Translate this page into:
Postepidural Spinal Intradural Arachnoid Cyst: A Rare Case Report
Address for correspondence: Dr. Muhammad Sohail Umerani, Department of Clinical Neurosciences, King Fahd Military Medical Complex, Dhahran, KSA. E-mail: drumerani@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Compression of the neural structures in spine by an intradural arachnoid cyst is a rare entity. At times such a cyst is an incidental finding. Spinal epidural injection is one of the few rare etiological factors for its development. Symptomatic cysts can present with variable neurological manifestations depending on the spinal level involved. This includes back pain, lower limb weakness, and sphincteric dysfunction. If asymptomatic, they can be followed radiologically. Surgical decompression along with a histological diagnosis is reserved for cysts that are enlarging, symptomatic or the ones for whom the diagnosis is uncertain. Incomplete excision of cyst wall or simple fenestration and decompression mandates close follow-up, clinically and radiologically for further recurrences.
Keywords
Arachnoid cyst
epidural injection
spinal intradural
INTRODUCTION
Arachnoid cyst can be extradural or intradural, former being more common. Intradural cysts is a rare cause of cord compression.[12] Although it may be rarely present in lumbar or sacral spine, the most common location is in the middle and lower thoracic spine.[3] They may have a congenital origin. Those intradural cysts that are acquired have either a traumatic or inflammatory etiology since its origin from altered arachnoid trabeculae is attributed to these factors. They may be a sequel of a previous spinal procedure such as spinal myelography, hematoma from epidural injection, or repeated lumbar puncture causing meningitis or arachnoiditis with adhesions.[456] Intradural arachnoid cyst may have a silent course. They are often picked up incidentally on magnetic resonance imaging (MRI) where it appears as a cyst with signal intensity of cerebrospinal fluid (CSF). Symptomatic intradural cysts have variable presentation such as simple back pain, gait abnormality, weakness of the limbs, and bladder or bowel dysfunction. An acute presentation such as cauda equina syndrome is also been reported after lumbar spinal surgery.
CASE REPORT
Spinal epidural injection has been proposed a rare predisposing factor to the development of a symptomatic thoracolumbar intradural arachnoid cyst. We present here a case of a 43-year-old female patient who had been on treatment for the Grave's disease. She had initially presented to a physician with complaints of low back pain along with bilateral weakness of the legs for last more than a year with gradual progression. This was more noticeable to her whenever she was trying to stand up from a squatting position. Since she was not getting better on usual analgesics, so was then referred to a neurologist with a suggestion of proximal myopathy of the lower limbs secondary to Grave's disease. Detailed history revealed that she had been incontinent for urine for more than a year without letting this known to her physician out of embarrassment. This symptom had worsened in the last 3 months to the extent that now she was incontinent for bladder and bowel as well. The neurologist did a thorough neurological examination and requested for MRI dorsal and lumbar spine as an initial radiological examination to rule out any mass lesion compressing the cord. MRI had shown a thoracolumbar intradural extramedullary space occupying lesion of CSF signal intensity, measuring 67 mm × 17 mm × 24 mm in craniocaudal, anteroposterior, and transverse dimensions that was noncontrast enhancing and extending from D10 to L1 [Figure 1]. This was causing pressure and displacing the adjacent neurological structures toward the left side along with mild posterior scalloping of mainly D12 vertebral body. With this, the neurologist consulted us and on reviewing the MRI finding, it seemed that this was a septated cyst with a smaller upper and a larger lower part that had pushed the cord cranially and to its left. This dual picture of the cyst was unusual.
