Translate this page into:
Retrobulbar optic neuropathy secondary to isolated sphenoid sinus disease
Address for correspondence: Dr. Atanu Biswas, Department of Neurology, Bangur Institute of Neurosciences, 52/1A, SN Pandit Street, Kolkata - 700 025, West Bengal, India. E-mail: atabis@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Paranasal sinus disease can cause a condition that mimics optic neuritis. Simultaneous appearance of both diseases would create etiological dilemma. We report two cases of retrobulbar optic neuropathy secondary to isolated sphenoid sinus disease. In the case of a 65-year-old female who had presented with acute loss of vision in the left eye associated with left-sided frontal headache which subsequently turned out to be caused by optic nerve compression at the orbital apex due to collection in abnormally pneumatized left lesser wing of the sphenoid. In another case, a 65-year-old lady had presented with symptoms of bilateral retrobulbar optic neuropathy which was found to be due to direct compression of optic nerves at the orbital apex secondary to metastases from breast carcinoma.
Keywords
Optic nerve compression
optic neuropathy
retrobulbar
sphenoid sinus disease
Introduction
A number of disease processes adjacent to the orbit and optic nerve can cause blindness and often mimic optic neuritis.[1] They are seen far less frequently than ischemic optic neuropathy and optic neuritis. Pathophysiological mechanisms which relate these two distinct disease entities include compressive optic neuropathy secondary to mucoceles, direct extension of sinus infection to the optic nerve from suppurative paranasal sinusitis, from osteomyelitis of the ethmoid and sphenoid sinuses.[23] Optic neuropathy due to sinusitis and mucocele should be considered in patients who have clinical evidence of optic neuritis with seemingly atypical features, particularly in elderly patients with severe sinus disease, a history of fever, ophthalmoplegia or progression of vision loss beyond 2 weeks.[1] Patients with known cancer at another site of the body who develop optic neuropathy, with or without evidence of metastasis, should be suspected of having cancer as a cause.[4]
Case Reports
Case 1
A 65-year-old female was referred to our OPD with acute visual deterioration in the left eye following left-sided frontal headache. She complained of having visual impairment for the past 2 months. The visual loss was nonprogressive and there was no history of color desaturation. She did not have a pain in her eye with ocular movements. Her medical and family history was unremarkable. Examination revealed a visual acuity of projection of rays on the left side and 6/6 on the right side. A swinging flashlight test revealed an afferent pupillary defect on the left. Slit-lamp biomicroscopy and direct and indirect ophthalmoscopy were normal on both sides. The clinical otorhinolaryngological status was unremarkable.
Visual evoked potential (VEP) revealed no wave formation on the left side and normal values on the right side. Magnetic resonance imaging (MRI) showed high signal intensity in the T2-weighted images, isointense on T1 with central hyperintense foci in the left orbital apex extending into the superior extraconal space, which compressed the optic nerve [Figure 1]. CT correlation revealed collection in the abnormally pneumatized lesser wing (Onodi cells) of sphenoid [Figure 2]. Optic neuropathy caused by an isolated mucocele in an Onodi cell was diagnosed. The patient refused endoscopic surgery and was managed conservatively with antibiotics, mucolytics and decongestants. After a month follow up, her vision improved to finger counting at 3 feet.

