Translate this page into:
Sacroiliac Pain: A Clinical Approach for the Neurosurgeon
Address for correspondence: Dr. Luis Rafael Moscote-Salazar, University of Cartagena, Cartagena, Colombia. E-mail: mineurocirujano@aol.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pain originating from sacroiliac joint may also cause pain in the lumbar and gluteal region in 15% of the population. The clinical manifestation represents a public health problem due to the great implications on the quality of life and health-related costs. However, this is a diagnosis that is usually ignored in the general clinical practice; probably because of the unknown etiology, making harder to rule out the potential etiologies of this pathology, or maybe because the clinical criteria that support this pathology are unknown. By describing several diagnostic techniques, many authors have studied the prevalence of this pathology, finding more positive data than expected; coming to the conclusion that even though there is no diagnostic gold standard yet, an important amount of cases might be detected by properly applying several tests at the physical examination. Thus, it is necessary to have knowledge of the physiopathology and clinical presentation so that diagnosis can be made to those patients that manifest this problem. We present a clinical approach for the neurosurgeon.
Keywords
Lumbar pain
neurosurgery
sacroiliac dysfunction
sacroiliac pain
INTRODUCTION
Lumbar pain affects two-thirds of the adult population, and it is a common cause of visits to the general practitioner and neurosurgeon. Lumbar pain may be originated by several causes that include degenerative, traumatic, and metabolic caused; among the causes of lumbar pain, we can find the pain that originates in the sacroiliac joints that because of the clinical context conforms the called “Sacroiliac Pain Syndrome.”
To talk about sacroiliac pain, some terminology should be cleared.[123] The terms sacroiliac joint dysfunction and sacroiliac pain syndrome (or sacroiliac joint pain) are usually used indistinctively to refer to this pathology, however, they do not have the same meaning, and they are not synonyms.[4] The first one refers to the movement or change in position of any of the structures that conform the joint, with the possibility of causing pain.[5] On the other hand, the second one refers to a wide range of pathologies (among which we can find joint dysfunction) capable of generating pain in several locations with common innervation with the sacroiliac joint.[4]
This way, instead of isolated concepts, they work as structural parts of a group of pathologies whose clinical presentation includes localized pain on the lower back, gluteal region, inguinal region, or any region of the lower limb.[16]
In 1950, Goldth and Osgood were the first to describe this type of pain, affirming that it was originated by a sprain of the sacroiliac joint. In the following decades, joint dysfunction was considered as the main cause, posteriorly, Mixter and Barr published in 1934 the discovery of intervertebral disc prolapse in the lumbar region, making easier to come up with a mechanical explanation for the lower back pain with irradiation to the lower limbs and widening the possibilities of a diagnosis with these characteristics.
Nowadays, the available evidence is empiric since it has been obtained through the information given by those patients who have been treated successfully to reduce symptoms and/or suggestive signs of sacroiliac pain syndrome (sacroiliac joint pain).[78]
In the origin of lower back pain, that also affects previously described regions, also intervene: sacroiliac joint, intervertebral discs, nerve roots, facet joint, vertebrae, spinal cord, ligaments, and muscles. However, it has not been proven that vertebrae, muscles, and ligaments are a common source of pain in these regions; unlike intervertebral disc, sacroiliac joints, and facet joints that, through diagnostic techniques such as pain mapping and anesthetic block, have been proven to be strong causes of pain.[8] The lack of specificity of this localized pain is due to the correlation between the sensorial regions of lumbosacral and sacroiliac regions, which have as common structure the dorsal nerves S1–S3.[49]
Sacroiliac pain is the second most common cause of visits to the neurologist in the US, after a headache. Both men and women seem to be equally susceptible, referring to have experienced it at least once in their life.[10] It frequently starts between the 30 and 50 years old, having a prevalence peak between the 70 and 79 years[11] as part of the aging process, but also, as a result of a sedentary lifestyle with poor exercise.[12]
The sacroiliac joint has been found to be compromised in about 5%–15% of all cases of chronic pain,[4] in the case of joint dysfunction, even though its prevalence is unknown, it is estimated between 15% and 25%.[13] In a trial of 1293 patients with lower back pain, sacroiliac dysfunction was the primary diagnosis in 22.5% of cases; and in 33% of these, it coexisted with an additional source of pain.[14] This may give an idea of how defying it can be to make an accurate diagnosis of this pathology.
