Translate this page into:
Suprasellar dermoid cyst associated with colloid cyst of the third ventricle: Disordered embryogenesis or a mere coincidence?
Address for correspondence: Dr. Nilesh S Kurwale, Department of Neurosurgery, Aditya Birla Memorial Hospital, Pune - 411 033, India. E-mail: drnilesh1998@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intracranial dermoid cyst and colloid cysts of the third ventricle are rare benign congenital lesions of early adulthood. Both lesions are thought to be congenital in origin however association is rare. Only one case of this association has been reported. We report a 22-year-old male with suprasellar dermoid cyst and colloid cyst of the third ventricle presenting simultaneously. Embryogenesis of this association has been discussed.
Keywords
Anterior neuropore closure
colloid cyst
neural tube defects
suprasellar dermoid
Introduction
Intracranial dermoid cysts and colloid cysts are rare congenital lesions generally occurring along the midline.[123] Dermoid cysts are known to be ectodermal in origin while debate still exists about the embryological origin of colloid cysts.[3] Here, we report a 22-year-old young male with suprasellar dermoid cyst associated with a colloid cyst of the third ventricle and discuss the possibility of their unified embryological derivation. To best of our knowledge, only one similar case has been reported previously.[4]
Case Report
A 22-year-old male patient presented with on and off frontal headaches and occasional blurring of vision for 1 year. Patient was operated initially for suprasellar dermoid cyst 5 years back. Bifrontal craniotomy and partial excision of dermoid cyst was performed during previous surgery. Patient was asymptomatic 4 years after first surgery. Clinical examination was normal with visual acuity of 6/6 in both eyes without evidence of any field defects on perimetry. Routine hematological and biochemical investigations were normal. Hormone status of the patient was normal. Magnetic resonance imaging (MRI) revealed mainly cystic lesion in the suprasellar region with small solid component anteriorly which was hyperintense on T1-weighted sequences without any contrast enhancement. Cyst wall did not show any