Translate this page into:
Nonfatal Stroke and All-Cause Mortality among Community-Dwelling Older Adults Living in Rural Ecuador: A Population-Based, Prospective Study
Address for correspondence: Dr. Oscar H. Del Brutto, Air Center 3542, P. O. Box: 522970, Miami, FL 33152-2970, USA. E-mail: oscardelbrutto@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Stroke is a leading cause of disability in developing countries. However, there are no studies assessing the impact of nonfatal strokes on mortality in rural areas of Latin America. Using a population-based, prospective cohort study, we aimed to assess the influence of nonfatal strokes on all-cause mortality in older adults living in an underserved rural setting.
Methods:
Deaths occurring during a 5-year period in Atahualpa residents aged ≥60 years were identified from overlapping sources. Tests for equality of survivor functions were used to estimate differences between observed and expected deaths for each covariate investigated. Cox proportional hazards models were used to estimate Kaplan–Meier survival curves of variables reaching significance in univariate analyses.
Results:
Of 437 individuals enrolled over 5 years, follow-up was achieved in 417 (95%), contributing 1776 years of follow-up (average 4.3 ± 1.3 years). Fifty-one deaths were detected, for an overall cumulative 5-year mortality rate of 12.2% (8.9%–15.6%). Being older than 70 years of age, having poor physical activity, edentulism, and history of a nonfatal stroke were related to mortality in univariate analyses. A fully adjusted Cox proportional hazards model showed that having history of a nonfatal stroke (P = 0.024) and being older than 70 years of age (P = 0.031) independently predicted mortality. In contrast, obesity was inversely correlated with mortality (P = 0.047).
Conclusions:
A nonfatal stroke and increasing age increase the risk of all-cause mortality in inhabitants of a remote rural village. The body mass index is inversely related to death (obesity paradox).
Keywords
All-cause mortality
cardiovascular risk factors
community-based study
nonfatal strokes
prospective cohort study
INTRODUCTION
Stroke burden is on the rise in Latin American countries and represents a leading cause of disability in the region.[1] In previous studies, we demonstrated that prevalence and incidence of stroke in rural Ecuador are similar to that seen in industrialized nations.[23] However, there are no studies assessing the impact of previous nonfatal strokes on all-cause mortality in these rural areas, where living conditions and health-care access are different than in urban centers. Using the Atahualpa project cohort, we aimed to assess the influence of nonfatal stroke on all-cause mortality in community-dwelling older adults living in a remote rural setting.
METHODS
Characteristics of Atahualpa residents have been detailed elsewhere.[4] In brief, >95% of the population belongs to the Ecuadorian native/Mestizo ethnic groups, and their living characteristics, dietary habits, and socioeconomic status are homogeneous. Individuals aged ≥60 years who signed the informed consent were prospectively followed up by means of yearly door-to-door surveys (2012–2017) and other overlapping sources. The protocol was approved by the Institutional Review Board of Hospital-Clínica Kennedy, Guayaquil, Ecuador (FWA 00006867).
To identify stroke survivors, all participants were screened by rural doctors with the use of a validated field questionnaire, and then, certified neurologists confirmed the diagnosis. An overt stroke was defined as a rapidly developing event lasting >24 h with no apparent cause other than vascular. These individuals were invited to undergo examinations (blood tests, brain magnetic resonance imaging [MRI], magnetic resonance angiography of intracranial vessels, electrocardiography, transthoracic echocardiogram, and Doppler examination of extracranial arteries) to categorize the specific stroke subtype.
Demographics, cardiovascular risk factors (smoking status, body mass index [BMI], physical activity, diet, blood pressure, fasting glucose blood levels, and total cholesterol blood levels), severe edentulism, and history of nonfatal myocardial infarction were selected as confounding variables. These confounders were assessed at the time of enrollment by means of previously described interviews and procedures.[345] In particular, edentulism was included as a covariate as it has been related to mortality[6] as well as to stroke incidence in the Atahualpa population.[3]
Data analyses are carried out using STATA version 14 (College Station, TX, USA). In univariate analyses, continuous variables were compared by linear models and categorical variables by Chi-square or Fisher's exact test as appropriate. Mortality incidence rate ratios (IRR) were estimated for all the assessed covariates. For computing person-years of follow-up, we considered the time under surveillance starting the day of the first visit and ending at the administrative censoring date (June 1) of the last annual survey when the individual was interviewed or the date of death. Univariate tests for equality of survivor functions (log-rank) were used to estimate differences between numbers of observed and expected deaths for each covariate investigated. Cox proportional hazards models, adjusted for covariates reaching significance in univariate analyses, were used to estimate Kaplan–Meier survival curves of variables reaching significance in univariate analyses.
