Translate this page into:
Primary Paraspinal Hydatidosis Causing Acute Paraplegia
Address for correspondence: Dr. Srihari Sridharan, Institute of Neurosurgery, Madras Medical College, Park Town, Chennai - 600 003, Tamil Nadu, India. E-mail: sriharisridharan@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The zoonotic infection hydatidosis is caused by the tapeworm cestode, Echinococcus granulosus. Though considered endemic in India where association of humans with sheep and dogs form part of the livelihood, primary skeletal muscle involvement of the disease is an extremely rare event. We report a case of primary paraspinal hydatidosis with extradural extension causing acute paraplegia. Excision of the cyst and decompression of the cord was done along with albendazole therapy. Paraspinal hydatid disease is a rare entity, and in regions where hydatid disease is endemic, it can be involved in the differential diagnosis of acute compressive myelopathy. Although antihelminthic chemotherapy forms the mainstay of the treatment, surgical intervention forms a major part of the management.
Keywords
Hydatid disease
paraspinal hydatid disease
vertebral hydatidosis
zoonosis
INTRODUCTION
Hydatidosis is caused by the tapeworm cestode, Echinococcus granulosus. Poor awareness, difficulty in access to clean potable water, intermingled lives of people with livestock, and infrequent veterinary care make this disease an endemic in India. Humans contract the disease by direct contact or feco–oral route. Theoretically, the disease can occur anywhere in the body other than teeth, hair, and nails. Primary paraspinal skeletal muscle involvement is extremely rare, with an incidence of <1%.[1] We report such a case having intraspinal extradural extension and acute paraplegia which was surgically treated.
CASE REPORT
A 64-year-old female farmer from rural parts of Southern India presented with slow-growing painless swelling in the midback for 15 years. It became painful for the past 1 month with rapidly progressing weakness of lower limbs and urinary sphincter dysfunction for 1 week. Examination showed a nontender, firm, 15 cm × 10 cm, oval left paramedian mass from T8 to L3 with normal overlying skin without cough impulse, pulsations or mobility [Figure 1]. Neurological examination revealed a flaccid paraplegia with hypoesthesia below T6. Abdominal, patellar, ankle reflexes were absent. Plantar reflex was equivocal. Magnetic resonance imaging (MRI) revealed encapsulated multiple thin-walled cystic lesions without septations, hypointense in T1-weighted imaging (T1-WI), hyperintense in T2-WI in the left erector spinae muscle, invading the intraspinal space through the D8 neural foramina with erosion of D8, and hypointense lesion in the intraspinal extradural space from D8 to D12 causing compression of lower dorsal spinal cord/conus and cauda. The cystic lesions were surrounded by hypointense areas in T2-WI [Figure 2]. These features were suggestive of hydatid cyst. Further, radiological investigations ruled out other regions of the body harboring hydatid cyst. Albendazole 800 mg twice daily was initiated, and posterior midline approach was planned for surgery. Ten percent povidone-iodine soaked pads were used as scolicidal agent, and meticulous surgical technique followed to avoid any untoward rupture and leakage of cyst. The dumbbell-like nature of the lesion makes in situ, en bloc removal prone to rupture with resultant contamination of tissues. The cyst in the left erector spinae was delineated all around, opened with due precautions and daughter cysts were removed [Figure 3]. The cyst was found to erode D8 and through the neural foramina, invaded intraspinally. D7–D10 laminectomy was carried out, and extirpation of unruptured cyst was done [Figure 4]. Histopathological confirmation of hydatid cyst was done [Figure 5]. Albendazole (15 mg/kg/day) was advised for 3 months. Sensory modality recovered on 3 months follow-up with no motor and bladder recovery.

