychotics are limited in the ICU, primarily due to fewer studies comparing them.[2223] Haloperidol, a high-potency neuroleptic, offers greater advantage due to additional sedative effect.[2223]
Depression, in ICU patients, results from the psychological toll of serious illness as well as the physiologic derangements caused by illnesses and treatments. The percentage of antidepressant prescriptions noticed in the study was 5%. Previous data suggest that establishing the diagnosis of depression in critically ill is often difficult.[24]
Although drug therapy is the most cost-effective method of minimizing mortality and morbidity in critically ill patients, drug therapy itself can be a major cause of increased cost, morbidity, and mortality in these patients.[25] The purpose of inpatient-based prescription audit has advantage of minimizing the “drop-outs” as patients had to purchase and take the prescribed drugs and limitation of the study included smaller sample size, study of only a single ICU for a specific 12-month time period and qualitative assessment of drug utilization was not performed. In conclusion, the utilization of drugs from multiple CNS drug classes was noticed and rational use of drugs can be encouraged by prescription by brand name.
We acknowledge all faculty and staff of the medical intensive care unit of St. John's Medical College for the valuable help and support in this study.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Oxford textbook of critical care. (1st ed). USA: Oxford University Press Publishers; 1999.
- [Google Scholar]
- Medications for analgesia and sedation in the intensive care unit: An overview. Crit Care. 2008;12(Suppl 3):S4.
- [Google Scholar]
- Applied Pharmacokinetics in the Intensive Care Unit. In: Irwin RS, Cerra FB, Rippe JM, eds. Irwin and Rippe's Intensive Care Medicine (4th ed.). Philadelphia: Lippincott-Raven Publishers; 1999. p. :1413.
- [Google Scholar]
- Drug utilization studies: Methods and uses European Series No. 45. Copenhagen: WHO Regional Publications; 1993.
- [Google Scholar]
- WHO Collaborating Centre for Drug Statistics Methodology. 2005. Anatomictherapeutic-chemical classification of drugs (ATC) Classification index. Oslo: Norway. Available from: http://www.whocc.no/atcddd/
- [Google Scholar]
- WHO Model Lists of Essential Medicines. Available from: http://www.who.int/medicines/publications/essentialmedicines/en/
- [Google Scholar]
- Sedative and analgesic practice in the intensive care unit: The results of a European survey. Br J Anaesth. 2001;87:186-92.
- [Google Scholar]
- Drug utilization pattern in the intensive care unit of a tertiary care hospital. J Clin Pharmacol. 2006;46:945-51.
- [Google Scholar]
- Utilization patterns, relative costs, and length of stay following adoption of MICU sedation guidelines. Formulary. 2001;36:664-73.
- [Google Scholar]
- Guidelines for Sedation and Analgesia during Mechanical Ventilation General Overview. J Trauma. 2007;63:945-50.
- [Google Scholar]
- Agents Acting at the Neuromuscular Junction and Autonomic Ganglia. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman's The Pharmacological Basis of Therapeutics (11th ed). New York: The McGraw-Hill Companies; 2006.
- [Google Scholar]
- Pharmacological management of seizures and status epilepticus in critically ill patients. J Pharm Pract. 2010;23:441-54.
- [Google Scholar]
- Intravenous levetiracetam as treatment for status epilepticus. J Neurol. 2009;256:1634-42.
- [Google Scholar]
- Guidelines for the management of severe traumatic brain injury. XIII. Antiseizure prophylaxis. J Neurotrauma. 2007;24(Suppl 1):S83-6.
- [Google Scholar]
- Treatment of acute cerebral haemorrhage with intravenous glycerol: A double blind placebo-controlled randomized trial. Stroke. 1992;23:967-71.
- [Google Scholar]
- Guidelines for the management of spontaneous intracerebral haemorrhage a statement for health care professional from a special writing group of stroke council, American Heart Association. Stroke. 1999;30:905-15.
- [Google Scholar]
- Indications for early aspirin use in acute ischemic stroke: A combined analysis of 40000 randomized patients from the Chinese acute stroke trial and the international stroke trial. On behalf of the CAST and IST collaborative groups. Stroke. 2000;31:1240-9.
- [Google Scholar]
- Prescribing pattern of antiedema therapy in stroke by neurologists and general physicians. Neurol India. 2004;52:191-3.
- [Google Scholar]
- Clearing up the confusion: The results of two pilot studies of antipsychotics for ICU delirium. Crit Care. 2010;14:316.
- [Google Scholar]
- Feasibility, efficacy, and safety of antipsychotics for intensive care unit delirium: The MIND randomized, placebo-controlled trial. Crit Care Med. 2010;38:428-37.
- [Google Scholar]
- Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo controlled pilot study. Crit Care Med. 2010;38:419-27.
- [Google Scholar]
- The characteristics of patients given antidepressants while recovering from critical illness. Br J Anaesth. 2000;84(5):666.
- [Google Scholar]
- Critical care pharmacotherapy: Issues and approaches. Curr Opin Crit Care. 2000;6:299-303.
- [Google Scholar]






