Translate this page into:
Paraspinal extramedullary hematopoiesis masquerading as nerve sheath tumor
*Corresponding author: R. T. Rajeswarie, Department of Laboratory Medicine, Sakra World Hospital, Bengaluru, Karnataka, India. raji.thiru9@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rajeswarie RT, Rudrappa S, Hosthota A, Deepthi VS. Paraspinal extramedullary hematopoiesis masquerading as nerve sheath tumor. J Neurosci Rural Pract 2023;14:355-7.
Abstract
Paraspinal tumors are uncommon tumors involving the soft-tissue around the vertebrae. The lesion could originate from nerve roots, soft tissue, or blood vessels. The diversity of the lesions poses diagnostic dilemma, warranting robust histopathological diagnosis. We report such a case presenting with radicular pain due to paraspinal extramedullary hematopoiesis (EMH) masquerading as nerve sheath tumor. EMH is presence of hematopoietic tissue outside the bone marrow. EMH is usually seen as a compensatory mechanism associated with underlying hematological disorder. Our case presented primarily as paraspinal mass without underlying hematological disorder on evaluation. Thus, recognizing that EMH can present as paraspinal mass even without a diagnosis of pre-existing hematological disorder is crucial.
Keywords
Paraspinal
Extramedullary hematopoiesis
Hematological disorder
INTRODUCTION
Paraspinal tumors are rare neoplasms presenting as soft-tissue mass that comes into contact with a part of vertebral column. Paraspinal soft-tissue mass may be caused by developmental anomalies, inflammatory disorders, degenerative processes, and neoplasms.[1] The diversity of these lesions in the paraspinal region pose challenge to the clinicians, radiologists, and pathologists. Although the differential diagnosis can be narrowed down by extensive clinical and radiological examination in most cases, final histopathological examination plays a key role in accurate diagnosis and further management. We report such a case of radicular pain due to paraspinal extramedullary hematopoiesis (EMH) without a known underlying hematological disease masquerading as nerve sheath tumor.
CASE REPORT
