Translate this page into:
Simultaneous Occurrence of Deep Vein Thrombosis and Carotid Artery Thrombosis in Antiphospholipid Antibody Syndrome
Address for correspondence: Dr. Rohan R. Mahale, Department of Neurology, M. S. Ramaiah Medical College and Hospital, Bengaluru - 560 054, Karnataka, India. E-mail: rohanmahale83@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Antiphospholipid antibodies (aPLas) are associated with an increased risk of arterial and venous thromboembolism.[1] These include lupus anticoagulant, anticardiolipin antibodies, and anti-β2-glycoprotein-1 antibodies. Antiphospholipid antibody syndrome (APS) is a prothrombotic condition characterized by the presence of these antibodies in patients with recurrent pregnancy morbidity and/or thromboembolic complications.[2] Some patients with aPLa develop multiorgan failure due to widespread thrombotic events, known as catastrophic APS.[3] The co-occurrence of cerebral arterial thrombosis and deep vein thrombosis of lower limb in a patient with APS has not been reported. We report a middle-aged female with the previous history of second-trimester pregnancy loss presenting with deep vein thrombosis of lower limb with carotid artery thrombosis simultaneously.
A 38-year-old female patient presented with history of painful swelling of her right lower limb of 5 days duration. On the 2nd day of admission, she noticed weakness in left upper and lower limb with deviation of angle of mouth to the right. She had slurring of speech. She had previous history of the second-trimester pregnancy loss. There was no previous history of migraine headache, seizures, drug intake, diabetes, or hypertension. On examination, her vitals were stable. Her right lower limb was swollen with tenderness. Neurological examination revealed mild slurring of speech with left upper motor neuron facial palsy. Motor assessment showed left hemiplegia (2/5 in upper and 3/5 in lower limb). Reflex was sluggish in left upper and lower limb with left extensor plantar response. Her complete hemogram showed mild anemia and thrombocytopenia (hemoglobin – 9.6 g/dL; platelet count – 52,000); renal, liver, and thyroid functions were normal. Serum electrolytes were normal. Magnetic resonance imaging of brain showed acute infarct in the right middle cerebral artery (MCA)/anterior cerebral artery and MCA/posterior cerebral artery borderzone territory. Magnetic resonance angiography of neck vessels and circle of Willis showed decreased flow in the right internal carotid artery from its origin. Duplex ultrasonography showed thrombosis of the right femoral vein [Figure 1]. Serological testing for antinuclear antibody, auto-antibodies profile including anti-double-stranded deoxyribonucleic acid, anti-Ro, and anti-La antibodies was negative. Serological testing for human immunodeficiency virus, hepatitis B virus (hepatitis B surface antigen), and venereal disease research laboratory was negative. Serum homocysteine, protein C and S, and antithrombin III levels were within normal limits. A hypercoagulability clinical evaluation showed significantly elevated aPLa (immunoglobulin G 24.6; immunoglobulin M 56.4) and positive lupus-like anticoagulant. She received systemic anticoagulation with heparin followed by transition to oral warfarin. During her stay, she had mild improvement in limb weakness and modified Rankin score (mRs) at the time of discharge was 4/6. At 3-month follow-up, her mRs was 2/6, but persistent elevated aPLa levels.
