Translate this page into:
Primary Sacral Hydatid Cyst Mimicking a Neurogenic Tumor in Chronic Low Back Pain: Case Report and Review of the Literature
Address for correspondence: Dr. Manuel Segura-Trepichio, Department of Orthopedic Surgery, Vinalopó University Hospital, 03203 Elx/Elche, Alicante, Spain. E-mail: manusegura5@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hydatid disease is caused by infection of Echinococcus granulosus. Bone hydatid cyst presentation without hepatic affectation is infrequent and occurs in 0,5-2% of cases. This rare condition makes clinicians not always aware of the disease, and as a result, misdiagnosis of spinal echinococcosis is common. We present a case of a 48-year-old female patient with primary sacral hydatidosis. Chronic low back pain radiating to the left buttock was the only symptom. The magnetic resonance imaging (MRI) suggested a neurogenic tumor versus giant cell tumor. Biopsy and pathological study revealed a hydatid cyst. Anthelmintic and surgical treatment was performed. At 12 months after surgery, the patient is free of recurrence. In patients with chronic low back pain and a MR suggestive of neurogenic tumor, spinal hydatid cyst should be considered in the differential diagnosis. It is recommended the assistance of an anesthesiologist during biopsy to avoid an anaphylactic shock.
Keywords
Echinococcosis
giant cell tumor of bone
hydatid disease
low back pain
spinal cord neoplasms
INTRODUCTION
Hydatid disease (HD), also known as cystic echinococcosis, is caused by infection with the larval stage of Echinococcus granulosus.[1] The disease has the highest incidence in countries where sheep are raised with the help of dogs. In endemic regions, human incidence rates for HD can reach >50/100,000 person-years, and prevalence levels as high as 5%–10% may occur in parts of East Africa, Central Asia China, Argentina, and Peru.[2] The adult tapeworm, which inhabits the small intestine of dogs, produces eggs which contain the larval tapeworm (oncosphere). Eggs excreted in the feces are dispersed widely in the environment. Intermediate hosts (sheeps and humans) become infected by accidental consumption of water or food that has been contaminated. Oncospheres penetrate the intestine and are carried through bloodstream where they are filtered out in various organs.[3] The most common hydatid cyst sites in humans are the hepatic filter, 60%–70% of cases, followed by lung and brain. Bone hydatid cyst presentation without hepatic affectation is infrequent and occurs in 0,5-2% of cases, half of which infest the spine.[4] Primary involvement of the sacral spine, as in the current case, is very rare.
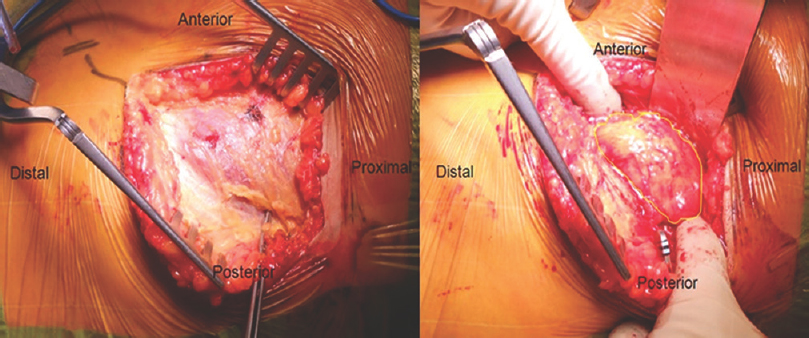
The first case was described in 1951.[5] Since then, few cases have been reported in literature [Table 1]. As a result, sacral hydatid cyst (SHC) is characterized by clinical latency, late diagnosis, and therapeutic difficulties. We document diagnosis and treatment of a patient with a primary SHC and is compared with other cases published in literature.
