Translate this page into:
Symptomatic Thoracic Intramedullary Arachnoid Cyst: “A Rare Entity” Report of Two Cases with Short Review of Literature
Address for correspondence: Dr. Naresh Panwar, Department of Neurosurgery, SMS Medical College, Jaipur - 302 004, Rajasthan, India. E-mail: panwaralice2005@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spinal arachnoid cysts are uncommon benign lesions of spine axis and most commonly present as compressive myelopathy. Intramedullary arachnoid cyst is uncommonly seen, hence, not much discussed in literature. Due to rarity of this entity, many questions are yet to be answered and should be addressed properly, particularly related to etiopathogenesis, accustomed course, behavior, differential diagnosis, and the best treatment modality. We report the clinicopathological profile of thoracic intramedullary arachnoid cysts in two adult patients, and present a detailed review of available literature on the spinal intramedullary arachnoid cyst. Most of the literature concerning with intramedullary arachnoid cysts are in the form of case reports from pediatrics population. As far to the best of our knowledge, only a few cases excluding our two were found in both pediatrics and adult population.
Keywords
Dorsal spine
intramedullary arachnoid cysts
surgical decompression
INTRODUCTION
Arachnoid cysts of spinal cord are a rare entity, and often found as an asymptomatic incidental finding during examination performed for other causes. Most of the arachnoid cysts are located in extradural compartment, though it can be intradural and further subclassified as either extramedullary or intramedullary. On the basis of findings of surgical examinations, radiological features and histopathological review of 22 cases, first attempt to classify the arachnoid cysts in the spine have been done by Nabors et al. in 1986[1] as: Type 1-extradural cysts without spinal nerve roots; Type 2-extradural cysts with spinal nerve root fibers; Type 3-intradural cysts.
Herniation through dural defect is considered the etiopathogenesis of extradural arachnoid cyst, while the intradural cysts are thought to arise from proliferation of arachnoid trabeculae. The mechanisms responsible for pathological development of these intramedullary cysts is still unclear with various hypothesis has been purposed in the past from congenital, traumatic, and inflammatory causes.[2345]
Most of the literature concerning with intramedullary arachnoid cyst is in the form of case reports from the pediatric population. Here, we are reporting clinicopathological characteristics along with review of relevant literature of two cases of intramedullary arachnoid cyst in adult age group.
CASE REPORTS
Case 1
This 45-year-old female presented with dull mid-backache for 6-month duration and paresthesias in both lower limbs for duration of 3 months. She completely denies any complaints related to bowel and bladder disturbances. Examination revealed normal bilateral upper limbs with spastic weakness (Modified Ashworth Scale-1+) of both lower limbs with power of 4-/5 in all major groups of muscles, and she was able to walk with minimal support. Lower limb deep tendon reflexes were brisk with bilateral extensor plantar response. Sensory examination showed decreased sensations to pinprick, touch, and temperature below D12 with spared sacral sensations.
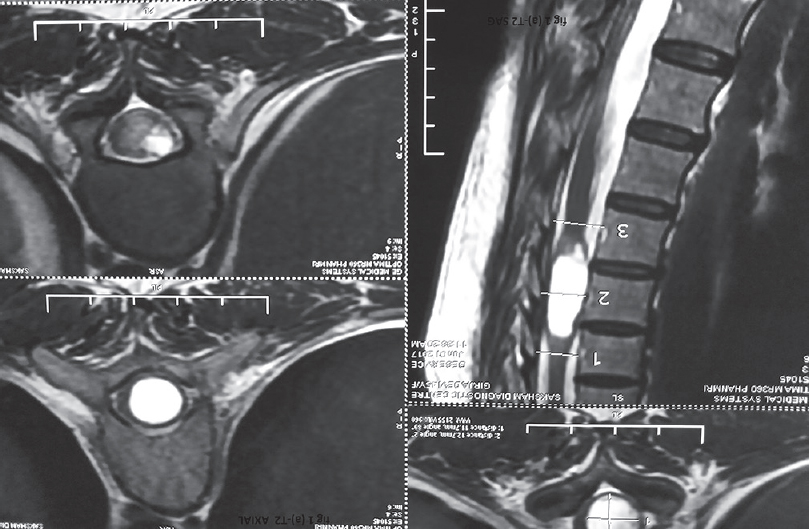
Magnetic resonance imaging (MRI) of the spine showed an intra-axial lesion, hypointense on T1 and hyperintense on T2-weighted sequences, respectively [Figure 1a and b]. Lesion was seems to be expanding the cord and extending from D9 to D11 region with no contrast enhancement. There was no evidence of any communication with the central canal.
