Translate this page into:
Rehabilitation for cerebral palsy: Analysis of the Australian rehabilitation outcome dataset
Address for correspondence: Dr. Bhasker Amatya, Department of Rehabilitation Medicine, University of Melbourne Royal Melbourne Hospital, 34 - 54 Poplar Road, Parkville, Melbourne VIC 3052, Australia. E-mail: Bhasker.amatya@mh.org.au
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To examine the outcome of inpatient rehabilitation for cerebral palsy (CP), using the Australian Rehabilitation Outcomes Center (AROC) database.
Materials and Methods:
De-identified data from the AROC database was analyzed for all rehabilitation admissions during 2003 – 2008, using four classes for the functional level. The outcomes included: Functional Independence Measure (FIM) scores, FIM efficiency, hospital length of stay (LOS), and discharge destination.
Results:
Of 141 case episodes 56.7% were female, mean age 48.5 years, 87.2% were discharged to the community and 64.5% (n = 91) were in the lowest functional classes (217, 218, and 219). The majority of CP patients were treated in the public hospital system (66.7% versus 33.3%), and had a slightly longer LOS compared with those treated in private facilities (22.6 versus 17.9 days, mean difference - 4.7 days, 95% CI - 9.2 to - 0.2, P = 0.041). The FIM for all classes (216 – 218) showed significant functional improvement during the admission (P = 0.001). As expected those in the most functionally impaired classes showed most change (FIM change: 16.6 in class 217, 15.3 in class 218). FIM efficiency was the highest in classes 217 compared to the other classes. The year-to-year trend demonstrated a mixed pattern for hospital LOS and was not significant (P = 0.492).
Conclusion:
The AROC dataset is a valuable research tool for describing rehabilitation outcomes. However, more specific information needs to be collected alongside the core AROC data, to allow a more meaningful evaluation of outcomes for CP rehabilitation.
Keywords
Australian rehabilitation outcomes center dataset
cerebral palsy
function
hospital length of stay
measurement
outcomes
rehabilitation
Introduction
Cerebral palsy (CP) is an umbrella term referring to a range of motor disorders arising from a non-progressive defect or damage to the developing brain in a baby or infant.[12] The cardinal clinical feature of CP includes motor disorders, which range from minimal to profound, and are often accompanied by disturbances of sensation, perception, cognition, communication, behavior and / or seizure, which can greatly contribute to an overall disability.[3–6] Based on the neurological signs and motor function, CP has been further categorized into: Spastic, ataxic, and dyskinetics syndromes, and mixed forms.[6] The prevalence of cerebral palsy is approximately 2 – 2.5 cases per 1000 live births, which has remained relatively stable over the past six decades, despite significant advances in the medical care of neonates.[7]
Cerebral palsy is a chronic, irreversible condition and is neither progressive nor communicable.[68] The management of a person with cerebral palsy, with the objective of optimizing the person's ability to function, typically includes the input of many disciplines, including medical, physical therapy, occupational therapy, and speech and language therapy.[135]
Cerebral palsy remains a significant health problem. Persons with CP commonly have multiple symptoms and impairments such as weakness, spasticity, and lack of co-ordination, which restrict them in performing their normal daily activities.[4] There is no curative treatment that exists for CP and improving the ability to perform normal daily activities is often the primary therapeutic goal.[349] Multidisciplinary and multifaceted therapies can provide help and improve the quality of life for these people.[1] In addition to medication, orthopedic surgery, and orthotic devices such as braces and splints, can help improve their function and activities.[4]
There is now a substantial body of evidence to support the effectiveness of rehabilitation following CP, and the place for rehabilitation in CP is well-established among service planners and providers.[3568–12] Rehabilitation has the potential to reduce the care burden both for family and for society, and the associated costs of care, by improving independence and autonomy.[13]
Despite the availability of health service frameworks (National Services Framework, 2005)[14] that promote rehabilitation for persons with long-term neurological conditions (LTNC) such as CP; as also clinical guidelines and standards,[15–18] gaining access to the appropriate rehabilitation services continues to be a challenge[121920]. One reason for this is the relatively poor understanding of the specific benefits that may be derived from rehabilitation in the context of this neurological disease.[13]
Although randomized controlled trials are methodologically the 'gold standard' for the effectiveness of rehabilitation, they cannot answer all the questions that need to be answered.[21] Therefore, prospective data collected systematically in the course of a routine clinical practice has the potential to provide additional information about CP survivors that will assist in understanding the nature of services provided, as well as the outcomes and service implications. Practice-based evidence can be used to address critical questions, such as, which patients have the most to gain, and what models and intensity of rehabilitation input are likely to be most effective.[2223]
In Australia, the Australasian Rehabilitation Outcomes Center (AROC) holds a centralized database, which gathers a standard set of information on both the process and outcome, for every person admitted for inpatient (IP) rehabilitation. It has data for over 160 accredited Australian hospitals (public and private) over the last seven years. It provides a national benchmarking service, as well as provides information to improve the understanding of factors that influence the rehabilitation outcomes and costs. In a previous analysis, we have described the broad outcomes of rehabilitation in persons with multiple sclerosis (MS).[24] The objective of this study is to examine the AROC database for the first episode of IP CP rehabilitation, to understand the nature, outcomes, and service implications for CP survivors in Australia. The primary outcomes include improvement in patient functional status, hospital length of stay (LOS), and discharge destination. In addition the year-to-year trends in LOS and service efficiency have been examined, as well as comparison of outcomes for service provision between the public and private sectors. This analysis provides the types of information that can be obtained from such a dataset, and identifies the additional information needed to answer the critical questions for rehabilitation in CP survivors over the coming decade.