CASE REPORT
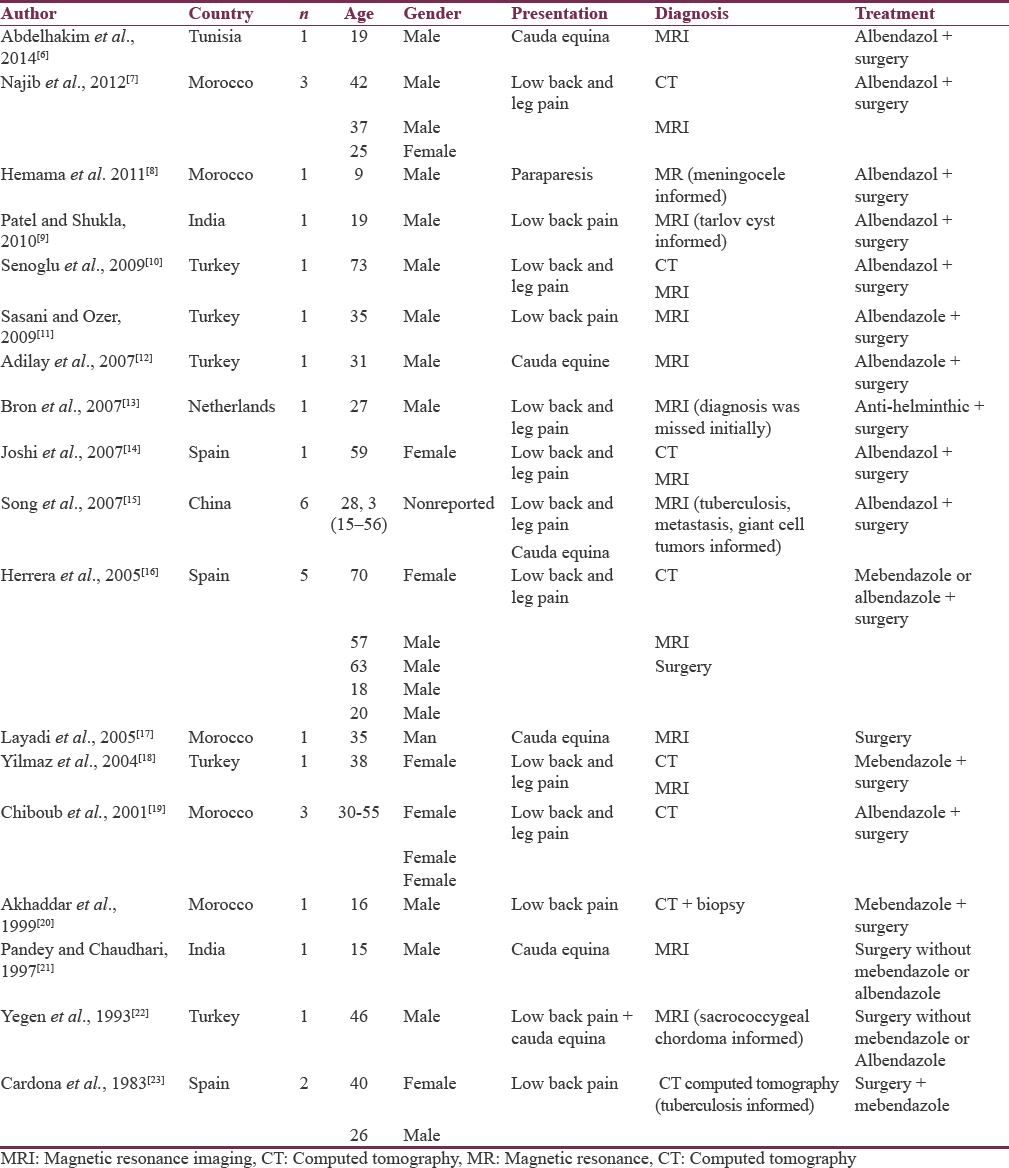
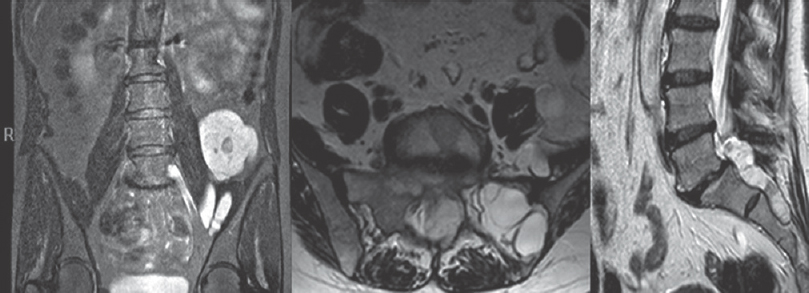
A 48-year-old woman from South Mediterranean region was admitted at our center because of low back pain radiating to the left buttock. She had no improvement with analgesia and physiotherapy for a year. Neurological examination showed no motor, sensory, patellar, or Achilleian reflexes’ deficits, and no bladder disorders. The patient had a lumbar radiography without abnormalities. The magnetic resonance (MR) revealed a cystic lesion with cerebrospinal fluid-like signal in contact with left sacral roots extending through sacral holes reaching iliac muscle [Figure 1]. The MR image suggested, as the first option, a neurogenic tumor (sacral neurofibroma or schwannoma), as the second, giant cell tumor (GCT) or chordoma. After consultation with radiologists and pathologists, a computed tomography-guided biopsy was performed with an 11-gauge bone access needle. During biopsy, a greenish-yellow aspirate was obtained. Pathological study revealed hydatid cysts presence, with an inner germinal layer, surrounded by an outer layer of chitin [Figure 2]. Specific enzyme-linked immunosorbent assay (ELISA) serological tests proved negative. Before surgery, treatment with oral albendazole (400 mg/12 h) and praziquantel (100 mg/8 h) for 2 months was given to the patient.