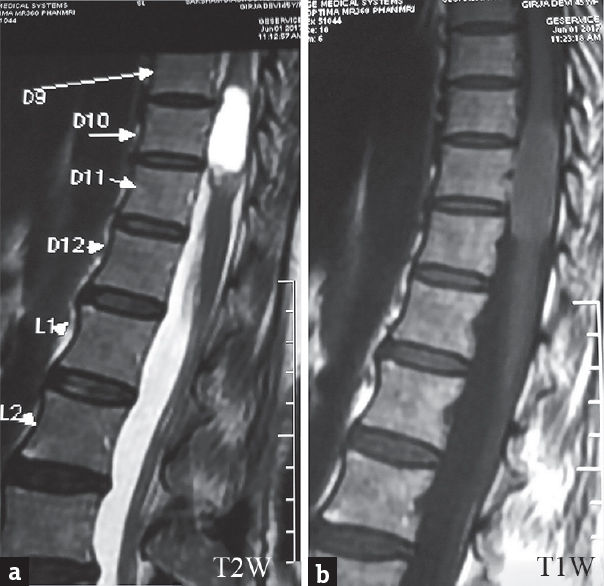
- (a and b) Sagittal T1- and T2-weighted images showed hypointense and well-defined hyperintense lesion at D9–D10 level, respectively
The patient underwent D8–D12 laminectomy. Following durotomy, the cord was found to be protruding. Midline myelotomy performed and cyst was tapped [Figure 2]. There was clear fluid such as cerebrospinal fluid (CSF). Fluid sent for routine biochemistry, a thin membrane, was found and was biopsied and sent for histochemical analysis. There was no communication of the cyst to the central canal. A watertight dural closure was performed. Histopathological examination revealed a cystic lining resting on fibrocartilaginous tissue with irregularly shaped cells, and a thin cystic lining possibility of arachnoid cyst suggested by our pathologist and for further confirmation marker study performed [Figure 3a and b]. Immunohistochemistry carried out on formalin fixed paraffin embedded section; tumor cells were negative for S100 [Figure 4a], carcinoembryonic antigen [Figure 4b], Glial fibrillary acidic protein [Figure 4d] and P53 [Figure 4e]. Cells were strongly positive for epithelial membrane antigen the antibody, and their clones used for detection were belonged to Biogenix and biocare SIGMA USA. Immunomarkers study confirmed the diagnosis arachnoid cyst [Figure 4c].