RESULTS
From a total of 437 individuals aged ≥60 years enrolled in the Atahualpa project from June 2012 to May 2017, follow-up has been possible in 417 (95%), contributing 1776 years of follow-up (average 4.3 ± 1.3 years). The median age of this followed population was 70 years, 235 (56%) were women, 337 (81%) had primary school education only, 195 (47%) individuals had severe edentulism, and 21 (5%) had a nonfatal myocardial infarction. A BMI ≥30 kg/m2 was noticed in 89 (21%) persons, blood pressure ≥140/90 mmHg in 190 (46%), fasting glucose ≥126 mg/dL in 141 (34%), and total cholesterol levels ≥240 mg/dL in 47 (11%). Eight (2%) participants were current smokers, 21 (5%) had a poor diet, and 49 (12%) had poor physical activity.
Forty-five (11%) participants had history of a nonfatal stroke (strokes not leading to death during the first 30 days). Of these, 32 patients had an ischemic and six had a hemorrhagic stroke; in the remaining seven cases, no imaging examinations were performed. Of the 32 patients with an ischemic stroke, 12 had cerebral small vessel disease as the most likely pathogenetic mechanism underlying the stroke and 10 had large vessel disease (intracranial); in the remaining 10 cases, no mechanism could be identified despite the practice of complementary examinations already mentioned in the method section. No patient had atrial fibrillation or another major cardiac source of intracranial emboli. Of the six patients with an intracranial hemorrhage (detected by echo gradient sequences on MRI), five had bleeding in the putamen, head of the caudate nucleus, or the pontine tegmentum (suggesting hypertensive arteriolopathy as the most likely pathogenetic mechanism), and the remaining patient had a lobar hemorrhage (cause not identified).
A total of 51 deaths were recorded during the study period. The overall cumulative 5-year mortality rate was 12.2% (95% confidence interval (C.I.): 8.9–15.6). The cause of death could be identified as nonvascular in 31 cases, as probable vascular in 11, and as vascular in the remaining nine (of these, three had a fatal stroke and six had a fatal acute myocardial infarction). However, this might be subject to misclassification because no autopsies were performed and proper diagnostic tests were done in just a few cases (most individuals died at home).
Fourteen (31.1%) of the 45 patients with history of a nonfatal stroke died during the follow-up period, as opposed to 37 of the 372 participants without a previous stroke (31.1% vs. 9.9%, P < 0.0001). Of the 14 patients with history of a nonfatal stroke who died during the study period, nine had a cerebral infarction, two had an intracranial hemorrhage, and the remaining three had strokes of unknown cause as neuroimaging studies were not performed.
Univariate analyses showed different mortality IRR for each of the measured risk factors. Being older than 70 years of age, having history of a nonfatal stroke, poor physical activity, and severe edentulism were significantly related to mortality, whereas individuals with primary school education only, a poor diet, and fasting glucose levels ≥126 mg/dL had a nonsignificant trend for a higher mortality rate ratio [Table 1]. These results were – as expected – similar to those found by the use of univariate tests for equality of survivor functions (log-rank) [Table 2].
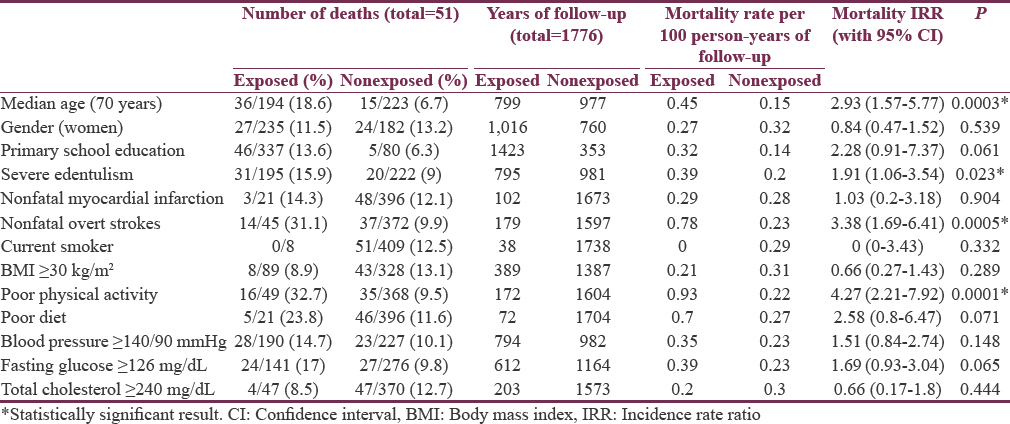

A fully adjusted Cox proportional hazards model showed that being older than 70 years of age (hazard ratio: 2.09, standard error [SE]: 0.72; 95% C.I.: 1.07–4.1; P = 0.031) and having history of a nonfatal stroke (hazard ratio: 2.18, SE: 0.75; 95% C.I.: 1.11–4.28; P = 0.024) independently predicted mortality [Figure 1]. In contrast, having a BMI ≥30 kg/m2 was inversely correlated with mortality (hazard ratio: 0.18, SE: 0.16; 95% C.I.: 0.03–0.98; P = 0.047). No other covariate independently predicted mortality in this multivariate model.
