Translate this page into:
Symptoms of Neurotoxicity among Carpenters Living in Rural Ecuador: A Population-based Study (The Atahualpa Project)
Address for correspondence: Dr. Oscar H. Del Brutto, Air Center 3542, P.O. Box: 522970, Miami, FL, USA. E-mail: oscardelbrutto@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
There is no information on the prevalence of symptoms related to neurotoxicity among carpenters working in underserved populations. To assess the magnitude of the problem, we conducted a population-based study in Atahualpa, a rural Ecuadorian village, where most men work as carpenters under poor safety conditions.
Methods:
All men aged 40–75 years living in Atahualpa were identified during a door-to-door survey and evaluated with a general demographic questionnaire, the Q16 questionnaire, the depression axis of the Depression Anxiety Stress Scale-21, and the Montreal Cognitive Assessment (MoCA).
Results:
Among 230 participants, 63% were carpenters. Seventy participants (30%) had a positive Q16 questionnaire (≥6 points), which suggested neurotoxicity. In a logistic regression model adjusted for age, education, alcohol intake, symptoms of depression, and MoCA score, the proportion of Q16 positive persons was 39.1% for carpenters and 15.9% for noncarpenters (odds ratio: 3.53, 95% confidence interval: 1.75–7.15, P < 0.0001). In a generalized linear model, adjusted mean scores in the Q16 questionnaire were 4.9 for carpenters and 3.6 for noncarpenters (β: 1.285, standard error: 0.347, P < 0.0001). There was no correlation between scores in the Q16 questionnaire and the MoCA (Pearson correlation coefficient = −0.02), and the only significant covariate in the multivariate linear model was age, with every 10 years of age difference contributing 0.64 points in the Q16 questionnaire.
Conclusion:
This study shows a high prevalence of symptoms associated with neurotoxicity among carpenters after adjusting for a number of confounders. Long-term exposure to toxic solvents is the most likely explanation to this finding.
Keywords
Atahualpa
carpenters
Ecuador
neurotoxicity
population-based studies
Q16 questionnaire
INTRODUCTION
Chronic exposure to organic solvents has been associated with adverse events ranging from skin reactions to a toxic encephalopathy. Chronic solvent poisoning is an occupational disease affecting persons who are in contact with paints, cleaning substances, pesticides, and liquids used for photographic processing, among others.[1] Carpenters are at increased risk for developing complications related to frequent exposure to varnish, lacquer, thinner, and other chemicals.[2] However, only a few studies have described neurological manifestations associated with chronic solvent exposure in carpenters, and many have considered them as a “minimally exposed group,” being at a lesser risk of developing adverse effects than painters or construction workers.[3] Most of these studies came from industrialized countries, where working conditions are different than in rural settings.
During a door-to-door survey performed by our group for the assessment of neurological disorders in a rural village of Ecuador, we noticed that most men work as carpenters. These individuals have been working for years under poor safety conditions, being in daily contact with a number of organic solvents. In two preliminary reports, we reported an association between chronic sawdust exposure and respiratory symptoms and a probably increased prevalence of Parkinson's disease among Atahualpa carpenters.[45] Here, we aimed to assess the occurrence of symptoms related to neurotoxicity in this population.
METHODS
As detailed elsewhere, the Atahualpa Project is a population-based cohort study, designed to reduce the burden of neurological and cardiovascular diseases in rural Ecuador.[6] The Institutional Review Board of Hospital-Clínica Kennedy, Guayaquil, Ecuador (FWA 00006867) approved the protocol and the informed consent form. Trained field personnel performed a door-to-door survey to identify all men aged 40–75 years residing in Atahualpa. Persons who declining to consent and those unable to complete the questionnaires were not included in the study. Field instruments included a general demographic questionnaire, the Q16 questionnaire, the Montreal Cognitive Assessment (MoCA), and the depression axis of the Depression Anxiety Stress Scale-21 (DASS-21).
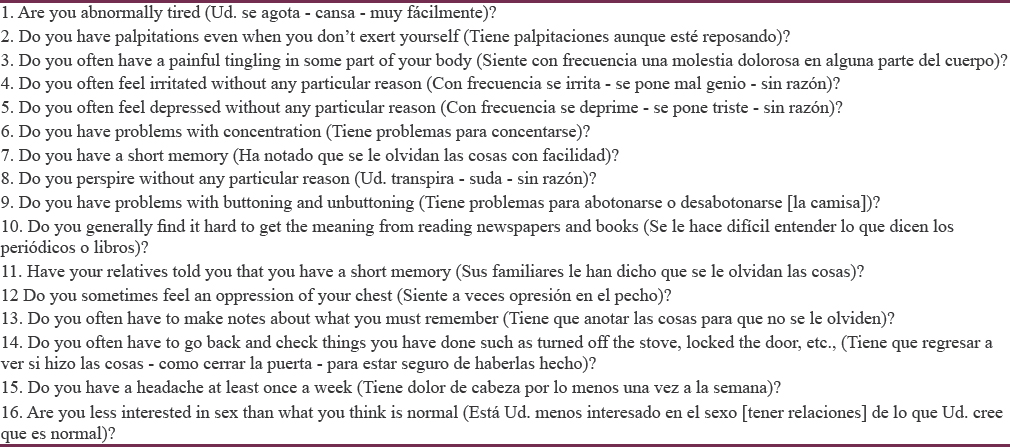
The Q16 questionnaire has been widely used for assessing symptoms suggestive of neurotoxicity.[7] It consists of 16 questions, and it is interpreted as positive if the person responds as affirmative to ≥6 questions; four of the questions inquire about memory complaints and the other 12 about other kinds of neurological and systemic symptoms [Table 1].