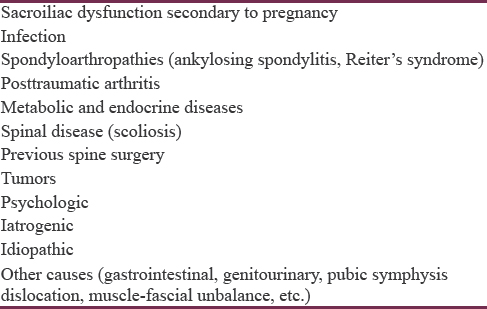
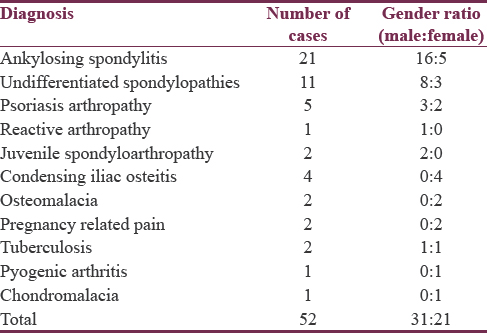
It must be pointed out that the management of patients with lower back pain, with or without irradiation, the different conditions that may cause it should be considered. Although most of these etiologies are benign, the impact in the quality of life is not. Hence, infections, trauma, metabolic bone disease, and spondyloarthropathies are a few of the pathologies that are well described and accepted, that by image studies have demonstrated sacroiliac joint disease. All these pathologies are inflammatory states that commonly would not case any diagnostic confusion, however, sacroiliac dysfunction is caused gradually by pelvic rotation, joint block, hyper- or hypo-motility, thus, they cannot be demonstrated in an X-ray and to diagnose them becomes tortuous.[1516171819202122]
DIAGNOSIS
The International Association for the Study of Pain (IASP), in 1994, came up with three criteria for sacroiliac pain diagnosis.[617]
-
Localized pain in the sacroiliac region
-
Pain that is produced by tension with several maneuvers
-
Pain that decreases with local infiltration of anesthetics to the articulation.
However, in the last years, several authors, among them physiotherapist and chiropractors, have questioned the reliability and validity of them, mentioning they are unequivocal.
The first criterion has not been proven to be present in all cases, due to the several localizations of pain (gluteal, lower back, calfs, among others); the second criterion, most of the tests that have been used to induce pain have been found to lack enough sensitivity and specificity to make a reliable diagnosis. Despite this, the third criterion has been found to have more sensitivity and specificity, thus it is considered the reference nowadays.[1718]
Even with all this, there's still no definition to replace the actual definition by the IASP, so it is still the global reference for diagnosis. Based on it, a list of aspects to be consider for the diagnosis is presented while obtaining the health history of a patient with sacroiliac pain.
Anamnesis
It has to be clear that pain coming from the sacroiliac joint may present in several anatomic regions, whether isolated or together with another: lower or upper lumbar, gluteal, inguinal, any thigh zone, lower abdomen, or even calfs [Table 1]. For this reason, some pathologies that might cause the pain should be ruled out [Tables 2 and 3]. Several findings in the health history have estimated the frequency on the right side of the body in 45% of the cases, on the left side in 35% and bilaterally in 20%, with the prevalence between 22.5 and 62.8%.[7]
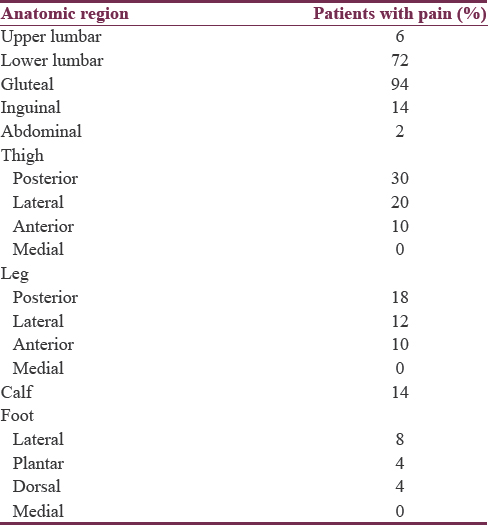
Patients often refer the start of it after the sudden lifting of heavy objects, holding them for long periods of time while having the back at flexion, falling over the gluteal region, car accidents, especially those which had rear impact and the ipsilateral foot to the pain was on the break.[19] The fact that pain increases with Valsalva maneuver should be pointed out, by sitting or lying on the affected side of the body or while holding heavy objects on the affected side of the body, on the other hand, it decreases when an object is held on the opposite side to the pain or the ipsilateral limb is flexed [Table 1].[78]
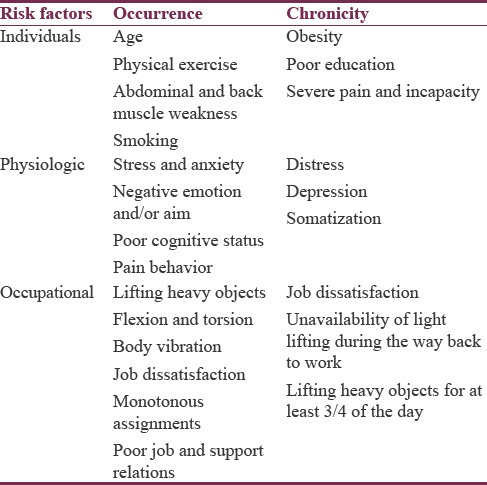
The causes may be divided into intra- and extra-articular; arthritis and infection being two examples of frequent intra-articular causes, and fractures and sprain frequent are extra-articular causes.[13] In addition, there are numerous factors that may predispose a person to develop disease gradually, and at the same time predict a late recovery [Table 4].
