Translate this page into:
Primary amoebic meningoencephalitis
Address for correspondence: Dr. Gentle Sunder Shrestha, Department of Anaesthesiology, Institute of Medicine, Tribhuvan University Teaching Hospital, Maharajgunj, Kathmandu, Nepal. E-mail: gentlesunder@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Primary amoebic meningoencephalitis (PAM) is an acute, fulminant and rapidly fatal central nervous system (CNS) infection caused by a thermophilic ameboflagellate Naegleria fowleri.[1] Infection commonly occurs in healthy children and young adults with a history of recent exposure to warm fresh water in ponds, swimming pools and man-made lakes, but older people are also affected. Infection is usually acquired during swimming or nasal irrigation by contaminated water. PAM is clinically indistinguishable from bacterial meningitis. Diagnosis is made by examination of cerebro-spinal fluid (CSF) wet mounts for motile trophozoites.[2] In recent years, the number of cases reported have increased, probably due to greater awareness of disease or due to development of more rapid, highly sensitive and specific diagnostic tests.[3] About 300 cases have been reported so far with high case fatality rate of around 95%.[4] There has been advances in understanding of pathophysiology of this grave disease. Many therapeutic options have been tried, but with variable success and evidences are limited to small case series.[56789] For the first time, we are reporting a case of PAM in Nepal. The patient died despite intensive multi-drug therapy. A 51-year-old gentleman weighing around 50 kg, fisherman by occupation, presented with headache, vomiting, abnormal behavior and irrelevant talking of 4 days duration. Cerebrospinal fluid (CSF) opening pressure was 380 mmH2O. On CSF analysis, total cell count was 800/mm3 with 82% neutrophils, sugar was 20.5 mg/dL and protein was 171 mg/dL. Corresponding serum sugar was 156 mg/dL. There were no red blood cells (RBCs) seen. With the provisional diagnosis of bacterial meningitis, intravenous Ceftriaxone 2 gm twice daily was started. Gram staining and culture of CSF were negative for bacteria. There was progressive deterioration in neurological status and the patient was intubated for fall in Glasgow Coma Scale (GCS) score to 7/15. CT scan of head was unremarkable. Detail review of the case revealed his hobby of swimming and his recent history of exposure to fresh water of river about a week before his illness. Lumbar puncture was repeated on day 4 of presentation to hospital. CSF was cloudy and slightly hemorrhagic with 300 RBCs/mm3. Wet mount direct microscopic examination of the centrifuged sample revealed motile amoebae [Figure 1]. The trophozoites were approximately 10-14 μm in size and contained a nucleus with a large karyosome. Enflagellation test was performed by adding 0.5 mL CSF to 2 mL distilled water on a sterile flat-bottom plate and was incubated at 37°C. Microscopy done at 15 minute intervals revealed amoebae moving in a distinctive flagellar pattern.
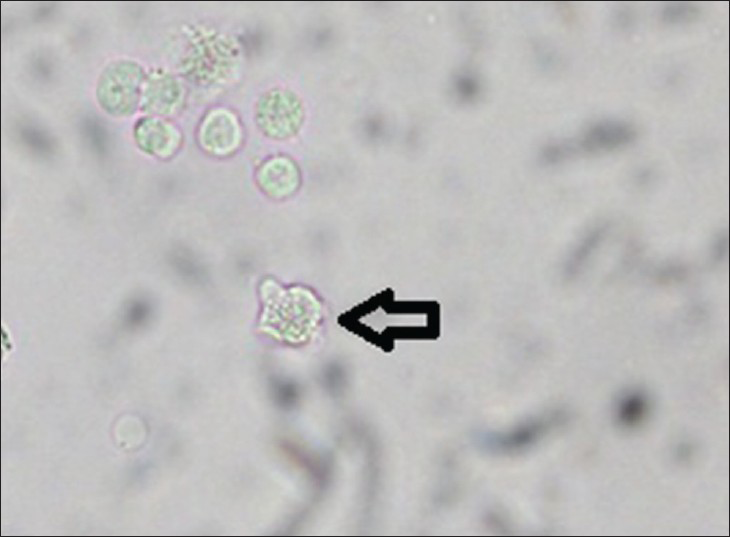
- Trophozoite of Naegleria fowleri seen during direct microscopy (indicated by arrow)
Ceftriaxone was stopped and the patient was started on Amphotericin B 50 mg iv daily. Intrathecal Amphotericin B was administered through a lumbar drain at 1.5 mg daily for 2 days and then 1 mg on alternate days for 8 days. Dexamethasone was administered 8 mg intravenously 8 hourly for 4 days. The patient was also administered Azithromycin 500 mg daily, Rifampicin 600 mg daily, Fluconazole 400 mg daily and Miltefosine 150 mg daily (in three divided doses) by the enteral route. CSF analysis was repeated at the end of intrathecal Amphotericin B therapy (on day 10 of multi-durg therapy) which showed turbid CSF with 1250 RBCs/mm3. Gram staining and culture was negative for bacteria, but the wet mount of centrifuged sample showed persistence of amoebae in CSF. Multi-drug therapy was continued, but neurologic status continued to deteriorate. On 16th day of hospital admission, he lost his brain stem reflexes and was declared dead.