enhancement on contrast. Simultaneously a colloid cyst of 1.2 × 1.5 cm was seen at the foramen of Monro, mainly occupying third ventricle with evidence of mild hydrocephalus [Figure 1a]. An old bifrontal craniotomy was re-explored and complete excision of suprasellar dermoid cyst was achieved through bilateral subfrontal approach along with transcortical transventricular excision of colloid cyst in the same setting. Intraoperatively, suprasellar cyst was containing a whitish fluid with fat globules with small solid vascularized fatty nodule. Post-operative scans showed complete excision of both the lesions [Figure 1b]. Histopathological findings confirmed the diagnosis [Figure 2].
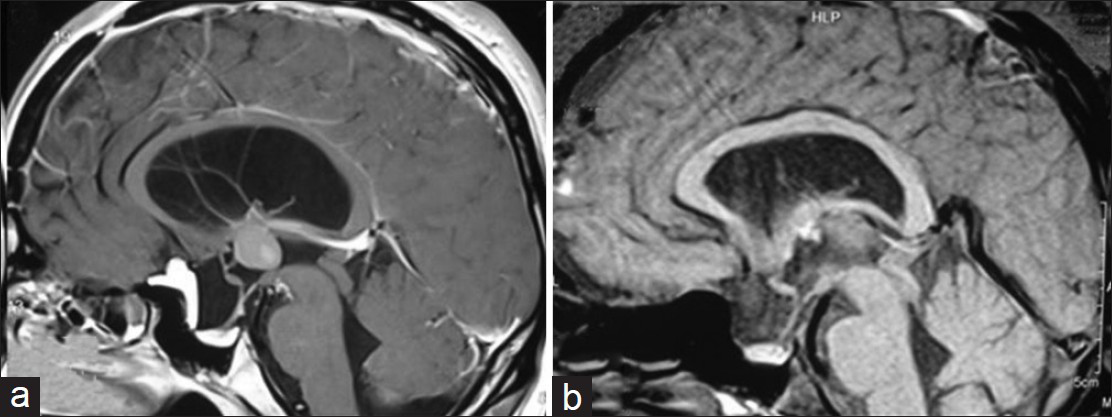
- Sagittal sections of contrast-enhanced magnetic resonance images of brain showing cystic lesion in the suprasellar area with small solid part anteriorly. Cyst displaced the pituitary stalk posteriorly. Pituitary gland is seen compressed in the sella. Colloid cyst of the third ventricle is evident with mild ventriculomegaly (a). Post-operative scans (48 hrs) scans showed complete excision of dermoid and colloid cyst with decreased mass effect on the optic chiasm (b)
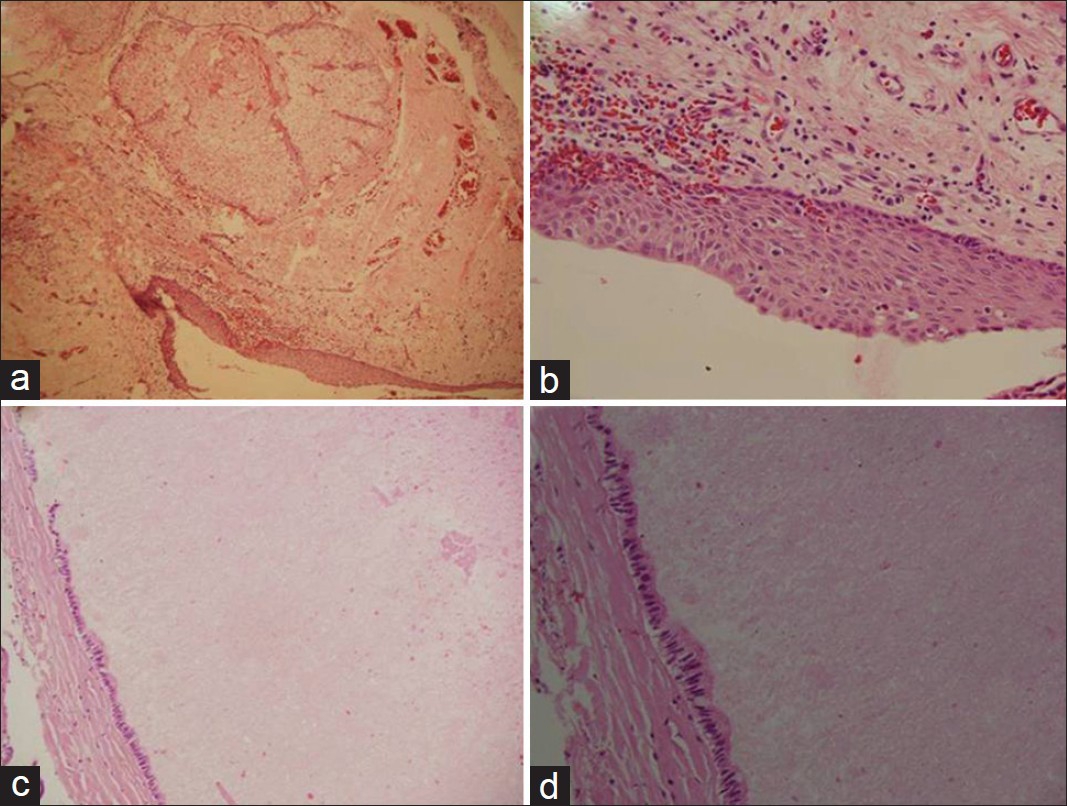
- Photomicrographs showing stratified squamous epithelium with underlying sebaceous glands (a). Higher magnification of the lining epithelium (b). Colloid cyst wall comprising fibrocollagenous wall and is lined by columnar epithelium (c) with high-power view of lining epithelium (d). (a, b: HandE ×100; c, d: H and E ×200)
Discussion
Intracranial dermoid cysts generally occur along the midline and are derived from the trapped somatic ectoderm during embryological development during third to fifth week of gestation.[3] These cysts are generally associated with dermal sinus tracts and other neural tube closure defects; however, dermal sinus tract may be absent in suprasellar and cerebello-pontine angle dermoids.[34] These lesions mainly presents with headache, local sings of mass effect, or neural compression. Spontaneous rupture and chemical meningitis, hydrocephalus are rare presentations.[34] Surgical excision is preferred treatment; however, complete excision is seldom achieved.