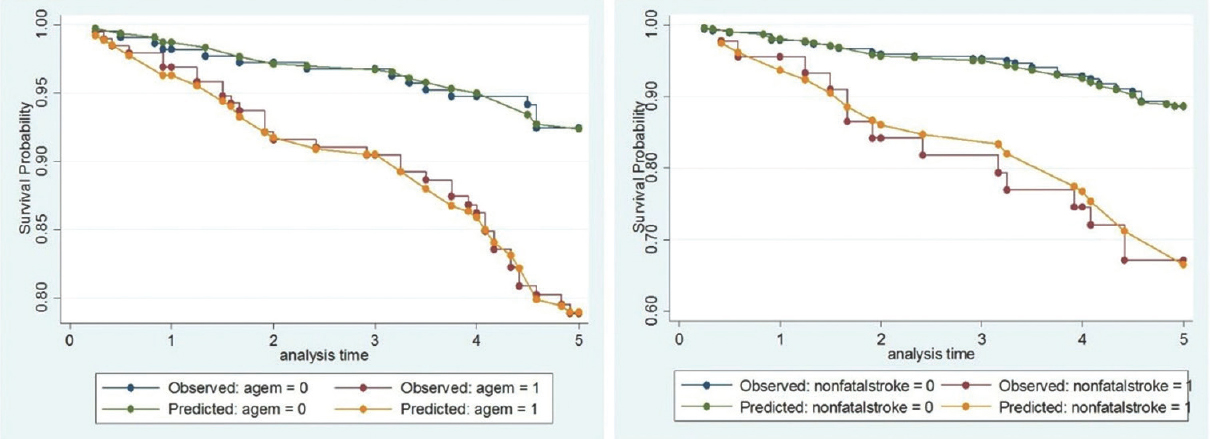
- Kaplan–Meier survival probability analyses of the two factors independently associated with an increased mortality rate in the fully-adjusted Cox proportional hazards model in this study, including, left: Being older than 70 years of age (P = 0.031) and right: Having history of a nonfatal stroke (P = 0.024)
DISCUSSION
In this population of community-dwelling older adults living in rural Ecuador, history of a nonfatal stroke and increasing age were independently related to increased mortality. Conceivably, the importance of these variables probably blurred the independent effect of individual cardiovascular risk factors when included in the multivariate Cox proportional hazards model (due to high levels of correlation). Indeed, having a poor physical activity was significantly associated with mortality in univariate analyses but lost its significance in the fully adjusted model. Likewise, the nonsignificant trend for a higher mortality rate showed in univariate analyses by fasting glucose levels ≥126 mg/dL and also disappeared in the multivariate model. Severe edentulism – a major stroke risk factor in the population of Atahualpa[3] – was also significantly associated with mortality in univariate analysis but not when other variables were included in the Cox proportional hazards model.
Interestingly, the BMI was inversely associated with mortality in the follow-up, supporting the concept of an obesity paradox, a term that encompasses several unexpected relationships between anthropometric indices and adverse cardiovascular outcomes, including vascular death.[789] In our series, however, the multivariate hazard ratio of a BMI ≥30 kg/m2 (0.18) was very close to its SE (0.16), suggesting that only certain subgroups of persons with obesity have a lower mortality rate. This paradox needs further investigation in the population of Atahualpa.
According to the literature, having less cardiovascular risk factors reduced the risk of death. In the Aerobics Center Longitudinal Study, the risk of death was 55% lower in participants with <3% and 63% lower in those with <2 cardiovascular risk factors.[10] In the Northern Manhattan Study, the risk of vascular death was 30% and 50% lower in people who had only one cardiovascular risk factor.[11] In the National Health and Nutrition Examination Study, having <2 cardiovascular risk factors reduced the risk of all-cause mortality (hazard ratio: 0.22 [95% C.I.: 0.1–0.5]).[12] None of these studies, however, considered the independent weight of individual risk factors on mortality rate; therefore, data might not be comparable with our results.
