Translate this page into:
Persistent Hypertensive Response Following Dexmedetomidine Infusion in a Patient with Cervical Spinal Cord Injury
Address for correspondence: Dr. Shalendra Singh, Department of Neuroanaesthesia, AIIMS, New Delhi, India. E-mail: drsinghafmc@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a 19-year-old male patient, an operated case of anterior cervical discectomy and fusion for traumatic C5–C6 vertebral injury, who developed persistent hypertension following dexmedetomidine infusion in the Intensive Care Unit to enable tolerance of noninvasive ventilation mask. This unusual side effect should be borne in mind when using this drug in patients with cervical spine injuries.
Keywords
Cervical spine injuries
dexmedetomidine
hypertension
INTRODUCTION
Dexmedetomidine is a centrally acting alpha-2-adrenergic agonist, which is widely used in neurosurgical procedures due to its beneficial effects on intracranial pressure (ICP) and cerebral blood flow. Sedation with dexmedetomidine resembles natural sleep as it results in a more physiologic sleep–wake cycle and patients remain arousable and cooperative. It is approved for sedation in mechanically ventilated patients for <24 h. The hemodynamic effects of dexmedetomidine show biphasic effect, which include both hypertension and hypotension.
CASE REPORT
A 19-year-old male patient presented with a history of trauma while jumping into a swimming pool. He presented to the emergency department with quadriplegia and impaired bowel and bladder sensation. Emergency computed tomography scanning revealed C5 burst fracture and C6 body sagittal split with cord compression without any brain injury. The patient had no other comorbidities. He was scheduled for C5 corpectomy with mesh cage placement and anterior cervical plating, which proceeded uneventfully under standard general anesthesia technique. He remained hemodynamically stable throughout the procedure and was subsequently shifted to the Intensive Care Unit (ICU) with endotracheal tube in situ.
On postoperative day 5, the patient was extubated, following a successful weaning trial. Since he was complained of some difficulty in breathing, the decision to transition the patient from oxygen via facemask to bilevel-positive airway pressure (FiO2 =40%, 8/4 cmH2O, 14 bpm) was made. The patient's Glasgow coma scale was 15, and his baseline vital signs were heart rate of 75, tachypnea with respiratory rate of 33 breaths/min, a blood pressure of 121/66 mmHg, and oxygen saturation by pulse oximetry of 92%. To reduce the patient's discomfort, he was administered dexmedetomidine at a dose of 0.5 mcg/kg/h, without a bolus dose directly through central venous access [Figure 1]. Blood pressure suddenly increased to 180/80 mmHg, and heart rate fell to 40 bpm. The patient was neither agitated nor in pain. Other etiologies of hypertension were ruled out (renal diseases and coarctation of aorta). Arterial blood gas analysis was done which failed to reveal hypercarbia or hypoxemia. This phenomenon resolved with the discontinuation of dexmwedetomidine infusion after 3 h of continuous infusion and treated with intravenous boluses of 20–30 microgram of nitroglycerine as required. The patient's blood pressure and heart rate gradually returned to initial parameters over approximately 20 min, and no further sedation was administered. No other similar episodes were noted during his hospitalization.