- Sagittal-oblique T2 image showing thick mucosal secretion (arrow) in the pneumatized Onodi cells at posterior aspect of left orbital roof causing compression of left optic nerve at orbital apex
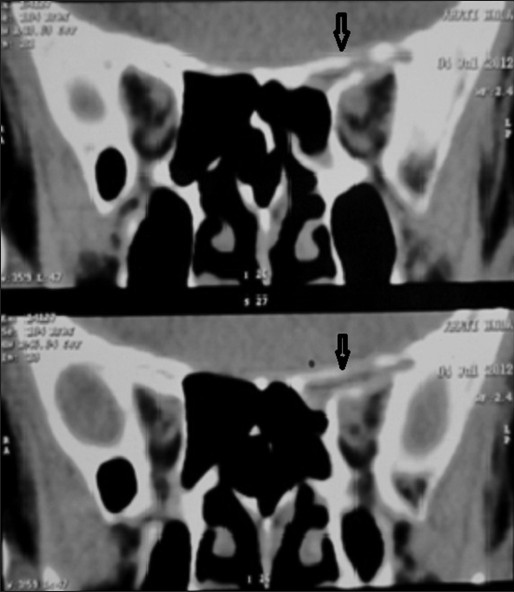
- Coronal CT scan of paranasal sinuses showing soft tissue attenuation (arrow) in left Onodi cells in relation to orbital roof
Case 2
A 65-year-old hypertensive female patient came to neurology OPD with complaints of visual impairment in the right eye for 3 months followed by the left eye 2 months later. Visual loss was gradual in onset and slowly progressive. There was no history of color desaturation and there were no pain with the eye movements. Examination revealed visual acuity of finger counting at 3 feet in the right eye and 6/36 in the left eye. A swinging flashlight test revealed an afferent pupillary defect on right. Slit lamp biomicroscopy and direct and indirect ophthalmoscopy were normal on both sides. A study with visual evoked potentials was conducted which showed increased latency and reduced amplitude on both sides, more on the right side. She had been operated for carcinoma of breast and had received chemotherapy (cyclophosphamide, 5-flurouracil, methotrexate) and radiotherapy 3 years ago. So we considered the possibilities of paraneoplastic, drug-induced, radiation-induced optic neuropathy and optic neuropathy due to direct compression of optic nerve. In this case, cause of retrobulbar optic neuropathy was direct compression as MRI showed metastases with infiltration of optic nerves bilaterally at orbital apex [Figures 3 and 4].

- Contrast enhanced coronal section of MRI brain showing heterogeneously enhancing soft tissue at orbitofrontal ridge and paranasal sinuses
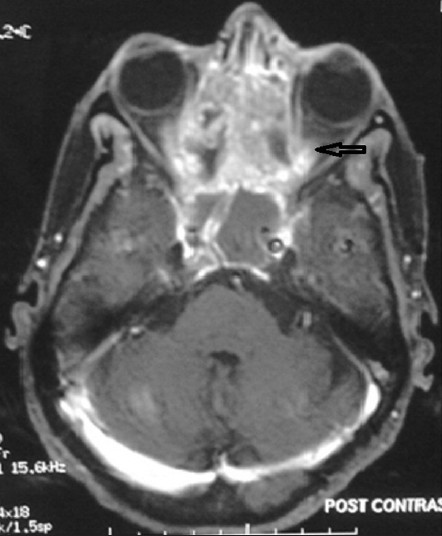
- Contrast-enhanced axial section of MRI brain showing heterogeneously enhancing soft tissue in ethmoid sinus, orbital apex and causing compression of bilateral optic nerves (arrow)
Discussion
Optic neuritis, an acute inflammatory disorder of the optic nerve, clinically demonstrated by a temporary but severe loss of vision, can be caused by a wide variety of diseases. The mean age of onset of optic neuritis is in the third decade of life, but can occur from the first to the seventh decades and it is more common in females.[5] The annual incidence of optic neuritis ranges from 1.4 to 6.4 new cases per 100,000 population.[5] In a typical case of idiopathic optic neuritis, visual loss occurs rapidly over several hours to a few days with decreased color vision and contrast sensitivity. In approximately 90% cases, there may be pain in the ocular region, particularly with movements of the eyeball. Pain typically lasts for 3 to 5 days and if it persists for longer than 7 days optic neuritis should be considered less likely. Recovery typically begins within 1 month.[1]
Acute inflammatory optic neuropathy (retrobulbar optic neuritis) is an uncommon but described complication of acute sinusitis.[1] The relationship of paranasal sinusitis to optic neuritis remains controversial. The close proximity of the optic nerve in the optic canal to the sphenoid sinus makes it vulnerable to direct spread of infection from the sphenoid sinus.[6] The Onodi cell (sphenoethmoidal cell) is an anatomical variation of the most posterior ethmoid air cell that pneumatizes laterally and/or superiorly to the sphenoid sinus. The optic nerve and carotid artery may often course through the lateral aspect of Onodi cell instead of sphenoid sinus proper.[7] Possible mechanisms of optic nerve involvement include compressive optic neuropathy secondary to mucoceles and/or pyoceles; direct extension of sinus infection to the optic nerve from suppurative paranasal sinusitis with invasion of the nerve by local bacteria and secondary inflammatory occlusive vasculitis causing optic neuritis.[236] A rare hypothesis that has been proposed includes demyelination caused by stimulation of the immune system by an infection in the sphenoid sinus.[36] In our case, optic neuropathy was caused by collection in abnormally pneumatized Onodi cells causing swelling along the entire length of the optic nerve secondary to compression or inflammation.
