Translate this page into:
Capacity Building in Mental Health for Bihar: Overview of the 1-Year Blended Training Program for Nonspecialist Medical Officers
Channaveerachari Naveen Kumar, MD, DPM, MAMS Department of Psychiatry, National Institute of Mental Health and Neurosciences (NIMHANS) Hosur Road, Bengaluru India cnkumar1974@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Objective The aim of this study is to give an experiential overview of a 1-year blended training program for nonspecialist medical officers (primary care doctors; PCDs) of Bihar State of India. The training program was aimed to enable PCDs identify, diagnose, and treat commonly presenting psychiatric disorders in primary care
Methods PCDs had a brief onsite orientation program to psychiatric practice at National Institute of Mental Health and Neuro-Sciences (NIMHANS), followed by 10 months of online blended training. The online program followed the NIMHANS Virtual Knowledge- Extension for Community Healthcare Outcomes (ECHO) model, that is, a hub and spokes model of training
Results Twenty-two PCDs participated in this program. Eleven of them got accredited at the end. The onsite orientation consisted of exposure to various psychiatry facilities at NIMHANS, in addition to learning psychiatric history taking and mental status examination. The ECHO model of online learning consisted of fortnightly sessions, lasting 2 hours each. There were 20 such sessions. Each session consisted of a didactic lecture by the psychiatrist followed by a case discussion. The cases were presented by PCDs, moderated by the hub specialists (NIMHANS). At the end of the training, participants rated an average of 4.5/5 on the mode, content and relevance of training and increase in knowledge due to the training. Around 23,000 patients were cared for during the said 1 year by the trained PCDs.
Conclusion Training PCDs in a manner that enables retaining the learnt skills is feasible. However, rigorous evaluation protocols are needed in order to test this in a systematic fashion.
Keywords
Bihar DMHP
primary care doctors
capacity building
Project ECHO
mental health
Introduction
Public Mental Health Care in Bihar
Recently conducted National Mental Health Survey (NMHS) of India (2016)1 showed the treatment gap ranging from 28 to 83% for mental disorders and 86% for alcohol use disorders. To cater to this huge need, the governments (both the federal and states, in collaboration) started the District Mental Health Program (DMHP), with the objective of making basic mental health services available at the district level.2 Though DMHP started way back in 1996, it has taken huge strides in the recent past.3 DMHP is now operational in more than 600 districts of the country. Notwithstanding this, the ground realities are different. For example, most of the DMHPs do not have psychiatrists to lead the teams. This is particularly true in states such as Bihar,4 which is predominantly a rural state, where 11.2 million people are afflicted by a psychiatric disorder at any given point in time. Bihar is the third most populous state of the country with a per capita gross state domestic product of □47,541 at current prices and □33,629 at constant prices and gross domestic product growth rate of more than 10% as per State’s Economic Survey 2017–2018.5 To cater to this huge patient population, the available government human resources in Bihar are 31 psychiatrists (0.03 per 100000 population), two psychiatric social workers, and two clinical psychologists per crore of population,6 way below the global median 9 per 100000 population or less than one mental health worker per 10000 population.7 Bihar initiated DMHP in 11 districts in the year 2015, but no psychiatrist could be recruited to these districts till 2017 (oral communication with the Bihar State health Society). To improve access to mental health services for patients in the face of this severe shortage of specialists, the Bihar government approached NIMHANS to help in capacity building.
Digital Technology in Mental Health
Digital technology has tremendous potential to reach remote, inaccessible areas, and overcome barriers to care. Particularly, tremendous progress has occurred in the area of interventions.8 Comparatively though, use of digital technology in mental health capacity building is relatively less. It is in this context, the initiatives of the National Institute of Mental Health and Neurosciences (NIMHANS), a tertiary care neuropsychiatric academic institute situated in Bengaluru, India are pioneering.9 10 Virtual Knowledge Network (VKN)-ECHO is one such collaboration of NIMHANS with Project ECHO of the University of New Mexico (UNM). Project ECHO (Extension for Community Healthcare Outcomes) is designed to provide best practice care to rural and remote communities that are otherwise underserved. The “Hub” and “Spoke” model links an interprofessional specialist team at an academic center of expertise (the Hub) with primary care doctors (PCDs) (Spokes) across the state.11 Each ECHO session consists of spoke-led presentations of anonymized patient cases and discussion of the cases whereby hub experts provide advice on the management. This is followed by a brief didactic on a mental health-related topic from the curriculum for the course.12
Based on the previous successful implementation of the ECHO model, when Bihar state approached NIMHANS for the DMHP capacity building, it was thought appropriate to use the VKN-ECHO model to overcome the barriers mentioned earlier. This article gives an overview of the implementation of this project titled “BLENDED TRAINING of Non-Specialist doctors for DMHP of BIHAR state.” This article describes a 1-year training program from June 2017 to May 2018 in which NIMHANS, Bengaluru, trained PCDs of Bihar (n = 22) and provides an overview of the impact of this training.