The MoCA assesses different cognitive domains including attention and concentration, executive functions, memory, language, visual-constructional skills, conceptual thinking, calculations, and orientation; maximum score is 30 points, with an additional point given to persons with ≤12 years of education.[8] We did not use a cutoff score for defining an abnormal MoCA, but the continuous score to avoid problems related to poor reliability of specific cutoffs in less educated populations.[9]
To recognize symptoms of depression, participants were evaluated with the depression axis of the DASS-21, a reliable field instrument that measures dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia, with seven questions that are rated on a four-point Likert scale ranging from 0 (not at all) to 3 (almost always) with a maximum total score of 21 and a diagnosis of depression in persons who have ≥5 points.[10]
As Atahualpa residents speak Spanish, we used validated Spanish versions of the MoCA and the depression axis of the DASS-21 previously used in South American communities including Atahualpa.[11] Bilingual physicians from our group independently translated the Q16 questionnaire from its original English version to Spanish, and disagreements in translation were resolved through discussion and consensus. Then, the Spanish version of the Q16 questionnaire was culturally adapted with the aid of community leaders and tested in a random sample of the population before the survey.
Descriptive statistics were presented as means with standard deviations for continuous variables and as percentages for categorical variables. A logistic regression model was used to study the relationship between job (dichotomized in carpenters and noncarpenters) and positivity in the Q16 questionnaire, after adjusting for age, education, alcohol intake, depression, and MoCA score. A generalized linear model assessed the relationship between job and mean score of the Q16 questionnaire, after adjusting for the same variables. P < 0.05 is considered statistically significant. Statistical analyses were carried out using STATA version 14 (STATA College Station, TX, USA).
RESULTS
The door-to-door survey identified 245 men aged 40–75 years. Of these, nine declined to participate, and six could not perform the Q16 or the MoCA due to aphasia or severe visual or hearing impairment. The 230 enrolled persons had a mean age of 56.5 ± 9.4 years, a mean level of education of 7.9 ± 3.3 years, 146 (63%) were carpenters, 108 (47%) reported alcohol consumption ≥50 g/day, and 14 (6%) reported depressive symptoms according to the DASS-21. Mean total scores were 4.5 ± 2.6 for the Q16 questionnaire and 21.7 ± 3.9 for the MoCA, with no correlation between them (Pearson correlation coefficient = −0.02). A total of seventy persons (30%) had a positive Q16 questionnaire (≥6 points).
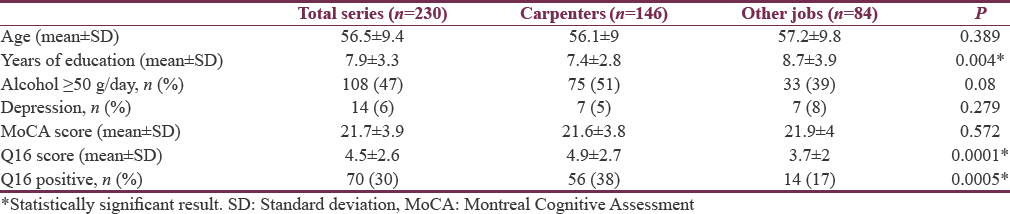
Table 2 describes characteristics of participants according to their job. Carpenters were less educated and had a nonsignificant tendency for drinking more alcohol than noncarpenters. There were no differences in age, in the prevalence of depressive symptoms or in the mean MoCA score across both groups. A positive Q16 questionnaire was recorded in 38% of carpenters and in 17% of noncarpenters (P = 0.0005). In addition, the mean score in the Q16 questionnaire was significantly higher among carpenters (P < 0.0001).
In a logistic regression model, after adjusting for age, education, alcohol intake, depression, and MoCA score, the proportion of Q16 positive persons was 39.1% (95% confidence interval [CI]: 31.2%–46.9%) for carpenters and 15.9% (95% CI: 8.2%–23.6%) for noncarpenters (odds ratio: 3.53, 95% CI: 1.75–7.15, P < 0.0001). The only other significant variable in a multivariate model was age, with older persons being more likely to have a positive Q16 questionnaire independently of the other variables (P = 0.013).