- Magnetic resonance T2-short-tau inversion recovery. Coronal, axial, and sagittal planes. Cystic lesion with cerebrospinal fluid-like signal in contact with left sacral roots extending through sacral holes reaching iliac muscle
- Hydatid cyst (cyst wall, inner germinal layer) (H and E, ×200)
Surgical treatment was performed using a dual approach to the lumbosacral spine.
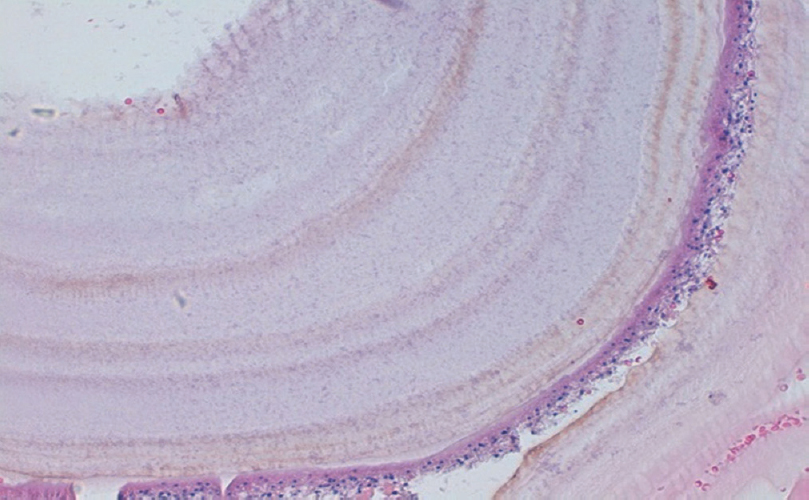
First stage: Ilium anterior approach, dissecting external oblique, internal oblique, and transversus abdominis. The cyst extended to the psoas muscle and left sacral foramens [Figure 3]. During dissection of the cyst, the wall was broken and the operating field was irrigated with hypertonic saline (7.2% NaCl).
- Ilium anterior approach, dissecting external oblique, internal oblique, and transversus abdominis after which the hydatid cyst was found
After the anterior approach, the patient was prepared for the second posterior spine approach to remove the sacral root origin of the sacral cyst [Figure 4]. Lumbopelvic instrumentation and bone grafting (femoral head) to fill the bone defect in the sacrum were added [Figure 5].