Materials and Methods
AROC dataset and ANSNAP classes
The Australasian Rehabilitation Outcomes Center was established in 2002, as a joint initiative of the Australasian Rehabilitation sector (providers, payers, regulators, and consumers), although development of the dataset started in 1999. The dataset comprises of case episode data of admissions for rehabilitation from participating services across Australia (currently there are > 400,000 episodes of care from 165 rehabilitation units in Australia [90 public and 75 private facilities]). The AROC dataset includes 42 items: Sociodemographic, medical (impairment codes, comorbidities, complications), episode items (admission dates), funding and employment details, and outcome data (patient level of function at admission and discharge).[1425] The proportion of missing data in the AROC dataset items for 2003 – 2008 is available from authors.
The Australian National Subacute and Non-Acute Patient (ANSNAP) casemix classification system was designed for sub and non-acute care, recognizing that such patients should be classified by treatment goals, such as, improvement in function, rather than by diagnosis and procedure.[14] The case episode data is therefore subdivided based on both diagnosis and functional level, using the Functional Independence Measure (FIM).[26] In 2007, the ANSNAP version II[25] was implemented, to reflect the clinical and demographic profile of patients who receive IP rehabilitation, and include the addition of more defined diagnostic classes for neurological impairment groups (such as CP) to ensure consistency in the allocation of patients. Similar to other neurological impairment groups the specific ANSNAP II classes for CP are categorized based on a functional level using a motor score of the FIM. These include:
-
216 (FIM motor (m) scores range 63 – 91)
-
217 (FIM m = 49 – 62)
-
218 (FIM m = 18 –48), and
-
219 (FIM m = 14 – 17)
The Australasian Rehabilitation Outcomes Center holds a territory license for use of the FIM™1 in Australia and New Zealand, and is the national certification and training center for this tool for all accredited rehabilitation facilities (public and private). Clinical staffs are required to complete FIM training, and must take a credentialing exam every two years. These procedures maximize the quality of data. All data received by the AROC are screened for errors and missing data, and if necessary the submitting facility is requested to review and correct any inconsistencies.
Note: 1FIM™ is a trademark of the Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities, Inc.
Data handling and statistical analysis
De-identified data for CP survivors, for the first episode of IP rehabilitation, during the six-year period between 2003 and 2008, were extracted from the main AROC database, cleaned, and transferred to the SPSS version 15 for analysis. Missing and small sample data were excluded from the analysis as indicated in Box 1. Descriptive analysis included the mean and 95% confidence intervals (CI) for demographic, FIM, LOS, and discharge destination, collated by year, ANSNAP class, and sector / provider type. Significant differences were tested by independent sample t-tests and between the subjects' ANOVA with post hoc pairwise comparisons using Bonferroni adjustments for significant ANOVA results. Given the large sample size, the effect sizes (Cohen's d) were calculated for each t-test to provide an indication of the magnitude of each effect.
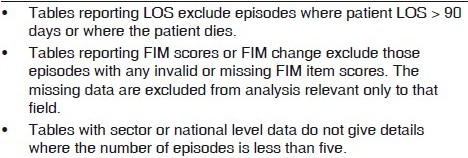
- Exclusions from AROC
Results
A total of 141 first episodes for CP IP rehabilitation were submitted to AROC during the study period (2003 – 2008) and included in the analysis below. For functional class 219 only one episode was reported.
