Translate this page into:
Rehabilitation in a Patient with Acute Disseminated Encephalomyelitis Presenting as Tetraplegia with Cortical Blindness
Anupam Gupta, MD Department of Neurological Rehabilitation, The National Institute of Mental Health and Neurosciences (NIMHANS) Bengaluru, Karnataka India drgupta159@yahoo.co.in
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Acute disseminated encephalomyelitis (ADEM) is a rare autoimmune acute demyelinating disease of the central nervous system occurring preferentially in young children commonly post infection/vaccination. 1 It typically presents with features of encephalopathy and multifocal neurological features depending on location, severity, and extent of lesions.
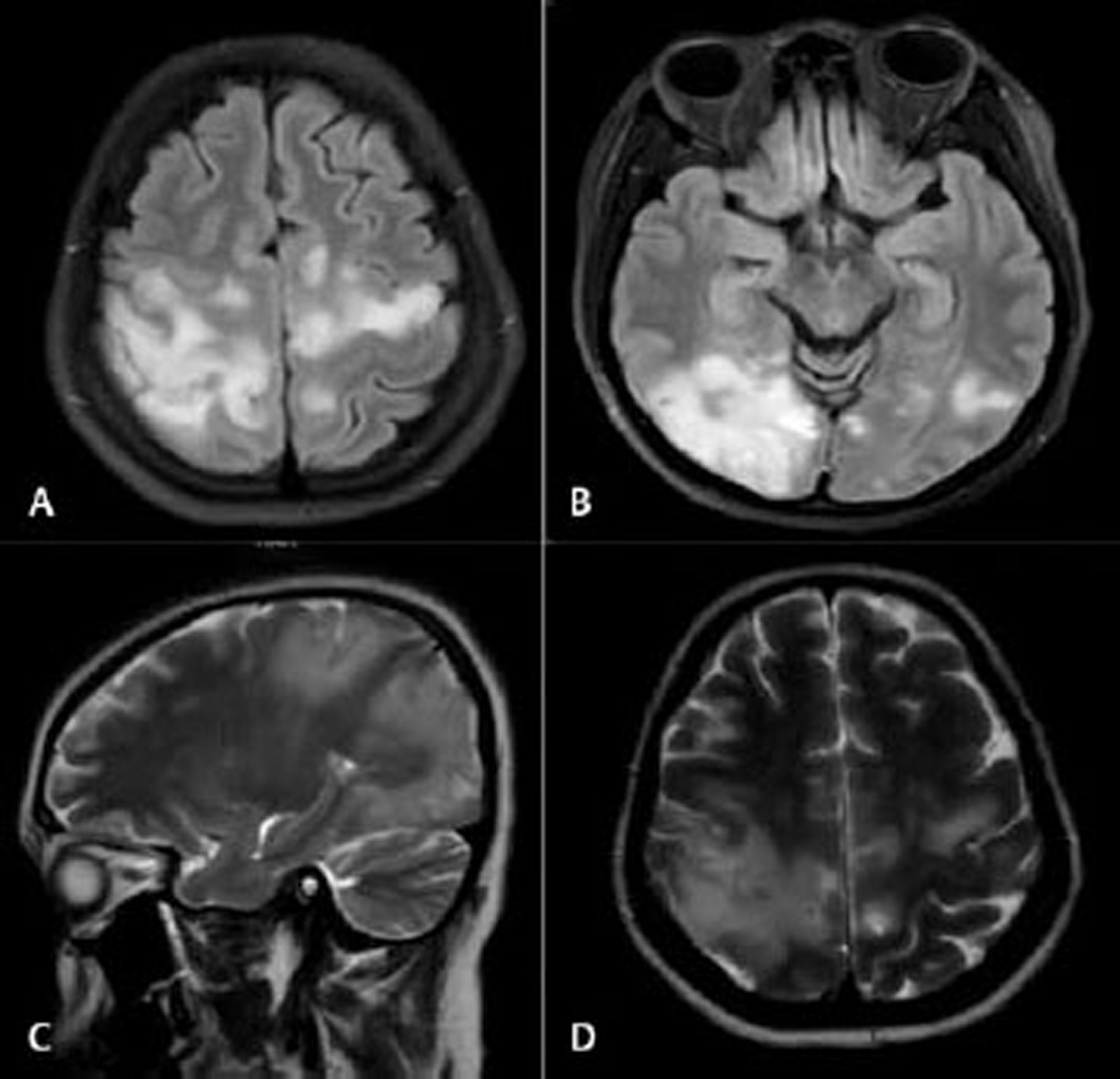
A 30-year-old female presented with tetraplegia and loss of vision of 2 months duration for inpatient rehabilitation. She had acute onset weakness of right upper limb with headache, motor incoordination, double incontinence, and an episode of focal seizure. She was in altered sensorium at the onset of illness. The magnetic resonance imaging showed bilateral asymmetrical hyperintensities in occipital, perirolandic area with patchy subcortical contrast enhancement, and few areas of diffusion restriction. Cerebrospinal fluid examination was normal. Workup for vasculitis and serum neuromyelitis optica spectrum disorders came as negative. A provisional diagnosis of ADEM was made and patient was treated accordingly. She was a known thalassemia carrier with no history of hypertension, diabetes, epilepsy, tubercular disease, or any similar episode in the past (Fig. 1).