There is some controversy regarding the lumbar spine surgery as a predisposing factor for sacroiliac pain. Several publications have attributed this to the weakening of muscles and trauma to the joint cavity during surgery, besides postsurgery hypermotility.[13] However, there are not enough tests to show a direct relation between the latter and sacroiliac pain.
Furthermore, pregnancy has been considered as an important factor, by predisposing the woman to have joint pain caused by weight gain, hyper-lordosis, trauma during labor, and induced ligamentous laxity by estrogen and relaxin.[20] Besides anxiety and other emotions, which have shown to activate a few number of motor units synergistically and repetitively during pregnancy.[2122]
Physical examination
Detailed neurologic examination of spine and hips must be performed, so it allows to identify whether the pain is somatic or neural. For this, in the literature, several maneuvers and clinical test have been described to unmask the pain origin at the sacroiliac joint. It is considered that the presence of three or more signs arise the suspicion of sacroiliac origin. Tests have been classified of several ways,[523] but for a better academic practice the following classification is presented:
-
Functional: Walking, undressing, walking on tiptoes and heels, and making sit-ups
-
Pain producers: Compression test (approximation), distraction test, Patrick's sign, Gaenslen's test, posterior tension tests, Fortin's toe test, Gillet's test, etc
-
Motility: Lumbar spine flexion/extension, lateral flexion of lumbar spine and hip rotation
-
Palpation: Pressure test on the middle sacral line, compression test, among others.[24]
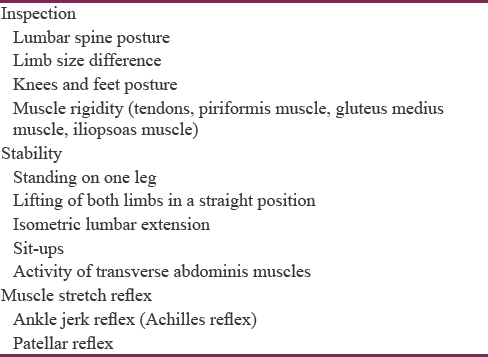
Likewise, other criteria should not be ignored such as inspection of muscle disposition and stability during the maneuvers and osteotendinous reflexes.
Several trials have demonstrated that the reliability of induction test is greater than other kind of tests, but the possibility that one test alone can make the diagnosis of sacroiliac pain is very low.[18] Sensitivity and specificity in the clinical examination increase proportionally with the number of positive induction tests. Two trials reported that three or more of these tests showed specificity and sensitivity of 79% and 85%, and 78% and 94%, respectively,[6] which were posteriorly confirmed in a meta-analysis.[17]
In this paragraph, some of the most important induction test are described, whose positivity is seen in most patients with sacroiliac pain [Table 5]:
-
Compression test (approximation test): With the patient laying on the healthy side, the affected side facing upward with the muscles flexed at 45° and knees at 90°, the examiner (behind the patient) places both hands on the iliac crest and makes downward medial pressure
-
Distraction test (separation test): With the patient laying supine, the examiner, standing on the affected side of the patient, places each of their hands on the anterior-superior ipsilateral iliac spine and applies dorsal-lateral pressure
-
Patrick's sign: With the patient lying supine with the examiner standing on the affected side of the patient, the affected limb is flexed, placing the foot over the contralateral knee, finally when pushing downward on the knee of the affected side the patient refers pain
-
Gaenslen's test (pelvic torsion): With the patient laying supine, placing the affected side limb over the examination table, non-affected side limb is flexed until the knee touches the abdomen. The contralateral limb (of the affected side) will hyper-extend, and then a slight pressure will be applied on the knee of the same side, and the patient will refer pain
-
Posterior tension test: With the patient laying supine with the healthy side limb on the table, the examiner standing on the affected side of the patient will flex the limb at 90° with slight adduction while simultaneously applying slight pressure on the flexed knee [Figure 1], the patient will refer pain
-
Gillet's test: With the patient standing on one knee and lifting the other, flexing it toward the chest, the patient will refer pain.

- Posterior tension test
Imaging
Simple hip X-ray is cheap and accessible, but not sensible to detect initial structural changes, does not have specificity to assess inflammatory activity.