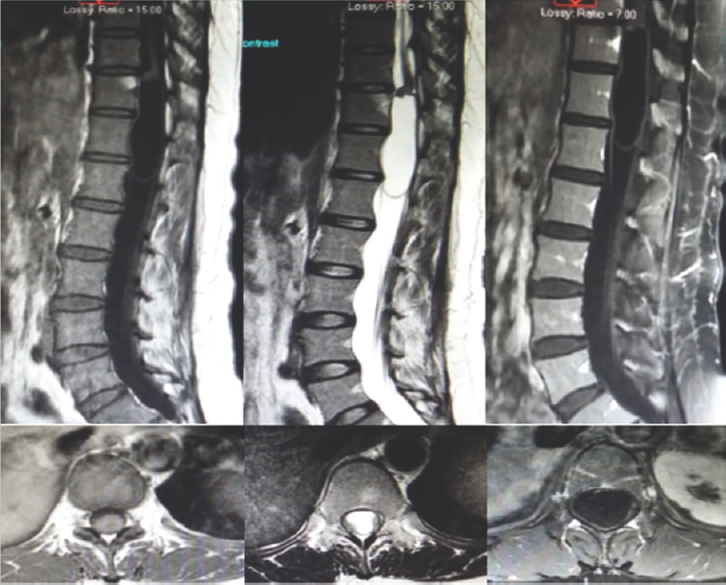
- Preoperative T1-weighted image, T2 weighted image and Gadolinium (GAD) contrast sagittal and axial magnetic resonance imaging images of intradural extramedullary cerebrospinal fluid signal intensity mass lesion opposite D11, D12, and upper border of L1 vertebrae
On inquiring again, the patient informed us that about 2½ years back, she had undergone a failed trial of spinal anesthesia during vaginal delivery after which she received general anesthesia. Her postpartum status was uneventful. About a year after delivery, she started having the symptoms for which she first visited her physician. Thereafter, we counseled her regarding our plan of surgical decompression. Peroperatively, after the opening of the dura, the cord seemed bulging with cyst being densely adhered to it. As soon as the arachnoid was opened through the cranial end of the cyst, its upper part got decompressed with egress of CSF. The caudal part of the cyst was then addressed, and fenestration was done through it. Part of cyst wall was sent for histopathological diagnosis. Postoperatively, the patient was mobilizing after 24 h and on the 3rd day of surgery, she was discharged home. The histopathology report showed that the cyst wall was made up of fibrous tissue rather than any meningothelial cells, suggestive of a pseudo arachnoid cyst. On follow-up in clinic, her weakness in the proximal muscle group of the lower limbs had markedly improved. Her bladder and bowel incontinence was also getting better. The wound was healing well, and the stitches were removed on 10th postoperative day. Follow-up MRI done after 2 weeks and later at 5 months had shown a significant reduction in the size of the cyst with normalization of the subarachnoid space [Figures 2 and 3].
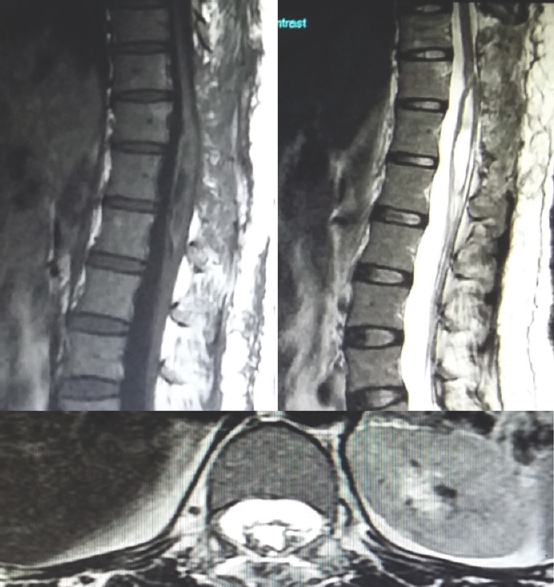
- Two-week postoperative T1-weighted image, T2 weighted image sagittal and axial magnetic resonance imaging images showing significant reduction in size of lesion

- Five-month postoperative T1-weighted image sagittal and axial magnetic resonance imaging images
DISCUSSION
The detailed history of our patient revealed the possibility of the cyst to be secondary to spinal anesthesia. The acquired intradural arachnoid cyst may result from iatrogenic spinal cord injury; either traumatic or after surgical procedure. This leads to arachnoiditis and subarachnoid adhesions.[7] The different surgical procedures or their complications so far reported in the literature are spinal laminectomy and discectomy, vertebroplasty, lumbar puncture, meningitis, postoperative epidural hematoma, and epidural injection for spinal anesthesia.[56]
In our patient, the symptoms started about a year after the event of failed trial of spinal anesthesia. Samuel in 2008 published the first ever case report of intradural arachnoid cyst after spinal anesthesia.[8] It usually presents itself in between fourth a sixth decade of life with a slight female predominance.[9] Our patient also presented in her early 40s. Her intradural arachnoid cyst was from D10 to L1 spinal level. Up to 80% of cysts are located in the middle and lower thoracic spine lying dorsal to the cord. Such a location in spine causes compression of the cord and nerve roots. Although may remain quiescent and only be evident on the radiological examination for some other symptomatology, ones progressively increasing in size can lead to a variable presentation. Rarely, they may rupture spontaneously and present with intracystic hemorrhage or with intracranial hypotension.[9] On average, these cysts have an extension of 3.7 vertebral bodies.[10] Giant arachnoid cyst with an extension from high dorsal to low lumbar has been described in literature.[11] In 2014, Gupta et al. reported an excision of a cyst, extending from D4 to L3 spinal segment after performing open door laminoplasty for a 15-year-old boy.[12]