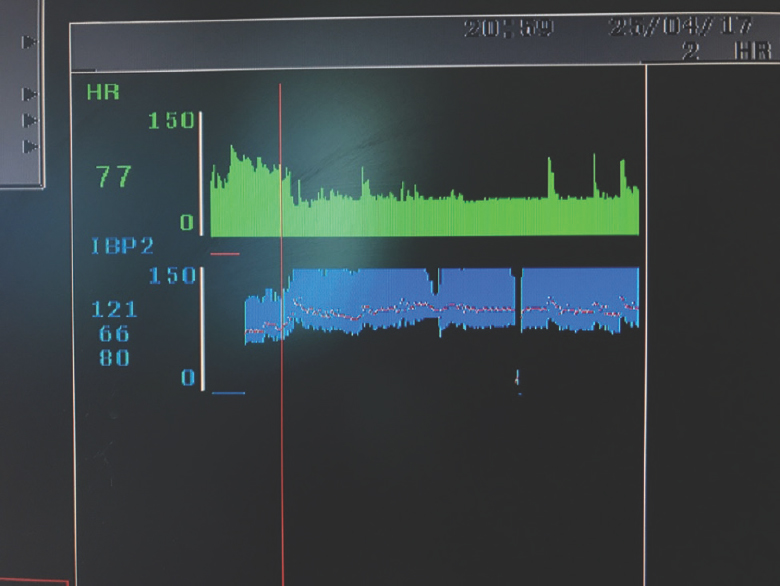
- Red line denotes initiation of dexmedetomidine infusion at 0.5 μg/kg/h
DISCUSSION
We present the occurrence of profound hypertension and bradycardia in a patient with cervical spine injury during dexmedetomidine infusion without any bolus dose. Dexmedetomidine is a nonopiate sedoanalgesic agent, and it is licensed for sedation of adults being mechanically ventilated for <24 h and for sedation of nonintubated patients before and/or during surgical and other procedures.[1] It is often used as part of a multimodal anesthetic regimen, since its sedative and anxiolytic properties are associated with minimal respiratory depression.[2] Since it has no action at opioid receptors, the typical side effects of narcotic use such as constipation and pruritus are not seen. Dexmedetomidine alpha-2 agonist effect produces sedation, analgesia, and anxiolysis within locus coeruleus in the pons. Stimulation of alpha-2 receptors in the dorsal horn of the spinal cord inhibits release of substance P for antinociceptive effects. Dexmedetomidine is more specific for alpha-2 action compared to alpha-1 with a ratio of 1620:1.[3] Its use has been described for awake fiberoptic intubationin patients with cervical spine injury, without causing any hemodynamic instability.[4]
The use of dexmedetomidine has been reported to cause refractory hypotension and bradycardia. The hypertension is thought to be due to an initial stimulation of peripheral alpha-1 or alpha-2b receptors due to higher peak plasma concentration following bolus dose, resulting in vasoconstriction. This decreases following subsequent central alpha-2a receptor activation, which exerts a stronger effect causing a biphasic response, including hypotension and bradycardia. In general, the recommendation is to administer dexmedetomidine boluses over 10 min to prevent profound hypotension and bradycardia that may be unresponsive to fluid therapy and vasopressor support. The hypertension associated with dexmedetomidine is usually mild, transient, and does not require treatment.
However, in our case, the hypertensive effect occurred with a low infusion dose of dexmedetomidine without any bolus administration. Patients with cervical cord injury may have autonomic dysfunction and difficulty in regulating blood pressure. Until now, there have been no published case reports of dexmedetomidine-induced hypertensive response in patients with cervical spine injury. Previous reports regarding the use of this drug have included an 18-year-old boy with acute traumatic brain injury with spikes in ICP, who was maintained on dexmedetomidine infusion for mechanical ventilation in the ICU.[5] Although we cannot definitely prove a causal relationship, other causes for hypertension were ruled out and the hypertension resolved following termination of the infusion. We present this case to caution practitioners about this uncommon side effect. Anesthesiologists should be aware of this hemodynamic response of dexmedetomidine in patients with cervical cord injury even at lower infusion dose.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Pharmacokinetics of dexmedetomidine infusions for sedation of postoperative patients requiring intensive caret. Br J Anaesth. 2002;88:669-75.
- [Google Scholar]
- Dexmedetomidine: Pediatric pharmacology, clinical uses and safety. Expert Opin Drug Saf. 2011;10:55-66.
- [Google Scholar]
- Characterization of the selectivity, specificity and potency of medetomidine as an alpha 2-adrenoceptor agonist. Eur J Pharmacol. 1988;150:9-14.
- [Google Scholar]
- Dexmedetomidine provides optimum conditions during awake fiberoptic intubation in simulated cervical spine injury patients. J Anaesthesiol Clin Pharmacol. 2016;32:54-8.
- [Google Scholar]
- High-dose dexmedetomidine-induced hypertension in a child with traumatic brain injury. Neurocrit Care. 2008;9:366-9.
- [Google Scholar]