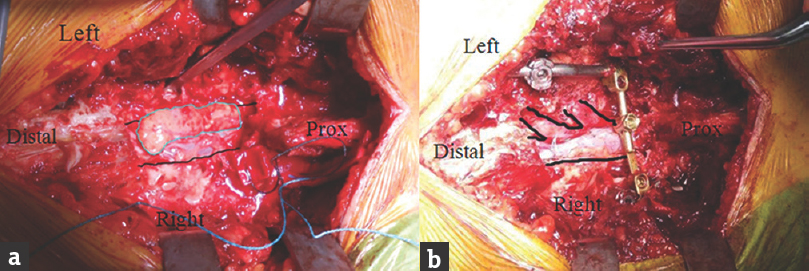
- Posterior approach. (a) Hydatid cyst (highlighted in blue) on top of the dural sac. (b) First and second left sacral roots, after removing the hydatid cyst (highlighted in black)
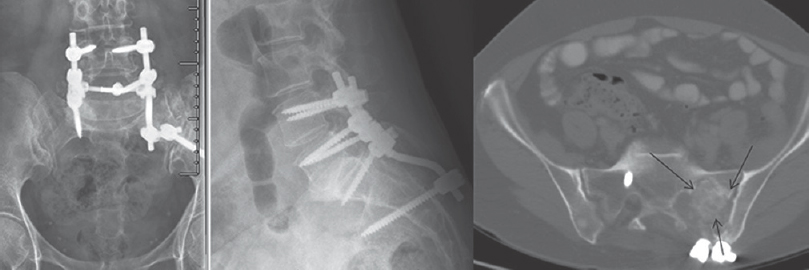
- Lumbopelvic instrumentation and bone grafting (femoral head) to fill the bone defect in the sacrum (highlighted with black arrows)
The patient continued treatment with albendazole (400 mg/two times a day) and praziquantel (40 mg/kg day) 3 months after surgery. At 12 months after surgery, the patient is free of symptoms and is complete autonomous for performing the basic activities of daily living.
DISCUSSION
Misdiagnosis of sacral echinococcosis in MR is common [Table 1].
In the present case, MR suggested a sacral neurogenic tumor. Neurofibromas, or schwannomas, can grow through the neural foramens outward from the sacral canal, and a giant mass may form anterior to the sacrum. Ogose et al. reported a presacral schwannoma with purely cystic form with similar MR characteristics to a SHC.[24] On MR, benign schwannomas have smooth tumoral margins and are isointense with muscle on T1-weighted images and hyperintense on T2-weighted images.[25] In SHC, MR shows a cystic lesion with similar characteristics to cerebrospinal fluid with a thin peripheral enhancement after contrast administration. The sacral hydatid cyst (SHC) capsule is best seen on T2- and proton density-weighted images.[2627]
Hemama et al. reported a SHC as a meningocele on MR.[8] Anterior sacral meningocele is a protrusion of the meninges through a defect in the anterior aspect of the sacrum into the retroperitoneal space. This lesion is seen with equal signal intensities of cerebrospinal fluid on all MR sequences and is usually unilocular.[28]
Song et al. mistook a SHC with a GCT on MR.[15] The most common GCTs site is distal femur and proximal tibia in 50%–65%, but can affect sacrum in 4%–9% of cases.[29] The MR T2-weighted images show a heterogeneous high signal with areas of low-signal intensity (variable) due to hemosiderin or fibrosis. High signal in adjacent bone marrow thought to represent inflammatory edema.[30]
Yegen et al. reported a SHC as a sacrococcygeal chordoma on MR.[22] The sacrum is the most common location, accounting for approximately 30%–50% of all chordomas.[31] Because chordomas lie in bone, they are usually extradural and induce bone destruction. In the MR, destructive lytic lesion with expansile soft-tissue mass can help distinguish chordoma from SHC.
We must be very careful with the SHC biopsy. Puncture of the cyst could cause the migration of parasites to the bloodstream causing an anaphylactic shock; hence, the assistance of an anesthesiologist during biopsy is recommended.[32]
The indirect hemagglutination test and the ELISA serology is 80%–100% sensitive and 88%–96% specific for liver cyst infection, but less sensitive for lung involvement (50%–56%) or other organs (25%–56%).[33] In the present case, the serological tests were negative. Other tests, such as immunodiffusion and immunoelectrophoresis, provide specific confirmation after a positive ELISA serology, and they were not used in this patient.[34]
Although medical treatment can decrease the size of cysts, the definitive treatment is complete surgical removal of the cyst.[3] There are several antiparasitic treatment alternatives; however, the most effective therapy appears to be the combination of albendazole + praziquantel rather than albendazole alone.[3536]
CONCLUSION
In patients originating from endemic areas of HD, with chronic low back pain and an sacral MR suggestive of neurogenic tumor, meningocele, chordoma, or GCT, sacral spinal HD should be considered in the differential diagnosis. Treatment with surgery and albendazole + praziquantel is effective for removal of the cysts.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2016. Echinococcosis Fact Sheet No. 377. World Health Organization; March. http://www.who.int/mediacentre/factsheets/fs377/en/
- Unusual locations of hydatid cysts. Ann Gastroenterol Hepatol (Paris). 1995;31:295-305.