In a generalized linear model, after adjusting for the same variables than in the previous model, mean scores in the Q16 questionnaire were 4.9 (95% CI: 4.5–5.3) for carpenters and 3.6 (95% CI: 3.1–4.2) for noncarpenters (β: 1.285, standard error: 0.347, P < 0.0001). Again, the only other significant variable in the multivariate linear model was age (P = 0.002), with every 10 years of age difference contributing 0.64 points in the Q16 questionnaire.
DISCUSSION
This study shows a significant increase in the prevalence of symptoms associated with neurotoxicity as well as a higher mean score in the Q16 questionnaire among carpenters living in rural Ecuador. From the many confounders investigated in our study, only age was independently associated with a poorer score and positivity in the Q16 questionnaire. While this could be related to age itself, it is possible that cumulative exposure to solvents has accounted – at least in part – for this association.[7]
We found no correlation between scores in the Q16 questionnaire and the MoCA in our participants, suggesting that symptoms of neurotoxicity do not correlate with poor performance in cognitive tests. This is an expected finding since only 4 of the 16 questions of the Q16 questionnaire inquire about cognitive function.[7] It has been suggested that other field instrument, the EuroQuest, may be more reliable than the Q16 questionnaire for screening persons with suspected neurotoxicity and memory complaints.[12] However, this test consists of 59 items and may be less feasible to perform in population-based surveys conducted in underserved populations.
Studies from industrialized nations have shown that most carpenters – with the possible exception of lacquerers – are not heavily exposed to toxic solvents. However, there is no information on neurotoxicity in carpenters living in underserved populations. Atahualpa carpenters are not specialized in a particular topic of carpentry. Hence, most of them have been working – at any point of their lives – as lacquerers, cabinet or furniture makers, sawyers, or polishers. This, together with the rudimentary facilities of most carpentry workshops and the lack of protective measures (glasses and masks), suggests that most of these persons have been exposed to the many toxic solvents that are used in the elaboration of furniture.
The major strengths of this study include its door-to-door design as well as the homogeneous characteristics of residents regarding race/ethnicity and socioeconomic status, together with the criteria used for the evaluation of potential confounders and the uniqueness of Atahualpa in that most men work as carpenters. A potential limitation is that biomarkers of solvent exposure across carpenters and noncarpenters were not evaluated. However, the high odds for having a positive Q16 questionnaire and the difference in mean values of this field instrument across carpenters and noncarpenters make it unlikely that unmeasured confounders accounted for our results.
CONCLUSION
This study shows a high prevalence of symptoms associated with neurotoxicity among artisans carpenters living in rural Ecuador. Long-term exposure to toxic solvents is the most likely explanation to this finding.
Financial support and sponsorship
This study was partially supported by Universidad Espíritu Santo – Ecuador, Guayaquil, Ecuador.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Occupational exposure to organic solvents and long-term nervous system damage detectable by brain imaging, neurophysiology or histopathology. Food Chem Toxicol. 2003;41:153-87.
- [Google Scholar]
- Health complaints and work conditions among lacquerers in the Danish furniture industry. Scand J Soc Med. 1979;7:97-104.
- [Google Scholar]
- Solvent-related health effects among construction painters with decreasing exposure. Am J Ind Med. 2004;46:627-36.
- [Google Scholar]
- Sawdust in carpentry workshops in rural areas of developing countries. J Epidemiol Community Health. 2013;67:973.
- [Google Scholar]
- Prevalence of Parkinson's disease in a rural village of coastal Ecuador. A two-phase door-to-door survey. Acta Neurol Belg. 2013;113:253-6.
- [Google Scholar]
- Atahualpa Project Investigators. Door-to-door survey of cardiovascular health, stroke, and ischemic heart disease in rural coastal Ecuador – The Atahualpa Project: Methodology and operational definitions. Int J Stroke. 2014;9:367-71.
- [Google Scholar]
- Evaluation of the Q16 questionnaire on neurotoxic symptoms and a review of its use. Occup Environ Med. 1997;54:343-50.
- [Google Scholar]
- The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695-9.
- [Google Scholar]
- Applicability of the MoCA-S test in populations with little education in Colombia. Int J Geriatr Psychiatry. 2013;28:813-20.
- [Google Scholar]
- The Depression Anxiety Stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. J Clin Psychol. 2012;68:1322-38.
- [Google Scholar]
- Edentulism associates with worse cognitive performance in community-dwelling elders in rural Ecuador: Results of the Atahualpa project. J Community Health. 2014;39:1097-100.
- [Google Scholar]
- Symptoms of chronic solvent encephalopathy: Euroquest questionnaire study. Neurotoxicology. 2009;30:1187-94.
- [Google Scholar]