Colloid cysts of the third ventricle are also rare benign midline lesions presenting during early adulthood. Colloid cyst generally become symptomatic in early adulthood and mainly presents with headache and hydrocephalus.[2] Sudden death is most feared presentation which is fortunately rare.[2] Although controversy exists about timing of surgery of asymptomatic colloid cysts, symptomatic ones are excised surgically at the earliest. With advent of endoscopy, complete or partial resection of colloid cyst has become the preferred treatment option.
Congenital origin of these cysts is accepted universally; however, cell of origin is highly debated.[145] Initial reports suggested their neuroepithelial origin as the derivatives of paraphysis or ventricular ependyma and these were further supported later by other studies.[67] However, Mackenzie[8] in 1991 suggested the endodermal derivation of these cysts on the basis of ultrastructural features which was supported by other authors.[59] Until recently endodermal derivation of these cysts enjoyed the favor when Nagaraju et al.,[10] in 2010 reignited the debate by claiming colloid cysts as paraphysis remnants in human.
Colloid cysts are associated with various developmental malformations like corpus callosal agenesis, anterior cranial fossa encephalocels, cavum veli interpositi, and multiple neuroepithelial cysts and aqueductal stenosis.[1] These malformations represent a spectrum of neural tube closure defects and associated anomalies. Although isolated sporadic form of colloid cyst is most common occurrence, these associations suggest disordered embryogenesis as a possible mechanism in their formation. Colloid cyst has also been reported to be associated with frontal epidermoid cyst.[11] Cheng et al.,[4] in 1999 reported a case of nasal dermoid sinus cyst associated with colloid cyst of third ventricle and proposed a fascinating theory of “anterior neuropore corridor defects” to explain the spectrum of these associated rare midline lesions. According to this theory, defective closure of situs neuroporicus promotes the neuroepithelium adjacent to commissural plate derivatives to form a vacuolated paraphysis growing slowly as colloid cyst of the third ventricle. Similar derivation from paraphysial remnants was also reported by Nagaraju et al., in 2010 supporting Cheng's hypothesis.[10] Although lack of substantial evidence remained main drawback of this theory, disordered embryogenesis appears to be the most plausible explanation in our case rather than mere coincidence.
Conclusions
Suprasellar dermoid cyst associated with colloid cyst of the third ventricle is a rare presentation. This association appears more than coincidence and can be partially explained by anterior neuropore corridor defect theory. This unique case provides the insight to the embryogenesis of other midline congenital lesions.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Familial colloid cyst of the third ventricle: Case report and review of associated conditions. Neurosurgery. 1996;38:392-5.
- [Google Scholar]
- A theory on the natural history of colloid cysts of the third ventricle. Neurosurgery. 2000;46:1077-83.
- [Google Scholar]
- Intracranial midline dermoid and epidermoid cysts in children. J Neurosurg. 2004;100:473-80.
- [Google Scholar]
- Intracranial nasal dermoid sinus cyst associated with colloid cyst of the third ventricle. Case report and new concepts. Pediatr Neurosurg. 1999;31:201-6.
- [Google Scholar]
- Colloid cysts of the third ventricle: Ultrastructural features are compatible with endodermal derivation. Acta Neuropathol (Berl). 1992;83:605-12.
- [Google Scholar]
- Neuroepithelial (colloid) cysts: Pathogenesis and relation to choroid plexus and ependyma. Arch Pathol. 1965;80:214-24.
- [Google Scholar]
- An immunohistochemical study of neuroepithelial (colloid) cysts. J Neurosurg. 1989;71:91-7.
- [Google Scholar]
- Cysts of the neuraxis of endodermal origin. J Neurol Neurosurg Psychiatry. 1991;54:572-5.
- [Google Scholar]
- Colloid cyst of the third ventricle: A comparative immunohistochemical study of neuraxis cysts and choroid plexus epithelium. J Neurosurg. 1993;78:101-11.
- [Google Scholar]
- Colloid cyst of the third cerebral ventricle with an embryological remnant consistent with paraphysis cerebri in an adult human. Clin Neuropathol. 2010;29:121-6.
- [Google Scholar]