Methods
Participants
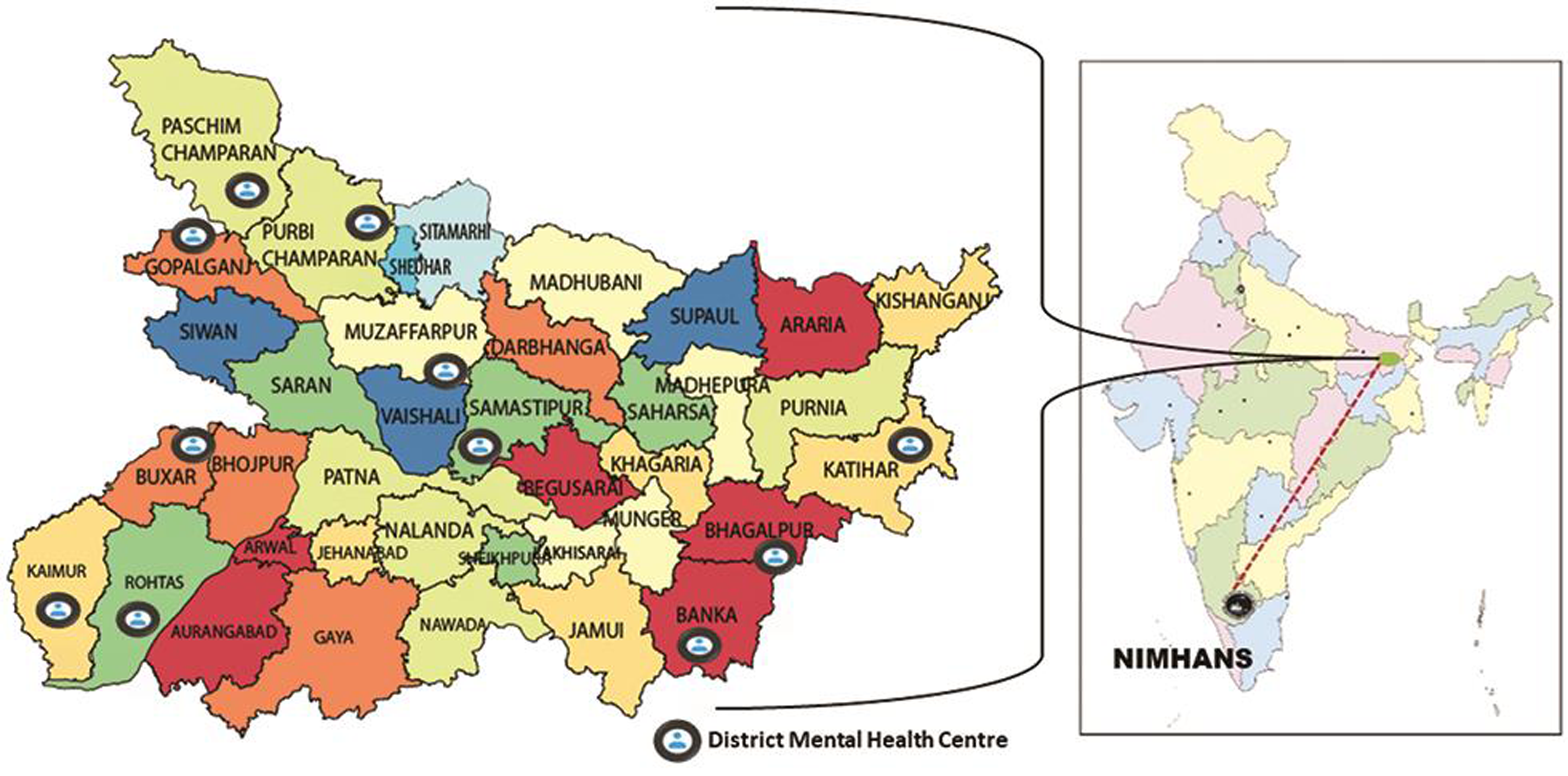
Nonspecialist MBBS medical officers from 11 districts of Bihar (Fig. 1) were nominated by their state health society to undergo DMHP training in order to enable them to provide basic mental health services at the district level. Two medical officers were nominated from each of the 11 districts from June 2017 to March 2018. These participants were MBBS graduates with no formal exposure to psychiatry and had either no or minimal clinical exposure to psychiatry. The course was a 10-month blended training module. Accreditation was provided to those members who fulfilled all the predetermined course completion criteria. Each participant was required to attend an onsite orientation program at NIMHANS for 2 weeks, maintain a minimum of 60% attendance for the online classes, and present six cases during the tele-ECHO clinics, as prerequisites for accreditation. Participation was voluntary but to be eligible for accreditation, participants were required to fill out one pretest before the onset of the training, and three posttests sent across the training duration, achieved at least 80% in each of the six assignments, and sent across monthly reports of psychiatric patients seen by them during the training period.
-
Fig. 1 Districts of Bihar connected to Virtual Knowledge Network, National Institute of Mental Health and Neuro-Sciences (VKN, NIMHANS).
Fig. 1 Districts of Bihar connected to Virtual Knowledge Network, National Institute of Mental Health and Neuro-Sciences (VKN, NIMHANS).
All participants were oriented about essential smartphone-based technology platforms. The technology platforms were easily accessible using either smartphones, tablets, or laptops.
Onsite training (n = 22) occurred at NIMHANS for 2 weeks wherein they were oriented to psychiatry and its practice. Participants were taken around various psychiatric facilities including outpatient services, inpatient services, specialty services, including child and adolescent psychiatry, emergency psychiatry and acute care, geriatric psychiatry, noninvasive brain stimulation, yoga, and related services. The daily routine consisted of the orientation tour in the morning and theory/practical (bedside clinics) classes during the afternoons. After completion of the onsite training, the participants felt confident of psychiatric history taking and conducting a brief mental status examination.