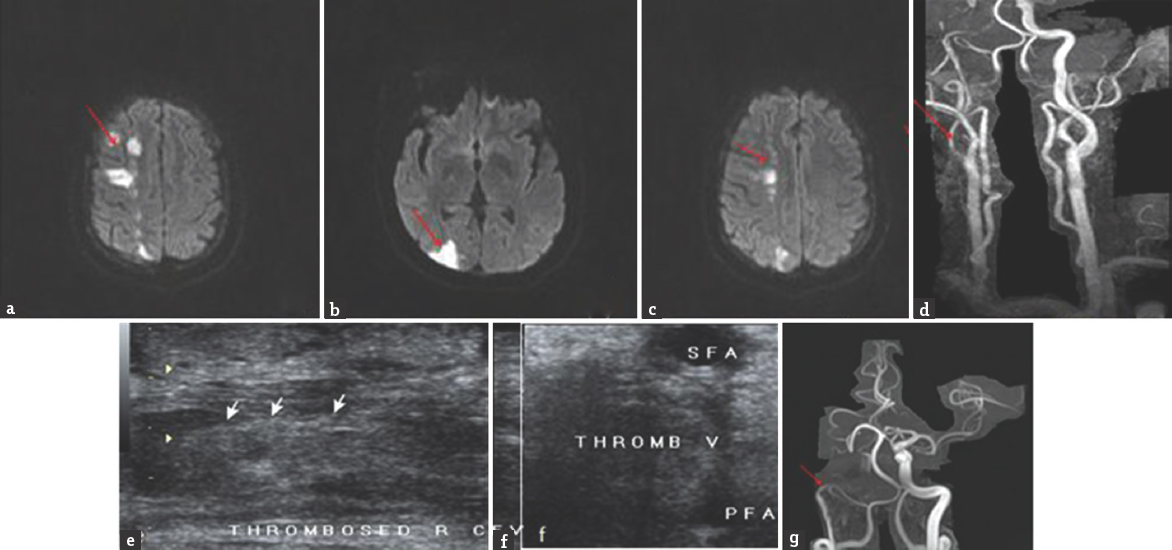
- Magnetic resonance imaging brain diffusion-weighted imaging (a), (b and c) showing diffusion restriction in right anterior cerebral artery/middle cerebral artery and middle cerebral artery/posterior cerebral artery borderzone territory (red arrow); magnetic resonance angiography neck vessels (d) and circle of Willis (g) showing decreased flow in the right internal carotid artery from its origin (red arrow); Duplex ultrasonography(e and f) showing thrombus in the right femoral vein
Neurological manifestations of APS include cerebrovascular disease (stroke, transient ischemic attack, and venous thrombosis), seizures, migraine headaches, and cognitive dysfunction.[4] The syndrome is referred as the primary APS in the absence of an underlying connective tissue disorder whereas the secondary APS is most commonly seen with systemic lupus erythematosus. The mechanisms of thrombosis in APS are aPLa interference with endogenous anticoagulant mechanisms, binding and activation of platelets, interaction with endothelial cells and inducing expression of adhesion molecules and tissue factor, and activation of the complement cascade.[5] Premature atherosclerosis has also been associated with APS.[6] Deep vein thrombosis of the lower extremities is the most common initial manifestation in APS, occurring in approximately 30% of patients.[7]
The diagnosis of APS is based on clinical criteria of pregnancy morbidity or one or more vascular thromboembolism, and laboratory findings of medium or high titer aPLas that are present on two or more occasions at least after 12 weeks.[5] Our patient satisfied the above criteria in terms of previous pregnancy morbidity and one or more vascular thromboembolism (carotid artery and deep veins of lower limb) with high titer aPLa on 2 occasions, 12 weeks apart. Thrombocytopenia is found in 20% of patients with APS. The occurrence of thrombocytopenia and thrombosis in APS suggests that aPLas interact with platelets triggering platelet aggregation and thrombosis. In vitro and in vivo studies have shown that aPLa binds with platelets, increasing their aggregation and activation in the presence of subthreshold concentrations of thrombin, adenosine diphosphate, or collagen.[8]
Sakamoto et al. reported a male patient with simultaneous presentations of deep vein thrombosis and cerebral sinus thrombosis in primary APS.[9] However, our patient had simultaneous occurrence of deep vein thrombosis and carotid artery thrombosis.
The co-occurrence of cerebral arterial and deep vein thrombosis in APS has not been reported. This patient represents the rare co-occurrence of carotid artery and deep vein thrombosis of lower limb in APS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Basilar artery thrombosis in the setting of antiphospholipid syndrome. Proc (Bayl Univ Med Cent). 2014;27:210-2.
- [Google Scholar]
- Catastrophic antiphospholipid syndrome: International consensus statement on classification criteria and treatment guidelines. Lupus. 2003;12:530-4.
- [Google Scholar]
- Antiphospholipid syndrome and central nervous system. Clin Neurol Neurosurg. 2010;112:602-8.
- [Google Scholar]
- Antiphospholipid antibodies and the antiphospholipid syndrome: Pathogenic mechanisms. Semin Thromb Hemost. 2008;34:236-50.
- [Google Scholar]
- Systemic antiphospholipid syndrome and atherosclerosis. Clin Rev Allergy Immunol. 2007;32:172-7.
- [Google Scholar]
- Antiphospholipid syndrome: Clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum. 2002;46:1019-27.
- [Google Scholar]
- Comparison of the effects of anticardiolipin antibodies from patients with the antiphospholipid syndrome and with syphilis on platelet activation and aggregation. Thromb Haemost. 1995;73:529-34.
- [Google Scholar]
- Simultaneous presentations of deep vein thrombosis and cerebral sinus thrombosis in a case of primary antiphospholipid syndrome. Angiology. 2009;59:765-8.
- [Google Scholar]