Complete excision of the cyst should be the aim of surgical intervention. Exceptions to this treatment option include giant cyst, cyst adhered to the important neural structures, ventrally located cyst. In such cases, the ideal approach would be fenestration with cyst decompression or partial resection.[39] Similarly, in our case, the excision of cyst was impossible because of adhesion to adjacent neural elements, so fenestration was performed. Another interesting thing seen in the imaging study of our patient was the presence of a band or septa separating the cyst into two well-defined masses. One should avoid simple aspiration of the cyst as a sole method for decompression since it carries a considerable chance of reaccumulation.[1113]
CONCLUSION
The possibility of an idiopathic arachnoid cyst to develop intradurally after an epidural injection for spinal anesthesia is remote. A detailed history in doubtful cases leads to a clue. Careful radiological distinction is of prime importance to rule out other differentials. Although complete excision of the cyst is the ideal strategy for the symptomatic intradural cyst, however in situations where it is adhered to cord or nerve roots, fenestration is an acceptable option. Postoperative follow-up radiologically through MRI is of utmost importance to ascertain any recurrences in such cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Symptomatic spinal arachnoid cysts: Report of two cases with review of the literature. Spine (Phila Pa 1976). 2003;28:E25-9.
- [Google Scholar]
- Thoracic spinal intradural arachnoid cyst: Report of two cases and review of literature. Eur Radiol. 2002;12:877-82.
- [Google Scholar]
- Spinal cord compression caused by idiopathic intradural arachnoid cysts of the spine: Review of the literature and illustrated case. Eur Spine J. 2010;19(Suppl 2):S124-9.
- [Google Scholar]
- Rapid expansion of a ventral arachnoid cyst after syringo-subarachnoid shunting in the thoracic spinal cord: Case report. Surg Neurol. 2005;64:86-9.
- [Google Scholar]
- Thoracic intradural arachnoid cyst associated with surgical removal of epidural hematoma – Case report. Neurol Med Chir (Tokyo). 2004;44:607-10.
- [Google Scholar]
- Intradural arachnoid cyst associated with thoracic spinal compression fracture: 7-year follow up after surgery. Spinal Cord. 2001;39:599-601.
- [Google Scholar]
- Thoracic arachnoid cyst presenting as backache after spinal anaesthesia. Anaesthesia. 2008;63:1264-5.
- [Google Scholar]
- Spinal intradural juxtamedullary cysts in the adult: Surgical management and outcome. Neurosurgery. 2004;55:1352-9.
- [Google Scholar]
- Lateral intrathoracic meningocele associated with a spinal intradural arachnoid cyst. Pediatr Neurosurg. 2001;35:107-10.
- [Google Scholar]
- Long segment dorsolumbar spinal arachnoid cyst: A case report. Rom Neurosurg. 2014;XXI:82-4.
- [Google Scholar]
- Intradural extramedullary cysts of the spinal canal: Clinical presentation, radiographic diagnosis, and surgical management. Neurosurgery. 1992;30:35-42.
- [Google Scholar]