Our patient is a 50- year old gentleman, who presented with pain in the back with radiation to lateral aspect of the chest on the left side for 2 months, which aggravates with cough with visual analog scale score of 7/10. There is no restriction of daily activities. On examination, there is no evidence of any neurocutaneous markers or local tenderness. The neurological examination was normal.
Imaging showed isolated D9−D10 level extraforaminal lesion, which is non-homogeneous, hypointense on T1, hyperintense on T2 and STIR, no extension of the lesion into the neural foramen, and the spinal canal [Figure 1a and b].
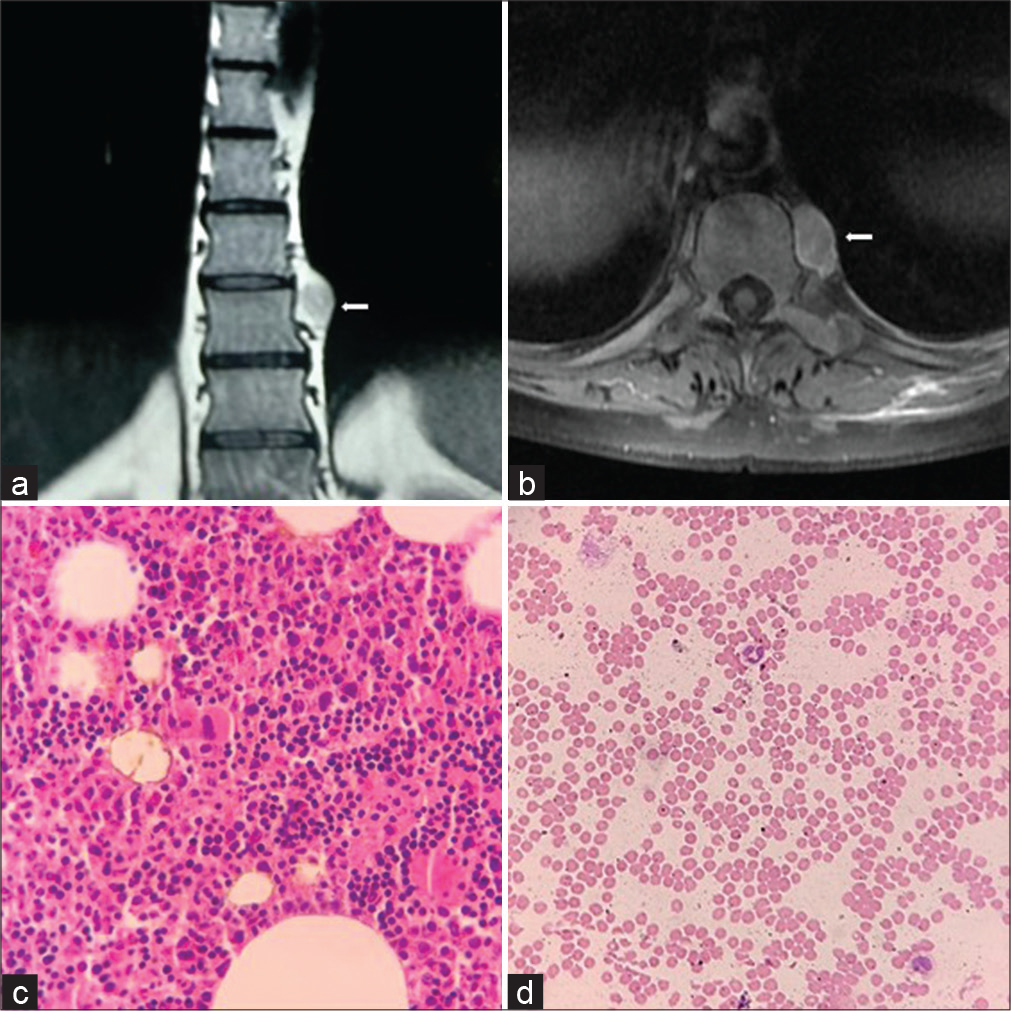
- Magnetic resonance images of thoracic spine lesion. Coronal section – lesion at the left paraspinal D9–D10 disk level (a), axial T2 – hyperintense with minimal vertebral scalloping (b), histomicrograph images of extramedullary hematopoiesis – cellular trilineage hematopoietic elements composed of erythroid, myeloid, and megakaryocytes (c), and normal peripheral smear (d).
The patient underwent left-sided D10 transthoracic approach for resection of the lesion. The lesion was firm, reddish vascular located adjacent to the sympathetic plexus with clear lesion, and tissue plane.
Histological examination revealed cellular trilineage hematopoietic elements composed of erythroid, myeloid, and megakaryocytes admixed with focal aggregate of small lymphocytes and plasma cells. Fat spaces were seen in between. There is no metastatic deposit or lymphoma or myeloma infiltration. Overall morphological features are compatible with EMH [Figure 1c and d].
Further hematological work up was done. Complete hemogram showed hemoglobin 11.2 gm/dL with normal differential count. Peripheral smear showed normocytic normochromic red blood cells, no evidence of target cells, tear drop cells, or spherocytes. No evidence of hemolysis seen. Leucocytes show normal distribution, no evidence of myeloid shift. Platelets are normal. There is no evidence of pancytopenia or marrow suppression. Hemoglobin and serum electrophoresis was within normal limits.
No evidence of hepatosplenomegaly on ultrasound of abdomen. The patient shows symptomatic improvement post-decompression with relief of pain. The patient is on hematological follow-up.