A tele-ECHO clinic was done prior to the start of the onsite training for needs assessment where the participants were allowed to express their requirements as per their place of work, topics of interest to them, and the expectations they had from the yearlong training. Accordingly, a curriculum was designed including topics such as screening for common and severe mental disorders, pharmacological and nonpharmacological approaches to mental health disorders, how to work with the family members or caregivers of the mentally ill, and brief overview of substance use disorders. Peer reviewing of the curriculum was done by experts in the field of mental health to ensure adequacy of content and quality. Substance use disorders were not covered in detail as there is a separate wing of addiction clinics running in each district of Bihar who have been trained on the ECHO platform by Center for Addiction Medicine experts from NIMHANS.13
Online Training
The online training sessions (virtual classrooms) were conducted using the Hub and Spokes model. The Hub (NIMHANS) consisted of a specialists’ team of psychiatrists (didactic speaker, facilitator, and moderator) and clinical psychologist with expertise in mental health services along with a distance learning coordinator, and an IT coordinator. Experts who were fluent in Hindi were involved in the training as this was the preferred language of the participants who were all from Bihar. A blended format for the online program was incorporated including both the synchronous and asynchronous aspects to the learning.
A pretest was administered by asking the participants to fill out a survey form before initiating the tele-ECHO clinics. Posttests included similar sets of questions and were repeated again in the third, sixth, and ninth month of the training. Prepost assessments tested the knowledge and skills instilled in the participating spokes. Additionally, the practice patterns were also quantified by noting down the number of patients seen, medicines dispensed, and referral patterns.
Invitations to participants including the agenda for the session were sent 3 days prior with a reminder sent 1 day prior to each of the online sessions. Besides email, WhatsApp was also used extensively for the purpose. A dedicated person for round the clock IT support was present for coordinating the tele-ECHO clinics. Any technology-related problems during the session or with the software used to give assignments or to load presentations was handled by the IT coordinator.
