Translate this page into:
Patterns of Illness Behaviors and its Correlates in Patients with Chronic Nonorganic Pain
Address for correspondence: Dr. Geetha Desai, Department of Psychiatry, NIMHANS, Bengaluru - 560 029, Karnataka, India. E-mail: desaigeetha@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Illness behaviors if abnormal can have significant influence in presentations of chronic pain. The aim of the study was to derive the patterns of illness behaviors and its correlates in subjects with chronic nonorganic pain.
Methods:
Illness Behavior Questionnaire (IBQ) was administered to 301 adult individuals with chronic nonorganic pain. Factor analysis was performed on the IBQ, and relationships of the dimensions of illness behavior with clinical and demographic variables were computed.
Results:
Majority of the sample consisted of women (n = 208; 69%) with 43% from rural background and 58% from below poverty line status. Principal axis factoring resulted in four factors, namely health concerns, affective inhibition (AI), bodily distress, and affective distress with psychosocial problems. The three factors excluding AI had significant intercorrelation among them. There was significant difference in mean scores of factors, bodily distress and affective distress in patients from urban and rural background.
Conclusions:
Illness behaviors in chronic nonorganic pain can be understood as three interrelated factors-health concerns, affective distress with psychosocial problems, and bodily distress. AI might be an independent factor for presentation of chronic nonorganic pain.
Keywords
Affective inhibition
bodily distress
chronic pain
health concerns
Illness Behaviour Questionnaire
illness behavior
INTRODUCTION
Clinicians treating chronic nonorganic pain often are dealing with illness behaviors which impact their manifestations and management. Research on chronic nonorganic pain has predominantly focused on the nature and severity of symptoms and its evidence on functioning and health care utilization.[12] Illness behaviors in chronic pain have been researched in the early 1970s and 1980s. However, the last quarter of century has seen sparse research on this potentially clinically significant topic.
Illness behavior was described as “the varying perceptions, thoughts, feelings, and acts, affecting the personal and social meaning of symptoms, illness, disabilities, and their consequences.”[3] Pilowsky further described the concept of abnormal illness behavior (AIB).[4] In conditions where in patient's illness behavior is disproportionate to the clinician's assessment of objective pathology and patient persists in the sick role, then this is a form of AIB. Illness behaviors are reported to be influenced by patient-related, illness-related and doctor-related variables.[5] AIB has been studied in chronic pain, myocardial infarction, rheumatoid arthritis, stroke, systemic sclerosis, Meniere's disease, cancer, HIV, depression, and somatization.[67891011121314151617181920212223] Most of the research on AIB has focused on disorders characterized by functional somatic complaints and chronic pain. A selective systematic review of illness behavior studies conducted in India has reported significant variations in the presentations of AIB.[24]
Measurement of illness behavior has also been a challenge.[25] Illness behavior questionnaire (IBQ)[6] has been the most commonly used instrument to assess AIB across studies. However, previous studies over the last four decades have shown that the factor structure and numbers of factors have varied from 3 to 11.[6121626] On the one hand, this raises questions about the persistence of factors across studies, and on the other hand, it depicts the underlying variance in the presentation of AIB in chronic nonorganic pain. Hence, the current research aims to study the patterns of AIB in patients presenting with chronic nonorganic pain. Given the variability in the factor structures noted for IBQ, this study attempts to revisit and resurrect fresh factor configuration.
METHODS
The study sample was from the participants attending outpatient services of the Department of Psychiatry, National Institute of Mental Health and Neurosciences, Bengaluru, India. Consecutive patients who satisfied the inclusion criteria were recruited for the study. Participants of either gender between the age of 18–45 years, reporting persistent pain (pain should have been present at least daily or on alternate days) for >6 months for which no organic basis was found were included in this study. Those with a history of psychosis, mental subnormality, organic brain syndrome or medical disorders, currently or in the previous 1 year, were excluded from the study.
Sociodemographic and clinical details were noted systematically by a semistructured pro forma. Clinical diagnosis was ascribed as per International Classification of Diseases 10th Revision (ICD-10). Illness behavior was assessed using the IBQ (62 items).[6] It assesses the patient's attitudes and affects about his or her illness and the patient's perception of the attitudes of significant others towards himself or herself and their illness. IBQ has been utilized in Indian setting with varied factor presentation. The IBQ has been previously translated to Hindi and adapted.[2127]
Factor analysis was performed to derive the different factors of IBQ, using Principal axis factoring (PAF) method. PAF extraction method was used as it is often considered as a better method than principal component analysis (PCA). In PAF, the analysis of data structure is based on shared variance and not on sources of error that are unique to individual measurements. The IBQ responses are coded as yes or no. Since this was binary data, tetrachoric correlation matrix was formulated. The final factors were retained after orthogonal rotation (vide infra).