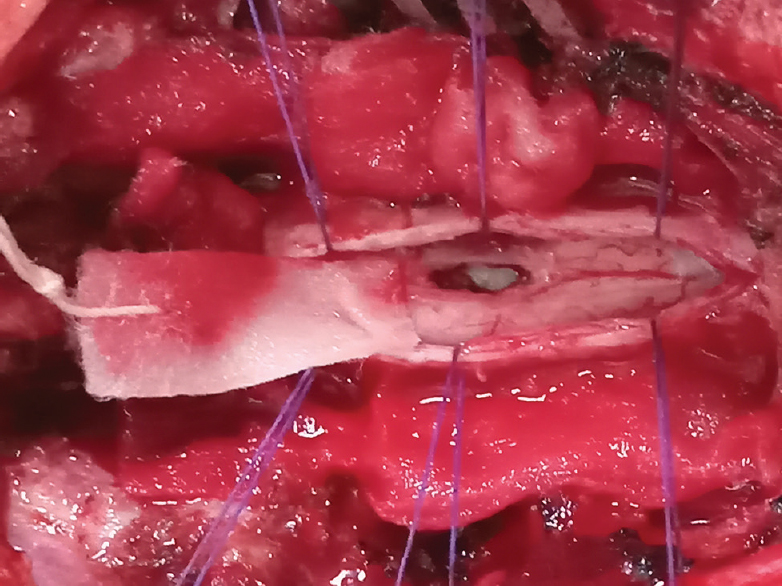
- Intra-operative image showing dorsomedian myelotomy with aspiration of arachnoid cyst
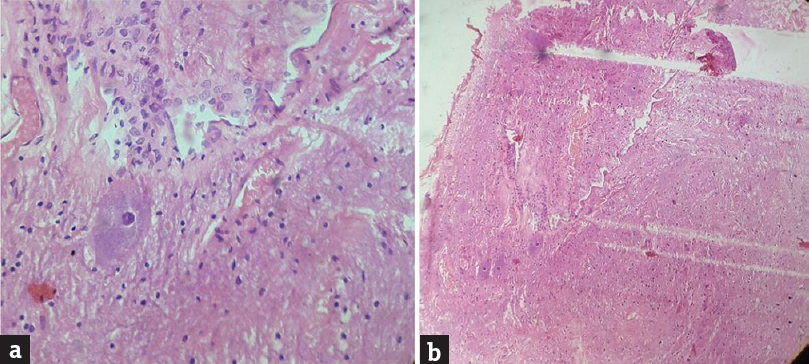
- (a and b) Histopathology of intramedullary cyst wall. Cuboidal cystic lining resting on fibrocartilagenous tissue (stroma) with irregularly shaped cells (H and E, ×5 and ×10 respectively)
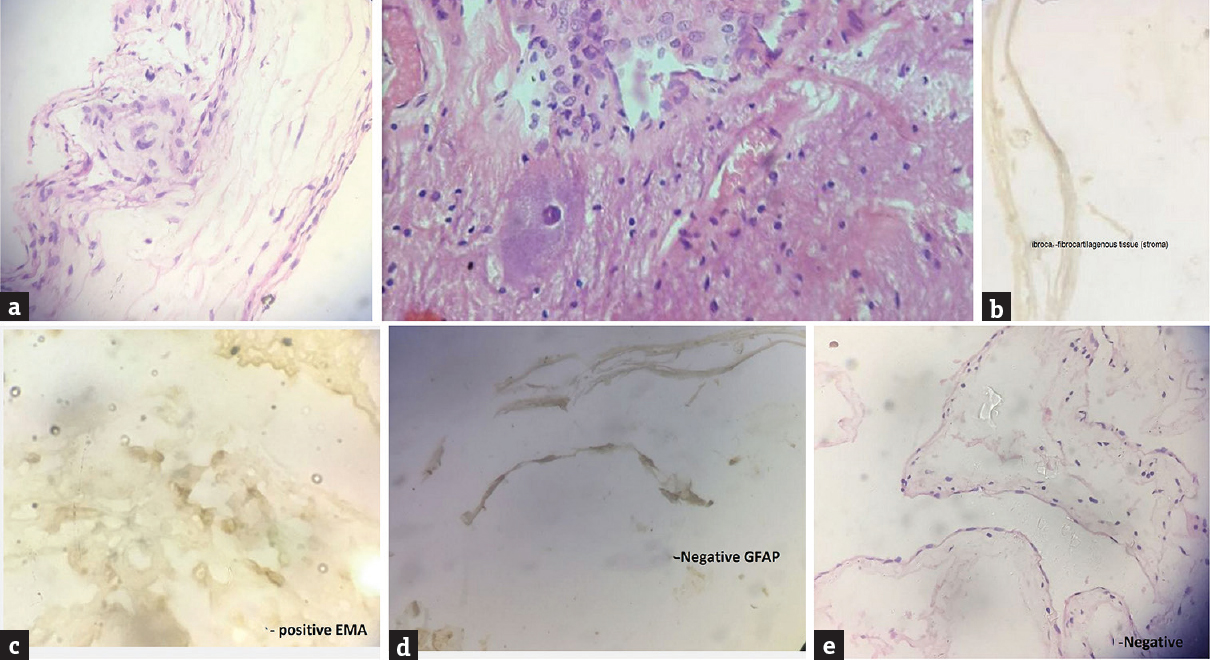
- Immunohistochemistry of intramedullary cyst. (c) The lining epithelial cells express epithelial membrane antigen. (a-e) Negative control slide for S100, P53, carcinoembryonic antigen, glial fibrillary acidic protein does not express target antigen. (immunoperoxidase against epithelial membrane antigen are from biogenix, ×10)
Case 2
Another case, a 40-Year-old male, presented with 2-year history of low backache that had worsen for the last 3 month and at the time of admission he also complaints of numbness in bilateral lower limb. Examination showed mild weakness in distal group of muscles with increased spasticity. Sensory examination revealed decreased sensation below D11 level.