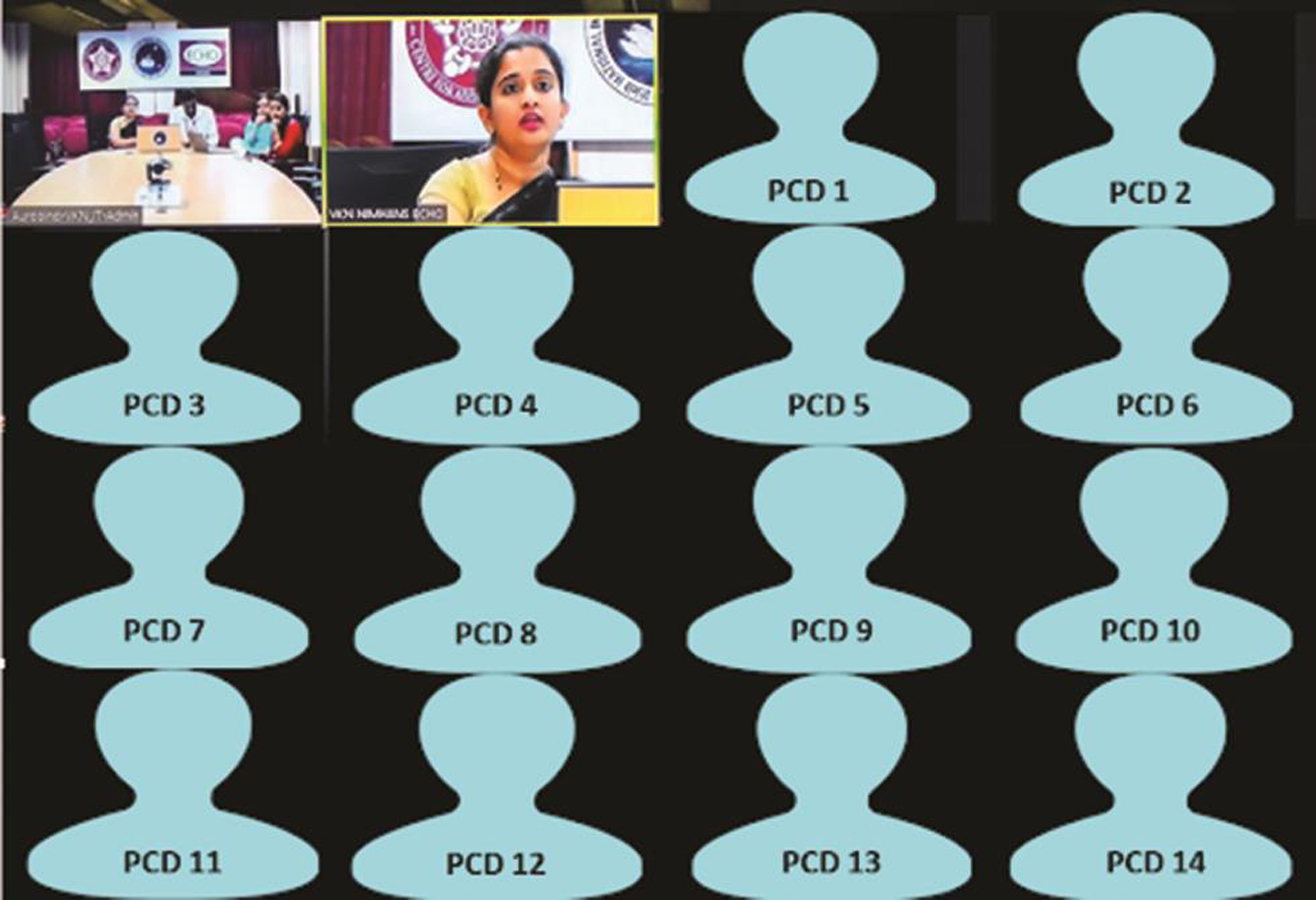
Online clinics were held fortnightly on every first and third Wednesday of the month from June ’17 to March ’18 that amounted to a total of 20 live interactive sessions. Each session consisted of a brief didactic presentation by a psychiatrist in English with translations in Hindi language when required. Every didactic was followed by case presentations from the participant spokes, which was then opened up for a peer-led discussion coordinated by the subject expert. This comprised the synchronous LIVE virtual tele-ECHO clinics (Fig. 2). Case recommendations were prepared by the psychiatrist for the cases discussed and learning points were added in it for future management that were sent to the participants through email and WhatsApp. For the asynchronous part of the learning, didactic presentations, additional reading materials, and case recommendations with specific learning points were shared with participants using Slido application14 as well as by mobile WhatsApp after every Tele-ECHO clinic.