In the assessment of sacroiliac joint, magnetic resonance imaging (MRI) and computed tomography (CT) scan constitute the most effective diagnostic tools to determine arthrosis and arthritis changes in the articulation, MRI can even show minimal changes such as: inflammatory activity in subchondral bone and ligaments, as in spondyloarthropathy as well as cartilage compromise. On the other hand, MRI can show subperiosteal, transcapsular, and periarticular infiltrations like those of septic arthritis, in these cases, CT scan and simple X-ray are useless.
TREATMENT
Conservative treatment: this is based on physical therapy, whose only objective is stabilization of sacroiliac joint, founded on pelvic stabilization exercises, and muscle strengthening.
The use of sacroiliac belts can also be strategic; the purpose of them is to stabilize the sacroiliac joint movements.
Anesthetics and steroids injections may also be useful. The use of radiofrequency to denervate the sacroiliac joint with secondary pain control has been an interesting alternative since it has been determined that sacroiliac joint innervations comes from L2–S2, L4–S2, and L5–S2.
As for the pharmacologic management, there are three groups of drugs that may be used for a patient with sacroiliac pain:
-
Simple analgesic: Such as acetaminophen and muscle relaxers, whenever there's associated muscle contraction. Whenever possible, acetaminophen should be used as analgesic
-
Nonsteroidal anti-inflammatory drugs (NSAID): They should be used for short periods and the patient should be informed about the possible adverse effects. There are several NSAID groups, thus, poor pain relief with one NSAID does not disqualifies the whole NSAID group and the physician should try with another groups with the purpose of finding the expected result
-
Opioid analgesics: Reserved for lumbar pain syndrome that does not improve with any of the previously mentioned drugs and also for pain crisis.
Surgical treatment: Reserved for patients who do not respond to conservative treatment, depending on the etiology.
CONCLUSIONS
Sacroiliac pain is a cause of lumbar pain that represents a challenge for physicians and neurosurgeons, as we have seen, it is responsible for 15%–25% of cases of axial lumbar pain, and there are several pathologies that may be related to the pathophysiology.
A detailed health history and physical examination, including sacroiliac joint test, image studies, and laboratory test allow an integral approach to the patient with sacroiliac pain. Repetitive assessment of patients will allow the physicians to improve their diagnostic ability for a disease that requires a highly trained neurosurgeon.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Unexplained lower abdominal pain associated with sacroiliac joint dysfunction: Report of 2 cases. J Nippon Med Sch. 2011;78:257-60.
- [Google Scholar]
- The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome. J Bodyw Mov Ther. 2012;16:29-35.
- [Google Scholar]
- Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976). 1996;21:1889-92.
- [Google Scholar]
- Clinical considerations of sacroiliac joint anatomy: A review of function, motion and pain. J Osteopath Med. 2004;7:16-24.
- [Google Scholar]
- Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16:142-52.
- [Google Scholar]
- A systematic review of sacroiliac joint interventions. Pain Physician. 2005;8:115-25.
- [Google Scholar]
- Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646-56.
- [Google Scholar]
- Sacroiliac joint pain: A comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101:1440-53.
- [Google Scholar]
- Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res. 1987;217:266-80.
- [Google Scholar]
- Sacroiliac joint dysfunction: From a simple pain in the butt to integrated care for complex low back pain. Tech Reg Anesth Pain Manag. 2011;15:40-50.
- [Google Scholar]
- The sacroiliac joint: An underestimated cause for low back pain. J Back Musculoskelet Rehabil. 2007;20:135-41.
- [Google Scholar]
- Diagnostic validity of criteria for sacroiliac joint pain: A systematic review. J Pain. 2009;10:354-68.
- [Google Scholar]
- The reliability of selected motion- and pain provocation tests for the sacroiliac joint. Man Ther. 2007;12:72-9.
- [Google Scholar]
- The sacroiliac joint: Anatomy, physiology and clinical significance. Pain Physician. 2006;9:61-7.
- [Google Scholar]
- Provocative sacroiliac joint maneuvers and sacroiliac joint block are unreliable for diagnosing sacroiliac joint pain. Joint Bone Spine. 2006;73:17-23.
- [Google Scholar]
- Chronic pelvic pain: Pelvic floor problems, sacroiliac dysfunction and the trigger point connection. J Bodyw Mov Ther. 2007;11:327-39.
- [Google Scholar]
- Sacroiliac joint pathologies in low back pain. J Back Musculoskelet Rehabil. 2009;22:91-7.
- [Google Scholar]
- Inter and intratester reliability of selected clinical tests in examining patients with early phase lumbar spine and sacroiliac joint pain and dysfunction. Adv Physiother. 2010;12:74-80.
- [Google Scholar]