PAM is a rapidly progressive disease that generally results in death within 5 to 10 days of symptom onset.[5] A majority of the infections occur after swimming in water naturally heated by sun. Lumbar puncture for CSF analysis is the primary diagnostic tool. Like in this case, CSF mimics acute bacterial meningitis except that gram stain is negative. Till date, there are only a few reported survivors. In those patients, infection was recognized promptly and managed with intravenous and intrathecal Amphotericin, variably coupled with other agents.[26]
After confirming the diagnosis, our patient was started on intravenous and intrathecal Amphotericin B in the dose suggested by Siedel et al., in a survivor from California.[6] Rifampin, fluconazole and dexamethasone was administered as suggested by a successful case report form Vargas-Zepeda et al.[2] Study in animal models has shown synergistic activities of Azithromycin with Amphotericin B.[7] So, Azithromycin was used as a part of regimen. Miltefosine was successfully used to treat disseminated Acanthemoeba infection.[8] So we included it as a part of our treatment. Similar treatment regimen was suggested by Centers for Disease Control and Prevention.[9]
Despite multi-drug therapy, the patient continued to deteriorate. The level of consciousness progressively declined, erythrocytes in CSF progressively increased and amoebae persisted in CSF on repeat examination after the end of intrathecal Amphotericin B therapy. The patient could not be salvaged. The possible reason can be due to late diagnosis, in part because the patient presented late in the hospital. Most of the reported survivors received early multi-drug therapy.
Several cases of PAM are misdiagnosed as bacterial or tubercular meningitis due to lack of awareness.[2] Increasing public awareness of the disease and maintaining high index of suspicion by healthcare professionals may help early diagnosis and timely initiation of multi-drug therapy. Preventive measures like avoidance of swimming in lakes epidemiologically associated with this disease, blowing out the nose after swimming to remove amoebae that may have been forcefully inhaled and use of nose plugs when jumping or diving into warm fresh water may reduce the risk of this devastating disease.[10]
References
- December 2002:19-year old male with febrile illness after jet ski accident. Brain Pathol. 2003;13:237-9.
- [Google Scholar]
- Successful treatment of Naegleria fowleri meningoencephalitis by using intravenous amphotericin B, fluconazole and rifampin. Arch Med Res. 2005;36:83-6.
- [Google Scholar]
- Primary amoebic meningoencephalitis caused by Naegleria Fowleri. PUJ. 2012;5:93-104.
- [Google Scholar]
- Characterization of brain inflammation during primary amoebic meningoencephalitis. Parasitol Int. 2008;57:307-13.
- [Google Scholar]
- Naegleria, acanthamoeba, and balamuthia. In: Feigin RD, Demmler GJ, Cherry JD, Kaplan SL, eds. Textbook of Pediatric Infectious Diseases (5th ed). Pennsylvania: Saunders; 2004. p. :2748-55.
- [Google Scholar]
- Successful treatment of primary amebic meningoencephalitis. N Engl J Med. 1982;306:346-8.
- [Google Scholar]
- Synergistic activities of azithromycin and amphotericin B against Naegleria fowleri in vitro and in a mouse model of primary amebic meningoencephalitis. Antimicrob Agents Chemother. 2007;51:23-7.
- [Google Scholar]
- Successful treatment of disseminated Acanthamoeba sp. infection with miltefosine. Emerg Infect Dis. 2008;14:1743-6.
- [Google Scholar]
- Available from: http://www.cdc.gov/parasites/naegleria/ treatment-hcp.html