-
Fig. 2 Snapshot of LIVE virtual tele-ECHO clinic. PCD, primary care doctor.
Fig. 2 Snapshot of LIVE virtual tele-ECHO clinic. PCD, primary care doctor.
Assignments
In order to regularly assess the knowledge and skills attained by the participants through this training, six assignments were provided to the participants. The assignments included the topics covered as per the predecided curriculum and included multiple choice questions. Case-based scenarios were also provided to check on the skills related to assessment and management of these patients. First two assignments were completed along with the pretest during the onsite program. Besides this, participants had to complete a total of four assignments at the end of every 2 months of the course based on the didactics and learning materials shared with participants. These were created and evaluated by the program experts to assess the knowledge level of the participants. Participants were expected to achieve a minimum score of 80% within five attempts in a 2-week time period in each assignment to be declared successful. These learning assignments were provided to the participants online through an LMS (learning management solutions) website, that is, talent LMS application.13
Results
Participant Demographics and Attendance
Eleven out of the total 38 districts were nominated to participate in this NIMHANS ECHO training program by the state health society, Bihar, from which 22 doctors from these 11 districts participated in the training and evaluation process. The other districts did not participate due to lack of initiation of DMHP programs in the other districts. Mean age of the participants was 44 and all were males. Nineteen participants (86.3%) had an MBBS degree with three (13.7%) of them having a postgraduate degree (ENT, pediatrics, and psychiatry). Six of the participants were also trained in addiction psychiatry from VKN NIMHANS Bihar Drug ECHO. Two of the participants had exposure to mental health through some brief training courses.
Over the 20 fortnight tele-ECHO clinics, 12 participants maintained more than 60% attendance. Reasons for dropping out were doctors were transferred to non-DMHP districts (n = 2) or left DMHP (n = 3) and some were involved in too many health programs and could not take time out for the sessions (n = 3), etc. Thirteen doctors continued to participate in the training program till the end. Average attendance from the participant spokes was 47.83% for all tele-ECHO clinics with around 10 of them connecting to every tele-ECHO clinic.
Satisfaction
Fourteen participants responded to the survey. Details are provided in Table 1.
|
Survey item |
Mean rating (out of 5) a |
|---|---|
|
aEach question rated on a 5-point Likert scale scoring from 1 to 5. |
|
|
How much has the tele-ECHO program increased my confidence in my clinical skills? |
4.615 |
|
How relevant and helpful was the course for me, professionally? |
4.308 |
|
How satisfied I am with the content of the tele-ECHO clinics? |
4.615 |
|
How satisfied I am with this form of training (onsite training + virtual sessions + WhatsApp support for 10 months) vs. more traditional forms of training? |
4.615 |
Thematic analysis of the qualitative feedback revealed the following.
The participants reported that their knowledge of psychiatry and its practice got enhanced through this training. Constant availability of the mentor (through phone or online calls) for case discussions improved their confidence and competence to deal with the patients. Since all participants are working in government hospitals with very high workloads, they had difficulty in finding time to attend the sessions. Though an official permission to attend the session was issued by the concerned authorities, these doctors had multiple roles to play that conflicted with time for the online sessions.
A few statements were as follows:
-
“The necessary and up to date practical and evidence-based information was provided’
-
“Role plays used in the session were useful in our training”
-
“Teaching style of the trainers was very good. They were responsible and always started training on time.”
Learning
All participants (n = 22) completed the pre- and posttests, including the 20 questions for knowledge assessment (Section 1). There was significant increase in “knowledge” from pretest scores of (9.6 ± 3.1) to final posttest scores (13.2 ± 4.4). Some of the participants required extra attempts to complete the assignment.