Differences between ANSNAP classes
Patient demographic split by the ANSNAP class are provided in Table 1. Approximately 87.2% (n = 123) were discharged into the community, with only 12.8% (n = 18) remaining in the hospital system. The majority of admissions (46.1%) were in the lowest functioning class (218), with only 17.7% (n = 25) in class 217. However, some interesting patterns emerge:
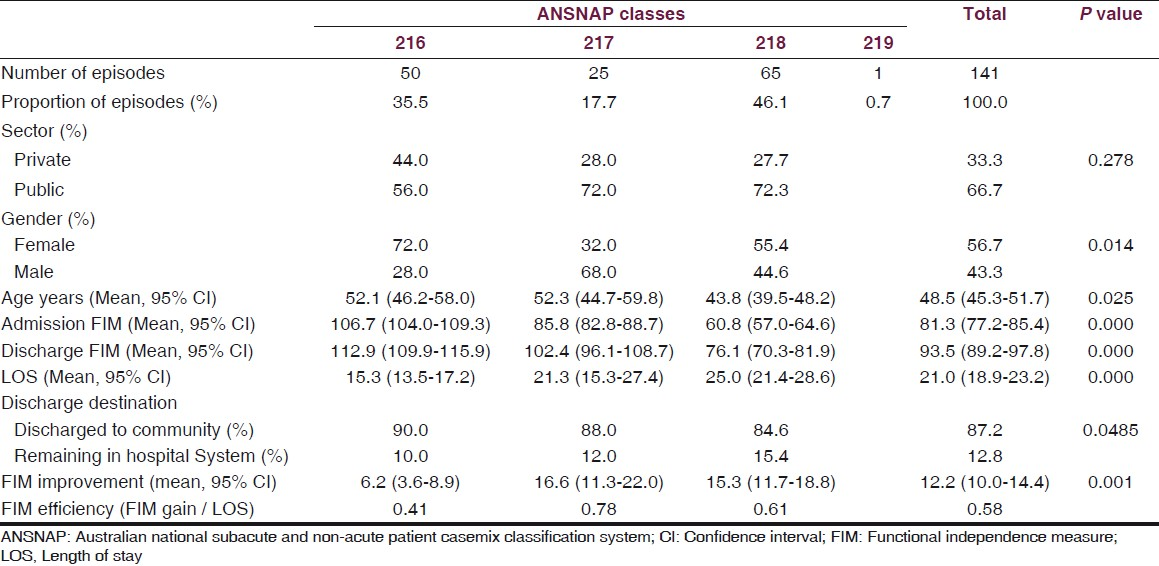
Gender
Overall there were more female patients (56.7%), with more females in the highest functioning class 216 (72.0%) and lowest functioning class 218 (55.4%). However, in class 217, there were predominantly male patients (68.0%).
Age
There were significantly younger patients in the lowest functioning class, 218, compared to other classes (P = 0.025)
Public versus private sector
Although in each ANSNAP class the majority of cases were treated in the public health sector (66.7%), this trend became more pronounced in the two lowest functioning classes (217 and 218). However this was statistically not significant (P = 0.278)
length of stay
LOS increases progressively with loss of function across the three classes, ranging from 15.3 days in class 216 to 25.0 days in class 218 (mean 21.0 days, 95% CI 18.9 to 23.2, P < 0.001).
All the ANSNAP classes from 216 to 218 showed significant improvements in FIM scores from admission to discharge [Table 1]. The FIM improvement differed between the three ANSNAP classes, 217 had a significantly greater improvement in FIM scores compared to class 216 (mean FIM change 16.6 vs. 6.2, P = 0.001). However, although the admission FIM scores for class 218 were the lowest compared to the other classes, the FIM improvement was not as marked as for class 217 (15.3 vs. 16.6). A majority of patients were discharged to their usual accommodation in the community (range 84.6 to 90.0%), however, those in class 218 with greater functional impairments were not able to return to their accommodation. FIM efficiency was higher in the middle classes 217 than in classes 216 and 218, probably due to the floor and ceiling effect of FIM.