-
Fig. 1 (A–D) Magnetic resonance imaging brain of the patient showing bilateral asymmetrical hyperintensities in occipital and perirolandic area with patchy subcortical contrast enhancement.
Fig. 1 (A–D) Magnetic resonance imaging brain of the patient showing bilateral asymmetrical hyperintensities in occipital and perirolandic area with patchy subcortical contrast enhancement.
On admission in rehabilitation, patient had tetraplegia with blindness. She was dependent for all the activities of daily livings, had indwelling catheter for bladder drainage and bowel incontinence. Ophthalmological examination suggested normal fundus and pupillary reaction and possibility of cortical visual loss. Sensations were impaired below C2 bilaterally and motor examination showed dense tetraplegia with hypertonia. Multidisciplinary rehabilitation was focused on the prevention of complications and maximization of functional ability. Physiotherapy program was focused on passive range of motion, stretching exercise of all joints, and bed mobility. Occupational therapy was focused on functional abilities training audio-visuo-tactile stimulation, home and environment modifications. The patient underwent filling and voiding phase cystometrography and trained for timed self-voiding. Wrist cock-up splints and ankle-foot orthosis were advised. Psychotherapy sessions were focused on cognitive retraining and coping with disease.
After 1 month of inpatient rehabilitation, she showed significant motor, cognitive, and functional recovery. She was able to stand and ambulate with moderate support. Repeat ophthalmological evaluation suggested red green recognition and normal fundus in both eyes. She was able to manage her bladder by timed self-voiding 3 hourly.
ADEM usually has monophasic course but recurrent and multiphasic forms have also been reported. Patients gradually improve over several weeks with 50 to 70% experiencing full recovery. Bilateral optic neuritis presenting as subacute visual loss is frequently seen in ADEM. 2 3 The lesions affecting the occipital lobe and visual cortex may also result in cortical visual disturbances, including cortical blindness if severe and bilateral. 4 In the present study, the patient developed tetraplegia with bilateral visual loss that was probably due to involvement of subcortical white matters fibers and bilateral occipital lobes. Some of the strategies to rehabilitate such patient with cortical blindness may include (1) visual restitution therapies, (2) compensation therapies, and (3) substitution therapies over and above the modifications in activities of daily living and home environment. 5 Use of white cane and auditory cues while ambulating helps patient in negotiating terrain without falling. The sensorimotor and bladder involvement is especially challenging due to cortical blindness and multidisciplinary rehabilitation helps in addressing some of these challenges.
Conflict of Interest
None declared.
Funding None.
References
- Acute disseminated encephalomyelitis, multiphasic disseminated encephalomyelitis and multiple sclerosis in children. Brain. 2000;123:2407-2422. (Pt 12)
- [Google Scholar]
- Acute disseminated encephalomyelitis (ADEM) presenting with bilateral optic neuritis. Malays J Med Sci. 2007;14(1):71-74.
- [Google Scholar]