- [Google Scholar]
- Hydatid bone disease of the pelvis. A report of two cases and review of the literature. Clin Orthop Relat Res. 1992;280:251-5.
- [Google Scholar]
- Hydatidosis of the pelvic bone: Case report and review of the literature. Eur J Orthop Surg Traumatol. 2012;22(Suppl 1):239-44.
- [Google Scholar]
- A sacral hydatid cyst mimicking an anterior sacral meningocele. J Neurosurg Pediatr. 2011;8:526-9.
- [Google Scholar]
- Combined anterior and posterior approach for sacral/retroperitoneal hydatid cyst disease: Case report. Turk Neurosurg. 2009;19:428-32.
- [Google Scholar]
- Spontaneous drainage of an asymptomatic recurrent hydatid cyst of the sacrum. Spine (Phila Pa 1976). 2009;34:E269-71.
- [Google Scholar]
- Cauda equina syndrome caused by primary lumbosacral and pelvic hydatid cyst: A case report. Minim Invasive Neurosurg. 2007;50:292-5.
- [Google Scholar]
- Long term follow-up of a patient with disseminated spinal hydatidosis. Acta Orthop Belg. 2007;73:678-82.
- [Google Scholar]
- Primary sacral epidural hydatid cyst: A case report. J Radiol. 2005;86(9 Pt 1):1040-2.
- [Google Scholar]
- Primary hydatid disease of sacrum affecting the sacroiliac joint: A case report. Spine (Phila Pa 1976). 2004;29:E88-90.
- [Google Scholar]
- Echinococcosis of the pelvic bone: Four cases. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:397-401.
- [Google Scholar]
- Primary hydatid cyst of sacral spinal canal: Case report. Neurosurgery. 1997;40:407-9.
- [Google Scholar]
- Sacrococcygeal hydatid cyst: Another entity in the differential diagnosis of sacrococcygeal chordoma. Case report. Paraplegia. 1993;31:479-81.
- [Google Scholar]
- 2 cases of vertebral hydatidosis treated by the association of surgery and mebendazole. Rev Chir Orthop Reparatrice Appar Mot. 1983;69:69-74.
- [Google Scholar]
- Hydatidosis of the pelvic bone: Case report and review of the literature. Eur J Orthop Surg Traumatol. 2012;22(Suppl 1):239-44.
- [Google Scholar]
- A sacral hydatid cyst mimicking an anterior sacral meningocele. J Neurosurg Pediatr. 2011;8:526-9.
- [Google Scholar]
- Successful management of a giant anterior sacral meningocele with an endoscopic cutting stapler: Case report. J Neurosurg Spine. 2016;24:862-6.
- [Google Scholar]
- From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: Radiologic-pathologic correlation. Radiographics. 2001;21:1283-309.
- [Google Scholar]
- Mimics on radiography of giant cell tumor of bone. AJR Am J Roentgenol. 2003;181:1583-9.
- [Google Scholar]
- Anaphylactic shock caused by nonruptured hydatid cyst of the liver. J Gastrointest Surg. 2008;12:2243-5.
- [Google Scholar]
- Primary spinal extradural hydatid cyst in a child: Case report and review of the literature. Eur Spine J. 2002;11:500-3.
- [Google Scholar]
- Immunodiagnosis of Echinococcus infections: Confirmatory testing and species differentiation by a new commercial Western blot. J Clin Microbiol. 2000;38:3718-21.
- [Google Scholar]
- Combined albendazole and praziquantel versus albendazole alone in the treatment of hydatid disease. Hepatogastroenterology. 1998;45:1690-4.
- [Google Scholar]
- The effect of combination therapy with albendazole and praziquantel on hydatid cyst treatment. Parasitol Res. 2008;103:195-9.
- [Google Scholar]