For this reason, the patient had undergone a spinal MRI revealing the presence of an intramedullary, nonenhancing CSF intensity cystic lesion at the conus medullaris [Figure 5a and b]. He underwent D9–D11 laminectomy, dorsomedian myelotomy, and cyst decompression. The cyst contained clear fluid. Safe, guarded, and incomplete removal of cyst wall was done, as it was adherent to the neural tissue. Histopathological examination revealed arachnoid cyst.
- (a and b) Magnetic resonance imaging of the dorsal spine. Sagittal T2-weighted images depicting well-defined, hyperintense lesion at D11–D12 with no perilesional signal changes, axial T2-weighted images shows intramedullary which is hyperintense and expanded cord seen
Both of the patients regularly followed in our outpatient department (outdoor) for approximately 11–12 month and detailed examination done by one of us. After few days of surgery, the patient got relieved from dysesthetic pain and spasticity. With due course of time, she regained muscle strength. Second case become neurologically normal 3-month postsurgery, and nowadays, he occasionally complaints of backache.
Follow-up MRI scan done after 11 month which showed a cystic mass hypointense on T1 and hyperintense on T2 of size 27 mm × 6 mm suggestive of recurrence [Figure 6a and b].
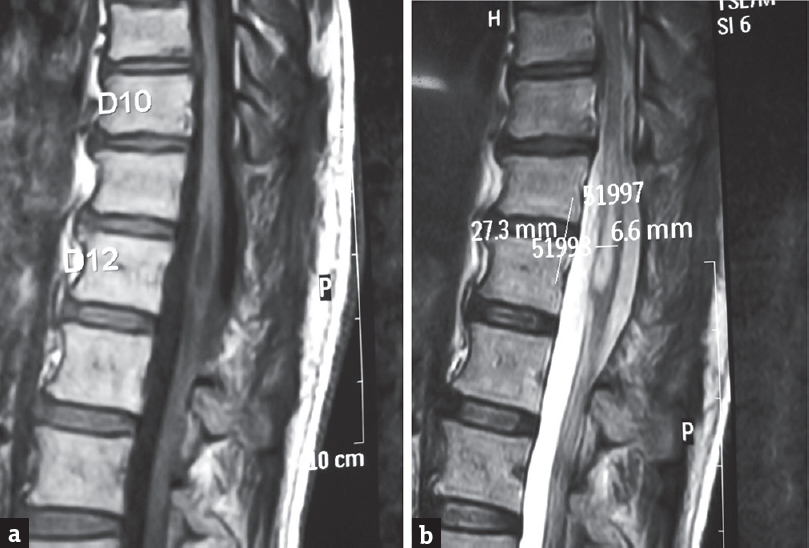
- Follow-up magnetic resonance imaging scan done after 11 month showed a cystic mass hypointense on T1 and hyperintense on T2 of size 27 mm × 6 mm suggestive of recurrence
Review of literature
Spinal intramedullary arachnoid cyst is one of the extremely rare lesions and has been sparsely reported in literature. They are usually asymptomatic but become symptomatic once the cyst exerts mass effect on the overlying cord and nearby nerve roots. The most common presenting initial symptom is backache and ultimately ends to gradually progressive myelopathy, because of continuous enlargement of the cyst. Close differential diagnosis of intramedullary arachnoid cysts includes neuroepithelial cyst, focal syrinx, cystic teratoma, cystic ependymoma, and ventriculus terminalis (VT). The characteristic feature of the VT in MRI is a cystic lesion of the distal central spinal cord canal without cord signal abnormality. Sometime, it is difficult to differentiate on imaging arachnoid cyst from ventriculs terminalis, and histopathological confirmation is required (lined by ependymal cell); however, VT has been described in newborn and pediatrics. VT is rare pathology in adult population and so far only few case reported.[5]
The origin, etiopathogenesis, and course of spinal intramedullary arachnoid cyst is still debatable and not clear. Misplaced cellular remnants during embryogenesis as a possible cause of intramedullary arachnoid were postulated by Hyndman and Gerber.[6] Fortuna and Mercuri[7] postulated the hypothesis that trapped arachnoid granulation at various locations including intramedullary is a causative factor in CSF production and accumulation, hence, cyst formation. This view was also supported by Goyal et al.[8]
An abnormal anatomical communication between subarachnoid space and cyst acting as a one-way valve-like mechanism for expansion of the cyst is also advocated.[9]
In the support of congenital cause of intramedullary arachnoid cyst Voss[10] and Rabb et al.[11] had described arachnoid cysts in relation with some developmental anomalies of spinal cord. Currently, no evidence available for the genetic predisposition of arachnoid cyst, however, report on familial spinal intradural arachnoid cysts[12] raises a concern and may merit further study.