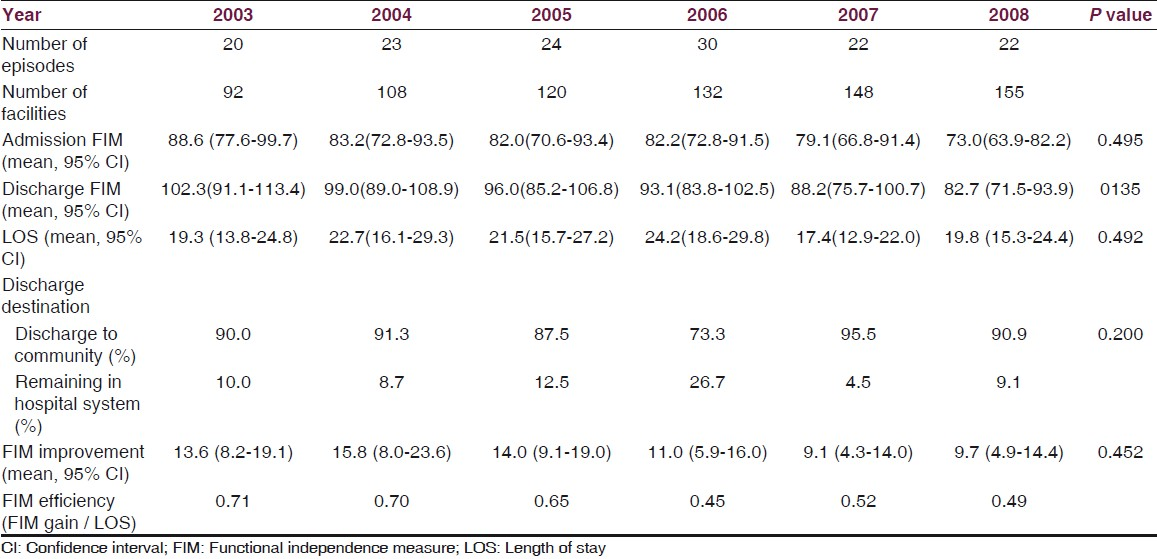
Year-to-year comparisons
Interestingly, although the facilities reporting to AROC grew substantially over the data collection period from 20 in 2003 to 155 in 2008, the number of cases reported per year remained consistent throughout this time period (ranging from 20 to 30). The ratio of episodes per facility did not change substantially between 2003 and 2008. Table 2 shows there were no significant changes in the number of episodes per facility, LOS, discharge destination, FIM change or efficiency, year by year.
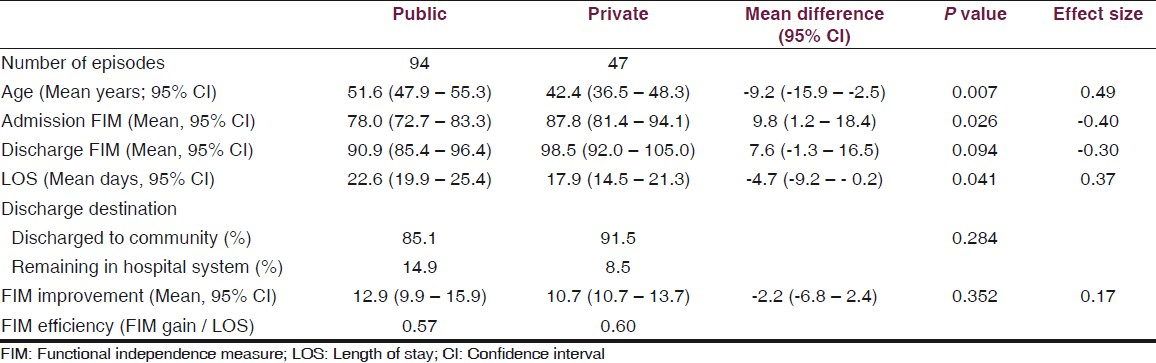
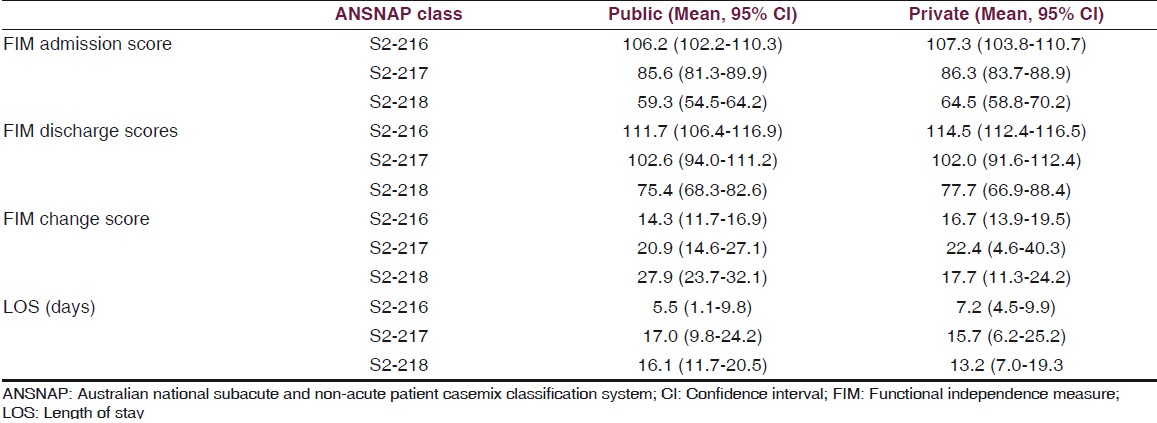
Comparison of private and public services
Overall, the LOS was longer for patients treated in the public sector (22.6 days) than the private sector (17.9 days) (mean difference = - 4.7, 95% CI - 9.2 to - 0.2, P < 0.041, d = 0.37) [Table 3]. FIM improvement was slightly higher in those treated in the public sector compared to the private sector, but was statistically not significant (12.9 vs. 10.7, mean difference= - 2.2, 95% CI - 6.8 to 2.4, P = 0.35, d = 0.17). A vast majority of patients from the private sector were discharged to their usual residence in the community compared to the public health sector (91.5 vs. 85.1%, P = 0.28). Approximately 14.9% of the patients remained within the public hospital system, presumably due to greater patient complexity. Within each ANSNAP class the LOS between the private and public sectors is shown in Table 4. The most functionally impaired class, 218, had the greatest difference, with almost three days longer for the public sector compared to the private sector. However, the FIM change achieved during that longer LOS was higher (12.9 vs. 10.7).
Discussion
This is the first report on the outcomes of IP rehabilitation (first episode only) for patients with CP (N = 141) using a national dataset. Persons with CP require IP care if their functional dependency is high and / or they need 24-hour nursing (e.g., optimization of medication dosage, functional mobilization or task reacquisition programs). The aim of this preliminary article is to describe CP rehabilitation outcomes including improvement in patient functional status, process measures (LOS, discharge destination) and comparison of these outcomes in public versus private facilities. Similar to the previous reports of rehabilitation on the outcomes for persons with MS[24] Guillain-Barre syndrome (GBS)[13] and Parkinson's disease,[27] the vast majority of persons with CP returned