The Seoul Male Cohort Study (Korea) considered the impact of individual cardiovascular risk factors on the risk of death. In that study, nonsmoking status, normal blood pressure, and fasting glucose levels <100 mg/dL were independently associated with lower mortality risk.[13] However, the study was restricted to men aged 40–59 years and might not be extrapolated to our population. In the large Kailuan Study (China), nonsmoking status, ideal physical activity, and normal blood pressure and fasting glucose levels were independently associated with a lower mortality rate.[14]
Major strengths of our study include the population-based design with unbiased enrollment of participants, the standardized protocol used for data collection and mortality surveillance, and the excellent retention of the cohort since Atahualpa is a closed village with little migration rates. However, the study has limitations. We did not consider possible changes in cardiovascular risk factors over time, which might have influenced mortality rate in the follow-up. Since we have been settled in the village for the past 5 years, visiting people and performing complimentary examinations, it is possible that advising on how to improve lifestyle and dietary habits had an impact in some of the participants, thus changing their cardiovascular risk factors.[1516] In addition, due to lack of autopsies and the fact that most people died at home, information on the cause of death was incomplete for many cases. Therefore, we could not assess whether cardiovascular risk factors were specifically associated with vascular or nonvascular deaths or if there were some hidden confounders that influenced outcome. Another limitation is the fact that Atahualpa residents might not be representative of other Latin American rural settings. Further collaborative longitudinal studies are needed to confirm these findings.
Financial support and sponsorship
This study was financially supported by Universidad Espíritu Santo, Guayaquil, Ecuador.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Stroke epidemiology, prevention, and management strategies at a regional level: Latin America and the Caribbean. Lancet Neurol. 2007;6:362-72.
- [Google Scholar]
- Stroke in rural coastal Ecuador: A community-based survey. Int J Stroke. 2014;9:365-6.
- [Google Scholar]
- Severe edentulism is a major risk factor influencing stroke incidence in rural Ecuador (The Atahualpa Project) Int J Stroke. 2017;12:201-4.
- [Google Scholar]
- Door-to-door survey of cardiovascular health, stroke, and ischemic heart disease in rural coastal Ecuador – the Atahualpa Project: Methodology and operational definitions. Int J Stroke. 2014;9:367-71.
- [Google Scholar]
- Population-based study of cardiovascular health in Atahualpa, a rural village of coastal Ecuador. Int J Cardiol. 2013;168:1618-20.
- [Google Scholar]
- Association between missing tooth count and mortality: A systematic review. J Prosthodont Res. 2018;62:134-51.
- [Google Scholar]
- Impact of body mass index on outcome after percutaneous coronary intervention (the obesity paradox) Am J Cardiol. 2002;90:42-5.
- [Google Scholar]
- Body mass index and mortality in heart failure: A meta-analysis. Am Heart J. 2008;156:13-22.
- [Google Scholar]
- Inverse relationship between the body mass index and severity of carotid siphon calcifications (another obesity paradox): Results from the Atahualpa Project. Atherosclerosis. 2017;259:1-4.
- [Google Scholar]
- Ideal cardiovascular health and mortality: Aerobics Center Longitudinal Study. Mayo Clin Proc. 2012;87:944-52.
- [Google Scholar]
- Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: The Northern Manhattan study. Circulation. 2012;125:2975-84.
- [Google Scholar]
- Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987-95.
- [Google Scholar]
- Cardiovascular health metrics and all-cause and cardiovascular disease mortality among middle-aged men in Korea: The Seoul male cohort study. J Prev Med Public Health. 2013;46:319-28.
- [Google Scholar]
- The ideal cardiovascular health metrics associated inversely with mortality from all causes and from cardiovascular diseases among adults in a Northern Chinese industrial city. PLoS One. 2014;9:e89161.
- [Google Scholar]
- The “know your numbers” program in Atahualpa – A pilot study aimed to reduce cardiovascular diseases and stroke burden in rural communities of developing countries. Int J Cardiol. 2013;168:3123-4.
- [Google Scholar]
- Implications and expectancies of the “Atahualpa Project”: A population-based survey designed to reduce the burden of stroke and cardiovascular diseases in rural Ecuador. J Neurosci Rural Pract. 2013;4:363-5.
- [Google Scholar]