In context to behavior or growth pattern of intramedullary arachnoid cysts, past purposed theories and case reports have shown a slow growth over time along with sudden neurological deterioration.
The available literature suggests a benign course and excellent recovery in spite of partial excision. There is no report on recurrence even with inadequate excision, which suggests that a free communication between cyst and subarachnoid space is enough for required decompression. However, long terms follow-up and MRI surveillance are not available for previously reported cases. Unfortunately, recurrence occurred in one of our patient after 11 month, which came to know after radiological evaluation. We purposed that either incomplete excision of cyst wall or a unnoticed ventral subarachnoid channel was culprit in this case.
The first case of intramedullary arachnoid cyst was reported by Aithala et al.[13] in a child, who went to dorsomedian myelotomy and got rapid and complete recovery within first week. Since then, to the best of author's knowledge, eight cases have been reported in pediatric population, and upper dorsal is the most common site reported for arachnoid cyst in pediatric age group [Table 1]. The probable embryonic malformations can be speculated as an etiological factor, no sex predilection found and all patients undergoes for myelotomy and drainage of cyst with or without fenestration. Final outcome in all patients was satisfactory, promising, and almost complete recovery. Follow-up was done from 5 days to 24 months, and we are fortunate enough that, no cyst recurrence/treatment failure reported till date worldwide.
| Authors and year | Age/Sex | Clinical presentations | Cyst location | Outcome | Follow-up |
|---|---|---|---|---|---|
| Aithala et al. 1999.[13] | 7 Yrs/M | Progressive Paraparesis | D4 | Rapid And Complete Recovery | 5 Days |
| Sharma et al. 2004.[3] | 10Yrs/F | Progressive Quadrapersis | C4-D2 | Rapid And Good Recover | 1 Month |
| Sharma et al. 2005.[4] | 4 Yrs/F | All Four Limb Weakness | C4-C6 | Complete Recovery | 17 Month |
| Ghannane et al. 2007[14] | 4 &8 Yrs | Progressive Para paresis | D 3-4 (Both Patients) | Complete Recovery | N/A |
| Guzel et al. 2007.[2] | 7 Yrs/F | Quadrapersis | C2-C4 | Rapid And Complete Recovery | 24 Month |
| Lmejjati et al.[15] | 12 Yrs/M | Progressive Paraparesis | D3-D4 | Rapid And Complete Recovery | 4 Month |
| Medved et al. 2009.[16] | 18 Month/M | Progressive Paraparesis, Constipation | D5-D6 | Complete Recovery | 1 Month |
| Kataria et al. 2012.[17] | 9 Years/F | Progressive Neurological Deficits | D-L | Complete Recovery | 1-6 Month |
The first case of intramedullary arachnoid cyst in adult was reported by Goyal et al.[8] in 2002. To the best of our knowledge, so far, 8 cases have been reported [Table 2]. As seen from the published data, it is evident that the intramedullary variant of arachnoids cysts is exclusively reported in dorsal cord in adult age group. As contrary to pediatric population, there is female sex predisposition. The surgical treatment of the symptomatic intramedullary arachnoid cyst in majority of cases includes dorsomedian myelotomy, with drainage of cyst and removal of the cyst wall as much as possible with avoiding of neurological deficit, where's Gezici and Ergün[18] preferred dorsal root entry zone myelotomy. In the majority of the cases, the cyst wall is found to be densely adhering to nearby glial tissue, and most of the time it is very difficult to excise it completely, but fortunately, no recurrence is reported till the date. Fenestration of the cyst with or without shunting to the subarachnoid space is another available treatment modality. Although surgery is the preferred approach in fact available one, a recent case reported by Fonseca and Ratilal[19] advocate “wait and scan” approach as a good therapeutic choice if patient is asymptomatic or mildly symptomatic.