Self-Confidence
The section on perceived self-confidence and self-efficacy had 15 questions assessed on a 5-point Likert scale that focused on participant level of confidence and overall level of significance. Statistically significant increase in the mean scores from the pretest to the final posttest scores was noted at the end of blended training.
Performance: Case Discussions
In the 20 tele-ECHO clinics held, a total of 79 patients from the participants’ clinical practices were discussed in detail during tele-ECHO clinics. The cases were worked up by the participants in detail using a proforma provided by the expert team. Details regarding the diagnosis of the patients seen are mentioned in Table 2. These patients directly benefited from the case recommendations prepared by the NIMHANS hub team. In this way, best practices were translated into the community through these case-based learning sessions.
|
Cases discussed |
|
|---|---|
|
Substance use disorders |
2 |
|
Schizophrenia/psychosis |
28 |
|
Mood disorders |
18 |
|
Obsessive compulsive disorder |
10 |
|
Anxiety disorders |
18 |
|
Others |
03 |
|
Total |
79 |
At the end of the training, 11 doctors got accreditation from NIMHANS for successfully fulfilling all the course requirements.
During the 10 months of training, the participants continued to care for persons with psychiatric disorders in their clinics. A total of 2,3242 patients were seen by these 22 doctors during the period June 2017 to June 2018.
Discussion
This article gives a broad overview of the NIMHANS-VKN-ECHO blended training program conducted for PCDs from Bihar that enabled them to identify and treat common psychiatric disorders presenting in the community. Total of 11 doctors got accredited in this yearlong program. Not only their knowledge and attitude towards psychiatric practice improved, but they were also able to care for many patients in their communities who otherwise would have great difficulty accessing appropriate mental healthcare. The results demonstrate the feasibility of our blended training model. The success of our program has special significance. For countries such as India that faces severe shortages of trained mental health professionals to cater to the burgeoning public health menace of psychiatric illnesses. These kinds of programs can act as a model for many similar innovative methods of leveraging digital technology for capacity building in mental health. Many such programs are currently underway in NIMHANS covering the entire strata of society ranging from lay-volunteers, medical undergraduates, mental health professionals to medical officers. Programs consist of an online course for lay-counselors, certificate course in geriatric mental health for lay counselors, specialty-based training program for psychiatry post-graduates, and the National Medical College Network catering to undergraduate students across the country. Apart from these basic courses, certain advanced courses are also running like Foundation of Addiction14 and Tobacco Cessation.13
There are many other issues that need to be considered regarding such training programs. Training medical officers is not a new thing in India. Integrating mental health care into general health care is at the core philosophy of the National Mental Health Program15 (and its operational arm, the DMHP) and medical officers are being trained as part of National Mental Health Program for the last several decades. However, the effectiveness of these training programs is uncertain as is the data on the translational quotient of these programs. An important reason for this lack of success is the structure and format of traditional classroom teaching methods. Noninclusion of adult learning principles is another reason. Other well-known factors are a lack of adequate human resources, overburdened staff, and the lack of motivation among the existing staff. It is also proven that unless there is ongoing mentoring and guided practice, the acquired skills are bound to dissipate.12 In our program, participants received sustained mentorship and guidance over a period of 1 year, while they implemented their new knowledge in their practices. Future efforts should be geared toward continuing and sustaining the mentoring till adequate skills transfer is ensured. An effort has been made for the same in the current program by opening an e-consult platform called “Super Friday” where the accredited doctors send difficult cases from their practice for discussion a day prior and cases are discussed every Fridays by the expert multidisciplinary team from NIMHANS. In this way, patients are comanaged with experts and NIMHANS continues to guide and mentor these nonspecialist doctors to increase their confidence and competence in practicing psychiatry. Other than Super Friday, the 11 accredited doctors were enrolled into an advanced course—certificate course on schizophrenia that was a 3-month blended training course. They were also involved in other advanced courses offered by NIMHANS Digital Academy based on their interests and continued to do various courses opened up by the academy from time to time.
However, despite the above positive aspect, a sobering observation is that out of the 11 accredited, 5 have been transferred out of their DMHP responsibilities and given administrative work. This is an inevitable scenario in the government sector where there is a constant challenge to maintain an adequate number of trained work force, not just for mental health, but in all sectors. This issue is being tackled by increasing the number of medical institutes across the length and breadth of the country, though it will take some more years before we see the impact on the ground.