- The mass in the left paraspinal region
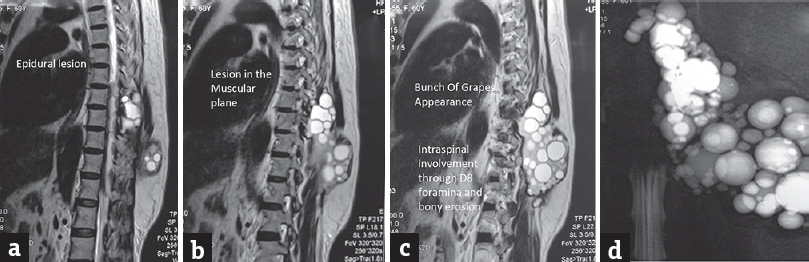
- (a-c) Magnetic resonance imaging showing “bunch of grapes appearances” of hydatid cyst in the paraspinal muscle entering the D8 neural foramina and extradural hypointense lesion, (d) myelographic image
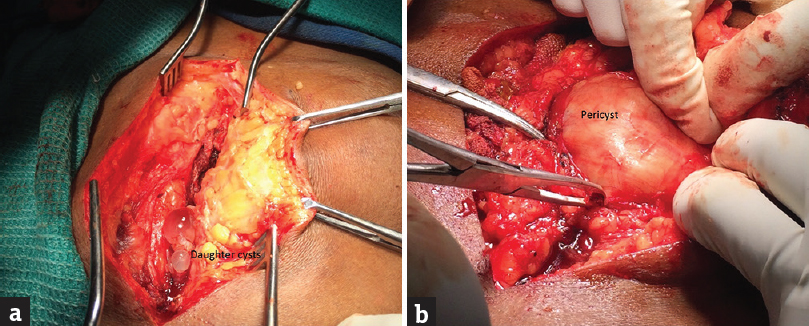
- (a) Cyst in the paraspinal muscles, (b) delineation of erector spinae, and the pericyst
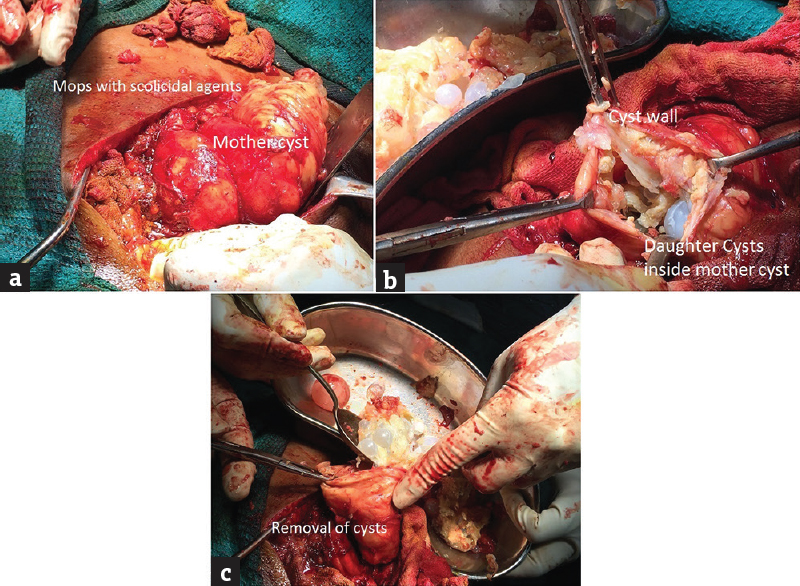
- (a) Povidone-iodine soaked pads around mother-cyst, (b) opening of cyst, (c) removal of shiny, pearly white daughter cysts
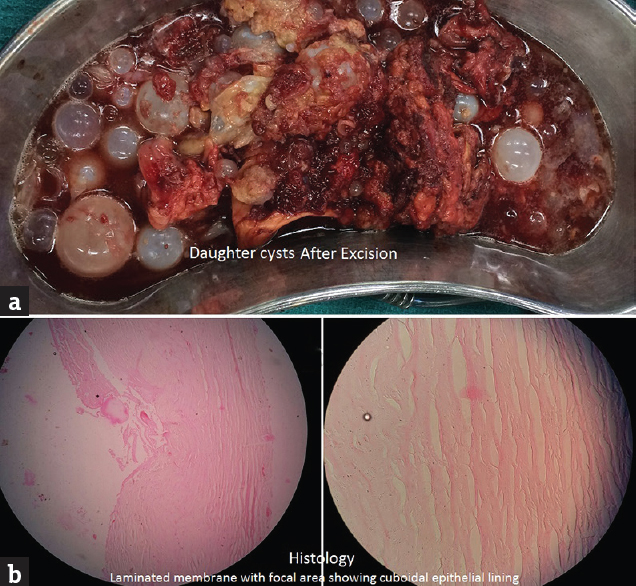
- (a) Gross pictures of cysts, (b) cyst wall with laminated eosinophilic membrane
DISCUSSION
In the life cycle of echinococcosis, humans are intermediate hosts, dogs being the definitive host and most common source of infection. Farming in India involves working with hands in soil and contact with livestock. Contamination of soil with infected dog feces and subsequent ingestion could have triggered the disease in our patient. The cysts are then transported from the intestinal wall through the blood stream. Liver (80%) and lungs (10%) form the focus of the disease as they are the major filters of the body. Spinal/paraspinal focus is rare. Radiologically, spinal hydatidosis is classified into intramedullary, intradural extramedullary, extradural intraspinal, vertebral, and paravertebral.[2] Neumayr et al. have divided them into intradural-extramedullary, extradural-extraosseous, and osseous. It also reports a dumbbell type which is paravertebral, extradural, and extraosseous with anterior extension.[3] Ours can be termed as a dumbbell variety with paraspinal and intraspinal involvement. Pain, pathological fracture, and deformity are the presenting features in a primary bony disease.[4] A slowly progressive swelling with a recent onset of pain and paraplegia puts in more evidence toward a primary paraspinal disease invading the intraspinal space in our case. The pathology of skeletal muscle involvement is poorly understood. Muscular contractions and the high lactic acid turnover are considered unsuitable for the cysts’ survival. Most cases of muscle hydatid disease have a primary of lung or liver.[5] There have been reports of hydatid disease of gluteal, neck, spinal, and rectus muscles.[56] Sener et al.[7] proposed that the parasite penetrates the intestinal muscle and enters the inferior vena cava through venous plexus between this system and portal circulation. Then, the parasite reaches the retroperitoneum, vertebral and paravertebral structures through lumbar epidural venous plexus.