to their usual accommodation in the community, however, 23.4% stayed within the hospital setting (private and public) unable to be discharged home due to greater disease severity. Most patients with CP were in the lower functioning ANSNAP class 218, with only less than 1% in the very disabled class (ANSNAP 219). Similar to MS survivors,[24] overall, there were more female patients. However, females were predominant in the higher ANSNAP functioning class 216 and lower ANSNAP class 218, whereas, in the ANSNAP class 217 male significantly outweighed their female counterparts.
Overall, patients with CP stayed longer in public hospitals, as expected, and many were treated within the public sector. This is in contrast with reports for persons with PD,[27] who are primarily treated in the private hospital system. In Australia there is universal health care, so all persons with CP can access the public hospital system. Within this there are no penalties for longer stayers or any relationship between physician renumeration and type or length of stay and so on. A number of persons with CP (usually children) may not have concurrent private insurance cover, which may have restricted them from using private facilities. Their social class and family income status were beyond the scope of this study.
There was an increase in the number of rehabilitation centers contributing to the AROC database over the years, but there were no significant changes year-to-year, in terms of the number of episodes, LOS, or discharge destination, except in FIM change and efficiency. The LOS in public hospitals was longer compared to the private facilities; however, this was not statistically significant.
The results of this report confirm reduction in the disability and functional gains (measured with FIM) made by persons with CP after rehabilitation. Patients in all ANSNAP classes made functional gains, however, as expected, those in the middle disabled classes (ANSNAP 217 and 218) improved the most. These results are similar to the previous AROC reports for persons with MS[24] and GBS survivors.[13] Those in class 217 had more than two-and-a-half folds of FIM score improvement compared with those in class 216 (mean FIM improvement 16.6 vs. 6.2). These gains in function translate to reduction of care needs of approximately 30 – 60 minutes per day, to offset costs of treatment, based on reports from a large US database.[26] More detailed description of the FIM motor scores for all ANSNAP classes will be presented in a separate report.