| Authors and year | Age/sex | Clinical presentations | Cyst location | Outcome | Follow up |
|---|---|---|---|---|---|
| Goyal et al., 2002[8] | 63 years/female | progressive paraparesis, and bladder dysfunction | D9–D12 | Rapid and good recovery | 3 month |
| Gezici and Ergün 2008[18] | 35 years/male | B/L lower limb weakness | D5–D6 | Good recovery, ambulatory with little difficulty | 3 years |
| Diyora et al., 2010[20] | 45 years/male | Progressive neurological deficits | D4–D5 | Gradual but Complete recovery | 6 week |
| Kataria et al., 2012[17] | 40 years/female | Progressive neurological deficits | D–L | Complete recovery | 1-6 month |
| Novegno et al., 2014[21] | 31 years/female | Progressive paraparesis with bladder dysfunction | D11–D12 | Rapid and complete recovery | 24 month |
| Ranjan et al., 2014[22] | 40 years/female | Paraplegia with bladder dysfunction | D11–D12 | Rapid and Complete recovery (both motor and bladder) | 50 month |
| Alugolu et al., 2016[23] | 51 years/female | B/L lower limb weakness | D9–D11 | Sensory recovery | 1 year |
| Fonseca and Ratilal 2017[19] | 49 years/female | Progressive cervical pain with episodic B/L distal paresthesia | C6–C7 | Conservative | 5 years |
| Present study and 2017 | 40 years/male and 48 years/female |
Back ache and paresthesia | D9–D11 | Pain relieved completely | 1-2 month |
B/L: Bilateral, N/A: Not available
We report here two cases of intramedullary cyst, and both of them underwent dorsomedian myelotomy with cyst decompression; postoperatively, they recovered very well. We discuss imaging, histopathology and immune histochemistry characteristics of this lesion. Although it is very rare entity, we thought spinal intramedullary arachnoid cyst should be considered and kept as a differential diagnosis of intramedullary cystic lesion even in adult patients. More importantly, these lesions should undergo for surgical treatment as they afford very good clinical results, excellent prognosis and almost no recurrence. It's time to provide focused attention on their occurrences in asymptomatic patient. However, the rarity of this instance makes it very difficult to conduct case series, retrospective, and prospective studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988;68:366-77.
- [Google Scholar]
- Unusual presentation of cervical spinal intramedullary arachnoid cyst in childhood: Case report and review of the literature. Pediatr Neurosurg. 2007;43:50-3.
- [Google Scholar]
- Spinal intramedullary arachnoid cyst in a 4-year-old girl: A rare cause of treatable acute quadriparesis: Case report. J Neurosurg. 2005;102:403-6.
- [Google Scholar]
- Cystic lesion of the ventriculus terminalis: Proposal for a new clinical classification. J Neurosurg Spine. 2008;8:163-8.
- [Google Scholar]
- Spinal extradural cysts, congenital and acquired; report of cases. J Neurosurg. 1946;3:474-86.
- [Google Scholar]
- Spinal arachnoid cyst without neural tube defect. Childs Nerv Syst. 2001;17:179-81.
- [Google Scholar]
- Rückenmarkskompression durch eine intradurale Cyste. Langenbecks Arch Surg. 1937;248:341-5.
- [Google Scholar]
- Spinal arachnoid cysts in the pediatric age group: An association with neural tube defects. J Neurosurg. 1992;77:369-72.
- [Google Scholar]
- Familial intradural arachnoid cysts. Report of two cases. J Neurosurg. 1979;50:826-9.
- [Google Scholar]
- Spinal arachnoid cyst with weakness in the limbs and abdominal pain. Pediatr Neurol. 1999;20:155-6.
- [Google Scholar]
- Symptomatic intramedullary arachnoid cyst. Report of two cases and literature review. Neurochirurgie. 2007;53:54-7.
- [Google Scholar]
- Spinal intramedullary arachnoid cyst in children. Pediatr Neurosurg. 2008;44:243-6.
- [Google Scholar]
- Thoracic intramedullary arachnoid cyst in an infant. J Neurosurg Pediatr. 2009;3:132-6.
- [Google Scholar]
- Intramedullary arachnoid cyst: 3-year follow up after bilateral dorsal root entry zone myelotomy. Acta Neurochir (Wien). 2008;150:595-7.
- [Google Scholar]
- An adult cervical intramedullary arachnoid cysts: Case report and review. J Spine. 2017;6:383.
- [Google Scholar]
- Spinal intramedullary arachnoid cyst: Case report and literature review. Spine J. 2014;14:e9-15.
- [Google Scholar]
- Spinal intramedullary arachnoid cyst – A rare case or a distinct rare entity.? Austin Neurosurg Open Access. 2014;1:1018.
- [Google Scholar]
- Intramedullary arachnoid cyst in an adult: Case report and review. Asian J Neurosurg. 2016;11:70.
- [Google Scholar]