The study was approved by the Institutional Ethics committee, and written informed consent was sought from participants.
RESULTS
The total number of participants for this study was 301. The mean age in years for the sample was 34.8 ± 7.76. The mean age in years for women was 35.5 ± 7.58 and for men 33.4 ± 8.04. Majority of the sample were women (n = 208; 69%), married (n = 224; 75%), and belonged to Hindu (n = 225; 75%) religion. Nearly 43% (130) of the samples were from the rural background and 58% (175) were below the poverty line. The mean years of education were 7.9 ± 4.74.
The mean duration of pain symptoms in years was 5.78 ± 5.43. About 61% of the sample did not have any precipitating factor before the onset of symptoms. The predominant site of pain was head followed by pain in extremities. Most of them (97%) had moderate-to-severe intensity of symptoms. The most common ascribed ICD-10 diagnosis was somatoform disorders (142; 47%), followed by chronic pain syndrome (105; 35%), and depressive and anxiety disorders (51; 18%).
Principal axis factoring
Eighteen factors were obtained by applying Kaiser criterion of eigen value more than 1.0. Using explained variance of minimum of 5% and loading value of 0.4 resulted in four factors. Nine items with high unique variance did not load on any of the four factors. These IBQ items were – Are you easy to get on with, when are you ill?, Does your family have a history of illness?, Do you think other people realize what it is like to be sick?, Does it upset you to talk to the doctor about your illness?, Do you know anybody who has had the same illness as you?, Do you find that your illness affects your sexual relations?, When you are angry, do you tend to bottle up your feelings?, Do you find that you get sad easily? And Are you always a co-operative patient?
PAF was repeated after removing these items. There was no significant difference in the factors that were obtained without the items. The four factors that were retained after orthogonal rotation are given below. The total explained variance from the above four factors was 44.45.
The first factor had 14 items and the items reflected health concerns and anxieties. This factor has been termed as health concerns and the mean, and standard deviation (SD) for this sample was 6.55 ± 3.72. The second factor had six items and reflects affective inhibition (AI) and the mean and SD was 2.64 ± 1.80. The third factor had 17 items and these were related to bodily distress and the mean and SD were 11.34 ± 3.15. The last factor was a mix of affective disturbance and psychosocial problems and had 16 items, and the mean and SD were 5.11 ± 3.33.
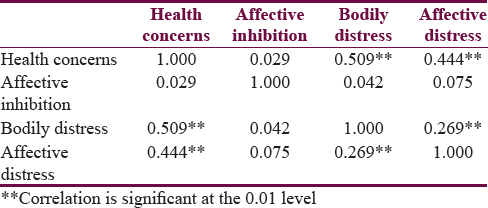
There was a significant correlation among the factors health concerns, bodily distress, and affective distress with psychosocial problems. AI did not correlate with the above factors [Table 1].
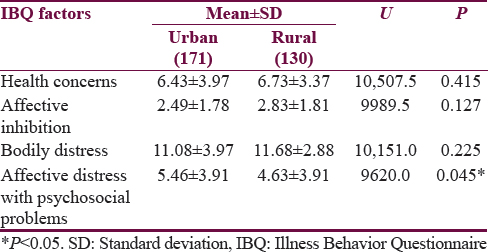
When gender differences were examined across the four subscales men had higher mean scores of AI (2.45 ± 1.78; 3.06 ± 1.79; U = 7692.0, P = 0.004) and women had higher scores on bodily distress (5.41 ± 4.17; 4.97 ± 3.82; U = 7783.0, P = 0.008). Participants from below the poverty line category had higher bodily distress (10.76 ± 3.41; 11.76 ± 2.87; U = 9202.5, P = 0.017) and lower affective distress with psychosocial problems (5.92 ± 4.51; 4.51 ± 3.51; U = 9072.0, P = 0.008). The mean scores of IBQ factors and background are provided in Table 2.
The mean scores of factors did not differ across the diagnostic groups, except for affective distress scores which were significantly higher in depressive and anxiety disorders (6.65 ± 3.82) as compared to somatoform disorders (4.59 ± 3.96) and chronic pain (5.09 ± 3.79) (H=11.457; P = 0.003).
DISCUSSION
In this study, the four dimensions of illness behaviors in persons with chronic nonorganic pain have been identified. These four factors are within the number of factors derived in previous studies which ranged from 3 to 11.[6121626]
The four factors derived were health concerns, AI, bodily distress, and affective distress with psychosocial problems. This is in contrast to the seven,[6] three,[26] and four[27] factors in previous studies. The comparison of factors across various studies is provided in Table 3.