In a patient with known cancer at another site of the body who developed optic neuropathy, etiological possibilities to be considered were paraneoplastic, therapy related (chemotherapy and radiotherapy) or direct compression by carcinoma or metastases. In paraneoplastic optic neuropathy, evidence of other neurological dysfunction is common and the antibody most commonly identified is directed toward collapsing response mediator protein 5 (CRMP 5).[1] Chemotherauptic agents causing optic neuritis are platinum complexes (cisplatin, carboplatin), nitrosoureas (carmustine), 5-fluorouracil (5-FU), methotrexate, fludarabine, paclitaxel, plant alkaloids (vincristine, vinblastine, vindesine, vinorelbine), tamoxifen, and bevacizumab.[8] Optic neuropathy may occur as a delayed effect of radiation therapy.[1] The criteria for diagnosing radiation induced optic neuropathy are irreversible visual loss with visual field defects indicating optic nerve or chiasmal dysfunction and absence of visual pathway compression, absence of optic disc edema and optic atrophy within 6-8 weeks after onset of symptom.[910] Isolated metastases to optic nerve are extremely rare.[11] Reported primary sites are spread from adjacent disease from choroid, orbit, primary central nervous system tumors (meningioma, medulloblastoma), carcinomas (lung, breast, GI tract, pancreas, prostate), melanoma and carcinoid tumor.[11]
Sphenoid sinusitis is an uncommon but treatable cause of optic neuritis. One must consider optic neuropathy due to sinusitis and mucocele in patients who have clinical evidence of optic neuritis with atypical features like elderly patients with severe sinus disease, a history of fever, ophthalmoplegia, or progression of vision loss beyond 2 weeks.[1] In the context of visual loss, opaque sphenoid sinus should always be considered pathological and never dismissed as coincidental.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Abnormalities of optic nerve and retina. In: Daroff RB, Fenichel GM, Jankovic J, Mazziotta JC, eds. Bradley's Neurology in Clinical Practice (6th ed). Philadelphia: Elsevier Saunders; 2012. p. :172-5.
- [Google Scholar]
- Relationship of optic neuritis to disease of the paranasal sinuses. Laryngoscope. 1984;94:1501-8.
- [Google Scholar]
- Reversible retrobulbar optic neuritis due to sphenoidal sinus disorders: Two case studies. Acta Otorrinolaringol Esp. 2008;59:308-10.
- [Google Scholar]
- Isolated optic nerve metastasis of breast cancer initially mimicking retrobulbar optic neuritis. Eur J Ophthalmol. 2011;21:513-5.
- [Google Scholar]
- A Review of Optic Neuritis. 1997. Digit J Ophthalmol. :3. Available at: http://djo.harvard.edu/print.php?url=/physicians/oa/390&print=1#OA_DN
- [Google Scholar]
- Is sphenoid sinus opacity significant in patients with optic neuritis? Eye (Lond). 1999;13:76-82.
- [Google Scholar]
- The prevalence and pattern of pneumatization of Onodi cell in Thai patients. J Med Assoc Thai. 2011;94:1122-6.
- [Google Scholar]
- Radiation optic neuropathy after megavoltage external-beam irradiation: Analysis of time-dose factors. Int J Radiat Oncol Biol Phys. 1994;30:755-63.
- [Google Scholar]
- Isolated metastases to the retina or optic nerve. Int Ophthalmol Clin. 1997;37:251-60.
- [Google Scholar]