[8] The growth of the cysts is usually slow ranging from 5 to 20 years before causing symptoms. Symptoms manifest depending on the site and mass effect. Spinal involvement leads to a mortality of 50% on an average of 5 years after symptom onset.[9] MRI is preferred for delineating the neural structures and the extent of disease though bony involvement is better seen in computed tomography Scan. The cysts are hypointense on T1-WI images, hyperintense on T2-WI without contrast enhancement. Ours had the characteristic “bunch of grapes” appearance on MRI.[8] The various serologic tests available are usually not helpful in spinal hydatid disease. The treatment involves medical and surgical management. Small cysts can be managed medically, but rarely seek medical care particularly in lower socioeconomic group. Decompression of the spinal canal with complete resection of the cyst whenever possible forms the mainstay of surgical intervention in such cases for permanent eradication. Reydellet holds the credit for the first surgical intervention for spinal hydatidosis in 1819.[3] Intraoperative use of scolicidal agents though controversial[3] is widely used to avoid recurrence and anaphylaxis. Chemotherapy with mebendazole/albendazole is to be given postoperatively for at least 3 months.[10] Hydatidosis is a preventable disease. Education of the rural public on hygiene such as washing hands and food items such as vegetables before eating and improving awareness regarding zoonotic infections in disease prevalent areas can help in containing the disease. Easy access to medical care and seeking early medical care can stop a preventable disease from becoming a surgical one.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Primary cervical paraspinal hydatid cyst: A case report. J Neurol Sci. 2011;28:97-100.
- [Google Scholar]
- Spinal cystic echinococcosis – A systematic analysis and review of the literature: Part 2. Treatment, follow-up and outcome. PLoS Negl Trop Dis. 2013;7:e2458.
- [Google Scholar]
- Vertebral echinococcosis: Report of case of surgical and biological therapy with review of the literature. J Neurosurg. 1964;21:647-59.
- [Google Scholar]
- Diagnosis and management of hydatid cyst of the central nervous system. Neurosurgery. 2001;11:1-9.
- [Google Scholar]
- Primary sacral epidural hydatid cyst: A case report. J Radiol. 2005;86(9 Pt 1):1040-2.
- [Google Scholar]
- A lasting solution is hard to achieve in primary hydatid disease of the spine: Long-term results and an overview. Spine (Phila Pa 1976). 2004;29:932-7.
- [Google Scholar]
- Combined medical and surgical treatment of spinal hydatid disease: A case report. J Neurol Neurosurg Psychiatry. 1982;45:927-30.
- [Google Scholar]