DISCUSSION
Paraspinal tumors often involve major nerve roots, major blood vessels, and other vital structures around the vertebral column. Benign neurogenic tumor and soft-tissue sarcoma compose the majority of the neoplasms in this location.[2] EMH is defined as the presence of hematopoietic tissue outside the bone marrow.[3] is defined as the presence of hematopoietic tissue outside the bone marrow. During fetal development, it is a physiological phenomenon in the liver, but after birth, it is pathological response, due to ineffective erythropoiesis in underlying hematological disorders.[4] It is a compensatory phenomenon due to insufficient bone marrow function that becomes unable to meet circulatory demands.[5]
EMH is believed to be associated with regaining of function through the vascular connective tissues at times of crisis.[6] EMH has been reported to occur in many parts of the body, especially liver, spleen, and lymph nodes. Paraspinal location warrants special attention due to close proximity to spinal cord and spinal nerves, compression of which causes neurological symptoms. First case of paraspinal EMH was report in 1954 by Gatto et al.[7] Paraspinal occurrence is seen in 11−15% of EMH.[8] Thoracic spine is the most commonly involved site of paraspinal EMH. There is limited mobility due to the narrow subarachnoid space at this location and early presentation due to spinal compression. The development of neurological symptoms is probably dependent on the chronicity of the lesion; thus, the usual presentation is in third or fourth decade. The size and site of the lesion determines the severity and acuteness of presentation.[9]
The early detection is essential to avoid irreversible neurological deficit. Most of the previous reports of paraspinal EMH presents with underlying hematological disorders, mainly thalassemia. Our case initially presented with symptomatic thoracic paraspinal mass which leads to diagnosis of EMH and evaluation of underlying anemia. Histological examination played an important role in further management of this case.
Paraspinal EMH with known underlying hematological disorder can be treated with blood transfusion and/ or radiotherapy and chemotherapy with hydroxyurea. Laminectomy is reserved for acute presentations. Extensive work up for hematological disorders is essential before considering conservative medical management of these lesion. EMH can be either active lesion with trilineage hematopoiesis or inactive ones with fat replacement or iron deposition due to oxidative stress.[3] Surgical treatment can be replaced with radiotherapy/chemotherapy in vulnerable/ inoperable locations. These lesions can be vascular, leading to catastrophic intraoperative bleed, especially the active ones.
However, this protocol cannot be followed in unsuspected cases with initial local compression symptoms simulating a nerve sheath tumor. Radiologically, the diagnostic dilemma occurs in solitary active lesion particularly in older individual without known hematological disorder.[3] Such patients warrant histopathological confirmation of the lesion to rule out metastasis, lymphomas, or multiple myelomas. Our present case is a similar one with symptomatic elderly male with unilateral, solitary active lesion without any known preexisting hematological disorder.[10]
CONCLUSION
Paraspinal lesions with underlying hematological disorder are usually evaluated with a differential diagnosis of EMH, and further, conservative medical or surgical treatment is based on imaging or biopsy of those lesions. However, surgical decompression and morphological evaluation are performed on unsuspected solitary active lesions masquerading as nerve sheath tumors. Thus, recognizing that EMH can present as paraspinal mass even without a diagnosis of pre-existing hematological disorder is crucial for the treatment plan and further hematological evaluation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Paraspinal mass with multiple differential diagnosis-a case report. JMSCR. 2018;6:201-4.
- [CrossRef] [Google Scholar]
- Anatomic classification system for surgical management of paraspinal tumors. Arch Surg. 2004;139:262-9.
- [CrossRef] [PubMed] [Google Scholar]
- Paraspinal extramedullary hematopoiesis in patients with thalassemia intermedia. Eur Spine J. 2010;19:871-8.
- [CrossRef] [PubMed] [Google Scholar]
- Thalassaemia intermedia: Revisited. Blood Cells Mol Dis. 2006;37:12-20.
- [CrossRef] [PubMed] [Google Scholar]
- Extramedullary paraspinal hematopoiesis in thalassemia: CT and MRI evaluation. Eur J Radiol. 1999;30:33-8.
- [CrossRef] [PubMed] [Google Scholar]
- Compression of the spinal cord due to proliferation of bone marrow in epidural space in a splenectomized person with Cooley's disease. Haematologic. 1954;38:61-76.
- [Google Scholar]
- Thalassaemia intermedia: An update. Mediterr J Hematol Infect Dis. 2009;1:e2009004.
- [CrossRef] [Google Scholar]
- Spinal cord compression in beta thalassemia: Case report and review of the literature. Spinal Cord. 2004;42:117-23.
- [CrossRef] [PubMed] [Google Scholar]
- Ectopic extramedullary hematopoiesis: Evaluation and treatment of a rare and benign paraspinal/epidural tumor. J Neurosurg Spine. 2013;18:236-42.
- [CrossRef] [PubMed] [Google Scholar]