As reported previously,[132427] the originators of FIM (uniform data systems), use the FIM efficiency as a marker for cost efficiency, benchmarking, and outcomes of rehabilitation research. The floor and ceiling effects of the FIM scale, its ordinal nature, and separate motor and cognitive domains scores do not lend themselves to the total summation scores nor manipulation such as division by LOS, to derive measures for efficiency. Other studies[28] show that FIM efficiency does not indicate cost efficiency outside the middle range for more dependant patients. Further information is needed to examine if the differences reported here are clinically meaningful for patients with CP. Other factors impacting outcomes such as the cost implications of CP care are beyond the scope of this study.
The usefulness of the AROC dataset depends on trained accredited staff and submission of accurate data, which is resource intensive. The year-on-year data shows a reduction in the missing data, but other data fields have information that is difficult to interpret clinically (such as time of onset). Information about patient functional dependency is available, however, other information not currently collected includes:
-
Type of treatment
-
Range of co-morbidities and complications
-
Range and severity of neurological, cognitive impairments
-
Type of treatment provided that is ‘black box’ (disciplines involved, intensity of treatment, key intervention)
-
Outcomes relating to participation and community reintegration.
(Note — the AROC ambulatory dataset has commenced data collection in 2009)
These issues indicate the complexity of the need for rehabilitation and the expected outcomes. In addition to the AROC dataset, additional disease-specific (CP) datasets can be recorded alongside for a more informative comparison. These should include more detailed information about the co-morbid conditions and other concurrent disabilities in persons with CP. With the commencement of the AROC ambulatory dataset, the follow-up data on patients discharged can be recorded. No information is available for variables such as the race and cultural context of the patients' lives or availability of healthcare resources, which may have the potential for modifying the impact of the disease on the overall QOL in CP patients.
Compared to MS, Parkinson's disease, and GBS population, most patients with CP are younger and complex, and the treatment requires a long-term process by a multidisciplinary team, focusing on all developmental aspects and planning interventions in relation to the most urgent needs of the patient and the family.[2] The optimal goal of the rehabilitation program usually is not to attain normalcy or cure, but to develop key areas of improvement including physical movement and coordination, speech, vision, and intellectual and cognitive development, social interaction, and independence.[12]
The number of adults with CP is increasing because of increased survival of low birth weight infants and increased longevity of the adult population, which impose an economic burden, not only on the person with the condition and their care givers, but also on the health system and society,[127] There is no mainstay treatment for patients with CP and the types of treatment depend on the patient's specific symptoms.[1] Therefore, a co-ordinated multidisciplinary approach focusing on total patient development, which encompasses pharmacological and surgical treatments and supportive rehabilitation therapies, may address the many disabling symptoms associated with CP.[112]
This study provides useful information on the outcomes of CP rehabilitation. The results of this study can be generalized to a wider population of patients with CP, as the data contains a wider population-based sample from across Australia. All rehabilitation facilities (public and private) in Australia submit their data to AROC as part of their accreditation — this study therefore captures all patients who have received the first episode of IP rehabilitation for CP during the study period. The instrument used (FIM) is valid and reliable; and the results are clinically relevant in this patient group. Despite the limitations in using FIM (mentioned earlier), it remains the most widely used instrument for outcome measurement and reimbursement in the Australian health care system.
In conclusion, the AROC dataset is a unique resource and a valuable research tool for describing rehabilitation outcomes in ‘real life settings’. However, more specific CP information needs to be collected alongside the core AROC data for a more meaningful evaluation of the outcomes of CP rehabilitation. This study contributes to an improved understanding of the outcomes of IP rehabilitation for people with CP, in Australia. Further comparative analysis of these results with other CP cohorts is now needed.
We thank The Australasian Faculty of Rehabilitation Medicine, The Royal Australasian College of Physicians for permission to analyze the AROC database; and Prof. L Turner Stokes, T Stevermuer, and F Simmonds for their assistance in the data analysis.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Pediatric Rehabilitation in Children with Cerebral Palsy: General Management, Classification of Motor Disorders. J Prosthet Orthotics. 2002;14:143-9.