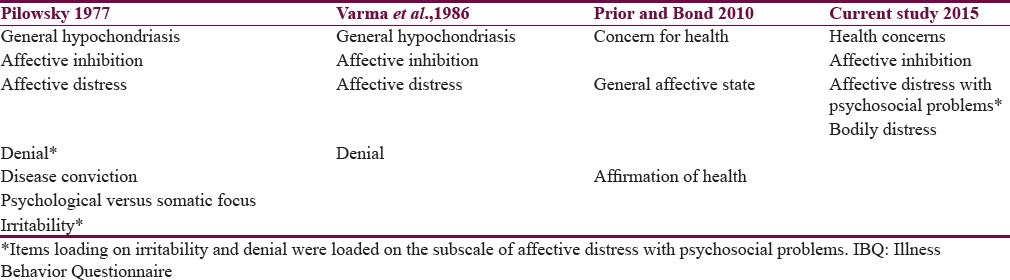
Interestingly, only AI was the common factor which was observed in previous studies using IBQ. One may wonder if alexithymia manifests in the form of AI. This finding has been consistently noted across most studies.[122627] Denial as an independent factor did not emerge in the current study; the IBQ items of denial loaded within the factor on affective distress and psychosocial problems. The possibility could be that the bodily symptoms could lead to dysfunction and then on to affective distress. Bodily distress emerged as an independent factor of illness behavior which has not been established in any of the earlier studies. The preoccupation with bodily distress might lead to health anxiety and affective distress.
The factor health concerns were compared with Whiteley's index[6] which assess hypochondriasis, eight items were found common between health concerns as well as Whiteley's index. The scores of health concerns correlated positively with Whiteley's index scores. It also correlated with bodily distress and affective distress with psychosocial problems. When the median value of health concerns was examined, nearly 60% of the sample scored above the median of six indicating that they had high health concerns.
Affective distress with psychosocial problems included questions on anxiety, depression, anger, irritability and also includes questions on various problems in life. Bodily distress, health concerns, and affective distress with psychosocial problems highly correlated with each other indicating that these factors describe the underlying psychopathology in patients with chronic nonorganic pain. Interestingly, the term bodily distress disorders have been proposed for somatoform disorders in the revised version of the ICD-10.[25]
AI was similar to factors described in the studies.[122627] The fact that this factor did not correlate with other factors raises the question of it being an independent dimension which needs examination regarding state or trait. AI as a pattern of AIB is probably an unique phenomena, which, could lead to bodily distress and thereby health concerns. AI despite being recognized as a concept long ago but has not been well researched.[28] The relationship between AI and alexithymia also needs to be reviewed, regarding their role in the presentation of chronic nonorganic pain.
The concept of AIB described Pilowsky[4] had three elements to describe AIB. The first component being the persistence of a maladaptive mode of experiencing, perceiving, evaluating, and responding to one's own health status. This aspect of the of AIB is best described the two factors in this study – bodily distress and health concerns. Participants who experience bodily distress would perceive as being ill, and the cause for their symptoms is not evident and would be seeking treatment for the relief of pain symptoms. However, the persistence of pain could lead to health concerns which make the persons more focused on their bodily sensations and anxious. The second and third part of the description of AIB are, adequate assessment of all relevant biological, psychological, social, and cultural factors and despite, the fact that a doctor has provided a lucid and accurate appraisal of the situation and management to be followed (if any), with opportunities for discussion, negotiation, and clarification. Adequate assessment of all relevant factors is highly variable and depends on the health professionals knowledge and attitude. Illness behaviors are influenced by doctor–patient relationship and are not evident in the factors that have been derived from this study. There could be many explanations for the same. The doctor–patient relationship is at a different level in the current setting, with not getting enough time with doctors for discussion, or doctors dismissing them as “nothing seriously wrong, no problem, could be stress related.” Each health professional may not provide the same kind of care and explanations which again can lead to AIBs.
The current study conceptualizes illness behaviors as a phenomenon, which has three major domains in patients presenting with chronic nonorganic pain. Bodily distress which is characterized by experiences of physical symptoms, preoccupation with these symptoms, constant monitoring of symptoms, thought of being vulnerable of being ill could lead to significant concerns about their health. This is manifested often by worries related to health, disease. The bodily distress and health concerns could lead to affective distress with psychosocial problems. However, the reverse could also be true where in participants who have affective distress with psychosocial problems could focus more on their bodily sensation and worry about their health.[29]
It should be acknowledged that illness behaviors tend to be on a continuum, fluctuate over period, and have varying distress levels associated with symptoms. Illness behavior is a dynamic concept; hence, a prospective design would have been a better method to study than a cross-sectional assessment as in the present study. Measuring illness behaviors cross-sectionally is further a limitation as the perception of their health state and illness might be a selective focusing on their current symptoms and distress. Many methods of exploratory factor analysis have been used, the most common one being PCA. However, there are criticisms that PCA is a mere data reduction procedure. Other statistical methods such as full information factor analysis based on item response theory could have been considered. However, PFA was considered for the current sample size.