As regards the format and structure of the training per se, it is to be noted that nothing stops MBBS doctors from catering to psychiatric disorders. However, the undergraduate psychiatry curriculum (and thereby the training) is so inadequate that very few MBBS doctors care for psychiatric patients in India (without additional systematic training in psychiatry). In this sense, the entire 1-year program was designed so as to enable the nonspecialist doctors identify, diagnose, and treat uncomplicated common psychiatric problems presenting in community settings. During the discussions, referral criteria were also discussed so as to enable them to identify clinical scenarios that needed referral to a specialist.
Now that Internet technology is so easily available, has penetrated to large parts of India, and transformed our lives in many sectors, there is a great opportunity to use digital technologies for capacity building in mental health as well. In this direction, the NIMHANS Digital Academy16 has been initiated since June 2018 onwards and already hundreds of doctors, and many mental health professionals are trained and accredited. States such as Gujarat have started their own digital academies to exponentially increase trained manpower to cater to the mental health needs of their populations.
To conclude, we have demonstrated the design, feasibility, and acceptance of a digitally driven training program to build capacity in the field of mental health. Such models are extremely useful in this current pandemic of coronavirus disease 2019. However, more rigorous evaluation methods need to be employed to critically evaluate the impact of such programs. It is also important to focus on assessing patient level outcomes that are crucial and more important than the cursory measures as discussed in the article. We have already incorporated patient level assessments as part of the next project currently underway in the same state.
Conflict of Interest
None declared.
References
- NMHS Collaborators Group. The National Mental Health Survey of India (2016): prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int J Soc Psychiatry. 2020;66(4):361-372.
- [Google Scholar]
- The birth of national mental health program for India. Indian J Psychiatry. 2015;57(3):315-319.
- [Google Scholar]
- National mental health programme: manpower development scheme of eleventh five-year plan. Indian J Psychiatry. 2011;53(3):261-265.
- [Google Scholar]
- Shristi A. Mental Health in Bihar: Are We Listening? Working Paper 06/2018. Patna, Bihar: The Center for Health Policy
- Challenges of human resources management in changing Bihar: The way forward. International Journal of Human Resource Management and Research.. 2020;10(1):101-112.
- [Google Scholar]
- Mental health service availability and delivery at the global level: an analysis by countries’ income level from WHO’s Mental Health Atlas 2014. Epidemiol Psychiatr Sci. 2017;13(1):12.
- [Google Scholar]
- Expanding access to hepatitis C virus treatment–Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010;52(3):1124-1133.
- [Google Scholar]
- Digital technology and mental health interventions: opportunities and challenges. Arbor. 2015;191(771):210.
- [Google Scholar]
- Innovative telementoring for addiction management for remote primary care physicians: a feasibility study. Indian J Psychiatry. 2018;60(4):461-466.
- [Google Scholar]
- Designing and implementing an innovative digitally driven primary care psychiatry program in India. Indian J Psychiatry. 2018;60(2):236-244.
- [Google Scholar]
- Project ECHO (project extension for community healthcare outcomes): a national and global model for continuing professional development. J Contin Educ Health Prof. 2016;36(01):S48-S49.
- [Google Scholar]
- Improving the psychiatric knowledge, skills, and attitudes of primary care physicians, 1950-2000: a review. Am J Psychiatry. 2001;158(10):1579-1586.
- [Google Scholar]
- A pilot from the virtual knowledge network (VKN) NIMHANS ECHO. In: 2017 5th National Conference on E-Learning & E-Learning Technologies (ELELTECH). IEEE; 2017.
- [Google Scholar]
- An effort to improve students’ activeness at structure class using Slido app. JEES (J Engl Educ Soc). 2019;4(1):1.
- [Google Scholar]
- Profile of cases discussed in innovative tele-ECHO mentoring program on addiction management. Asian J Psychiatr. 2020;52:102060. (102060)
- [Google Scholar]
- National mental health program of India: a review of the history and the current scenario. Int J Community Med Public Health. 2016;3:2696-2704.
- [Google Scholar]