- [Google Scholar]
- Occupational therapy for children with cerebral palsy (Protocol) Cochrane Database Syst Rev 2003:CD004490.
- [Google Scholar]
- Acupuncture for children with cerebral palsy (Protocol) Cochrane Database Syst Rev 2008:CD007127.
- [Google Scholar]
- Speech and language therapy to improve the communication skills of children with cerebral palsy. Cochrane Database Syst Rev 2003:CD003466.
- [Google Scholar]
- Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy. Cochrane Database Syst Rev 2007:CD004149.
- [Google Scholar]
- Access Economics Pty Limited. The Economic Impact of Cerebral Palsy in Australia in 2007. In: Canberra. Australia: Cerebral Palsy Australia; 2008.
- [Google Scholar]
- Ambulatory physical activity performance in youth with cerebral palsy and youth who are developing typically. Phys Ther. 2007;87:248-57.
- [Google Scholar]
- Muscle strengthening for children and adults with cerebral palsy (Protocol) Cochrane Database Syst Rev 2009:CD007971.
- [Google Scholar]
- Effects of constraint-induced movement therapy on hand skills and muscle recruitment of children with spastic hemiplegic cerebral palsy. Neurorehabilitation. 2009;24:95-108.
- [Google Scholar]
- A systematic review of the effectiveness of treadmill training for children with cerebral palsy. Disabil Rehabil. 2009;31:1971-9.
- [Google Scholar]
- International perspectives on paediatric rehabilitation-Australia. Pediatr Rehabil. 2004;7:267-70.
- [Google Scholar]
- Rehabilitation for Guillain Barre syndrome: Analysis of the Australian rehabilitation outcomes dataset. J Clin Med Res. 2010;2:91-7.
- [Google Scholar]
- The Australian National Subacute and Nonacute patient classification (ANSNAP): Report of the National Subacute and Nonacute Casemix Classification Study. NSW 1997
- [Google Scholar]
- The Royal Children's Hospital. Clinical Practice Guidelines: Cerebral Palsy. February 2006. Available from: http://www.rch.org.au/clinicalguide/cpg.cfm?doc_id=5165#intro
- [Google Scholar]
- Practice parameter: Diagnostic assessment of the child with cerebral palsy: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2004;62:851-63.
- [Google Scholar]
- National Institute for Health and Clinical Excellence. Interventional procedure overview of selective dorsal rhizotomy for spasticity in cerebral palsy. London, UK: NICE; 2009.
- [Google Scholar]
- The Physician's Guide to Caring for Children with Disabilities and Chronic Conditions. USA: Paul H. Brookes Publishing Co; 2000.
- [Google Scholar]
- Can strength training predictably improve gait kinematics.A pilot study on the effects of hip and knee extensor strengthening on lower-extremity alignment in cerebral palsy. PhysTher. 2010;90:269-79.
- [Google Scholar]
- Rehabilitation of neuromuscular disturbance: Summary of round table discussion. Pediatrics. 1957;20:165-9.
- [Google Scholar]
- Traumatic brain injury rehabilitation: Are there alternatives to randomised controlled clinical trials? Arch Phys Med Rehabil. 2002;83:1320-2.
- [Google Scholar]
- Another look at observational studies in rehabilitation research: Going beyond the holy grail of the randomized controlled trial. Arch Phys Med Rehabil. 2005;86:S8-15.
- [Google Scholar]
- Opening the black box of post-stroke rehabilitation: Stroke rehabilitation patients, processes, and outcomes. Arch Phys Med Rehabil. 2005;86:S1-7.
- [Google Scholar]
- Multiple Sclerosis Rehabilitation Outcomes: Analysis of a National Casemix Dataset from Australia. Mult Scler. 2009;15:869-75.
- [Google Scholar]
- The development of Version 2 of the ANSNAP casemix classification system. Aust Health Rev. 2007;31:S68-78.
- [Google Scholar]
- Functional assessment scales: A study of persons with multiple sclerosis. Arch Phys Med Rehabil. 1990;71:870-5.
- [Google Scholar]
- Rehabilitation for Parkinson's Disease: Analysis of the Australian rehabilitation outcomes dataset. J Clin Med Res 2010
- [Google Scholar]
- Efficiency of specialist rehabilitation in reducing dependency and costs of continuing care for adults with complex acquired brain injuries. J Neurol Neurosurg Psychiatry. 2006;77:634-9.
- [Google Scholar]