CONCLUSIONS
Illness behavior in chronic nonorganic pain has three interrelated domains-health concerns, affective distress with psychosocial problems and bodily distress. AI might be an independent domain. Assessing severity and dysfunction are essential in patients with chronic pain as this can lead to illness behaviors. It could be bidirectional as symptoms and dysfunction per se could be due to AIBs. The assessment of illness behavior across these domains will help us to develop a management for that individual. Early identification of AIB could prevent significant burden on the health resources as well as address it in treatment. Behaviors arising out of an illness can be managed by treating the illness, but when behaviors itself is the illness; it costs heavily for the health systems and derails the functioning of the health systems.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Total somatic symptom score as a predictor of health outcome in somatic symptom disorders. Br J Psychiatry. 2013;203:373-80.
- [Google Scholar]
- Revisiting the symptom iceberg in today's primary care: Results from a UK population survey. BMC Fam Pract. 2011;12:16.
- [Google Scholar]
- The study of illness behaviour: Some implications for medical practice. Med Care. 1965;3:30-2.
- [Google Scholar]
- Patterns of illness behaviour in patients with intractable pain. J Psychosom Res. 1975;19:279-87.
- [Google Scholar]
- Pain, depression, and illness behavior in a pain clinic population. Pain. 1977;4:183-92.
- [Google Scholar]
- Responses to illness and health in chronic pain patients and healthy adults. Psychosom Med. 1987;49:470-81.
- [Google Scholar]
- Site of pain: Relationship to measures of pain description, behavior and personality. Pain. 1984;19:389-97.
- [Google Scholar]
- Illness behavior as a predictor of pain and overt behavior patterns in chronic low back pain patients. J Psychosom Res. 1986;30:543-51.
- [Google Scholar]
- Psychometric construction and validity of the pilowsky illness behaviour questionnaire in British patients with chronic low back pain. Pain. 1987;28:13-25.
- [Google Scholar]
- Dimensions of illness behaviour as measured by the illness behaviour questionnaire: A replication study. J Psychosom Res. 1993;37:53-62.
- [Google Scholar]
- Psychiatric disorder and illness behaviour in rheumatoid arthritis. Br J Rheumatol. 1988;27:357-63.
- [Google Scholar]
- Illness behaviour and outcome following survived myocardial infarction: A prospective study. J Psychosom Res. 1981;25:97-107.
- [Google Scholar]
- Measuring illness behavior in patients with systemic sclerosis. Arthritis Care Res (Hoboken). 2013;65:585-93.
- [Google Scholar]
- Abnormal illness behaviour in rehabilitation from stroke. Clin Rehabil. 1997;11:162-70.
- [Google Scholar]
- Illness behaviour, personality traits, anxiety, and depression in patients with Menière's disease. J Otolaryngol. 1996;25:329-33.
- [Google Scholar]
- Psychiatric and psychosocial concomitants of abnormal illness behaviour in patients with cancer. Psychother Psychosom. 1996;65:246-52.
- [Google Scholar]
- Illness behavior, emotional stress and psychosocial factors among asymptomatic HIV-infected patients. Psychother Psychosom. 1999;68:31-8.
- [Google Scholar]
- Dhat syndrome: Is it a distinct clinical entity? A study of illness behaviour characteristics. Acta Psychiatr Scand. 1995;91:136-9.
- [Google Scholar]
- An investigation of hysteria using the illness behaviour questionnaire. Br J Psychiatry. 1985;146:601-8.
- [Google Scholar]
- Illness behaviour: normal to abnormal – A selective systematic review of research from India. 2016. Int J Med. 5:2. Available from: http://www.intjmi.com/browse.php?a_code=A-10-1-138&slc_lang=en&sid=1
- [Google Scholar]
- World Health Organization. The ICD.10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992.
- New dimensions of abnormal illness behaviour derived from the illness behaviour questionnaire. Psychol Health. 2010;25:1209-27.
- [Google Scholar]
- Illness behaviour questionnaire (IBQ): Translation and adaptation in India. Indian J Psychiatry. 1986;28:41-6.
- [Google Scholar]
- The phenomenon of ‘alexithymia’. Observations in neurotic and psychosomatic patients. Psychother Psychosom. 1977;28:47-57.
- [Google Scholar]
- Do diagnostic criteria for psychosomatic research explain diagnosis of medically unexplained somatic symptoms. Psychother Psychosom. 2016;85:121-2.
- [Google Scholar]






